Abstract
Objective:
To identify differences in amount and distribution of fat and lean soft tissue in a cross-sectional study of subjects with and without type 2 diabetes and to determine whether any differences are affected by race/ethnicity or sex.
Design and methods:
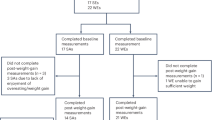
Overweight and obese (body mass index, BMI⩾25 kg m−2) Black, White and Hispanic men (490) and women (825) with type 2 diabetes ((mean±s.d.) age 58.5±6.6; BMI 35.3±5.3) who had a baseline dual energy X-ray absorptiometry whole-body scan at the time of enrollment in the Look AHEAD clinical trial, and 242 healthy controls, 91 males and 151 females (age 55.3±8.6 years, BMI 30.7±4.2 kg m−2) who were participating in unrelated research and were scanned on the same densitometers.
Results:
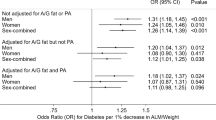
Adjusted for gender, age, race, clinical site and body size, total fat mass was smaller in persons with type 2 diabetes than in controls (−1.4±0.3 (s.e.); 34.5 vs 35.8 kg, P<0.001) while trunk fat was larger (1.3±0.2 (s.e.); 19.9 vs 18.6 kg, P<0.001) and leg fat was smaller (−1.5±0.2 (s.e.); 10.7 vs 12.3 kg, P<0.001). The arms of subjects with type 2 diabetes did not have significantly less fat compared to controls. Adjusted trunk lean mass was larger in type 2 diabetes by 0.6 kg (28.4 vs 27.8 kg, P<0.001) while leg lean was smaller by 0.5 kg (18.1 vs 18.6 kg, P<0.001).
Conclusions:
Type 2 diabetes is associated with less total fat, leg fat and leg lean mass and more truncal fat and lean mass than controls. The physiological processes producing these deviations in tissue distribution and their metabolic significance warrant further investigation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others

References
Cnop M, Landchild MJ, Vidal J, Havel PJ, Knowles NG, Carr DR et al. The concurrent accumulation of intra-abdominal and subcutaneous fat explains the association between insulin resistance and plasma leptin concentrations: distinct metabolic effects of two fat compartments. Diabetes 2002; 51: 1005–1015.
Wagenknecht LE, Langefeld CD, Scherzinger AL, Norris JM, Haffner SM, Saad MF et al. Insulin sensitivity, insulin secretion, and abdominal fat: the Insulin Resistance Atherosclerosis Study (IRAS) Family Study. Diabetes 2003; 52: 2490–2496.
Utzschneider KM, Carr DB, Hull RL, Kodama K, Shofer JB, Retzlaff BM et al. Impact of intra-abdominal fat and age on insulin sensitivity and beta-cell function. Diabetes 2004; 53: 2867–2872.
Kuk JL, Katzmarzyk PT, Nichaman MZ, Church TS, Blair SN, Ross R . Visceral fat is an independent predictor of all-cause mortality in men. Obesity 2006; 14: 336–341.
Svendsen OL, Hassager C . Body composition and fat distribution measured by dual-energy X-ray absorptiometry in premenopausal and postmenopausal insulin-dependent and non-insulin-dependent diabetes mellitus patients. Metabolism 1998; 47: 212–216.
Maiolo C, Mohamed EI, Di DN, Pepe M, Perriello G, De LA . Body composition and pulmonary function in obese type 2 diabetic women. Diabetes Nutr Metab 2002; 15: 20–25.
Poynten AM, Markovic TP, Maclean EL, Furler SM, Freund J, Chisholm DJ et al. Fat oxidation, body composition and insulin sensitivity in diabetic and normoglycaemic obese adults 5 years after weight loss. Int J Obes 2003; 27: 1212–1218.
Goodpaster BH, Krishnaswami S, Resnick H, Kelley DE, Haggerty C, Harris TB et al. Association between regional adipose tissue distribution and both type 2 diabetes and impaired glucose tolerance in elderly men and women. Diabetes Care 2003; 26: 372–379.
Bavenholm PN, Kuhl J, Pigon J, Saha AK, Ruderman NB, Efendic S . Insulin resistance in type 2 diabetes: association with truncal obesity, impaired fitness, and atypical malonyl coenzyme A regulation. J Clin Endocrinol Metab 2003; 88: 82–87.
Stoney RM, Ireland PD, Walker KZ, Giles GG, Best JD, O’Dea K . Do postmenopausal women with NIDDM have a reduced capacity to deposit and conserve lower-body fat? Diabetes Care 1998; 21: 828–830.
Tafeit E, Möller R, Peiber TR, Sudi K, Reibnegger G . Differences of subcutaneous adipose tissue topography in type-2 diabetic (NIDDM) women and healthy controls. Am J Phys Anthropol 2000; 113: 381–388.
Terry RB, Stefanick ML, Haskell WL, Wood PD . Contributions of regional adipose tissue depots to plasma lipoprotein concentrations in overweight men and women: possible protective effects of thigh fat. Metabolism 1991; 40: 733–740.
Kahn HS, Austin H, Williamson DF, Arensberg D . Simple anthropometric indices associated with ischemic heart disease. J Clin Epidemiol 1996; 49: 1017–1024.
Williams MJ, Hunter GR, Kekes-Szabo T, Snyder S, Treuth MS . Regional fat distribution in women and risk of cardiovascular disease. Am J Clin Nutr 1997; 65: 855–860.
Snijder MB, Dekker JM, Visser M, Bouter LM, Stehouwer CD, Yudkin JS et al. Trunk fat and leg fat have independent and opposite associations with fasting and postload glucose levels: the Hoorn study. Diabetes Care 2004; 27: 372–377.
Snijder MB, Henry RM, Visser M, Dekker JM, Seidell JC, Ferreira I et al. Regional body composition as a determinant of arterial stiffness in the elderly: The Hoorn Study. J Hypertens 2004; 22: 2339–2347.
Ryan DH, Espeland MA, Foster GD, Haffner SM, Hubbard VS, Johnson KC et al. Look AHEAD (Action for Health in Diabetes): design and methods for a clinical trial of weight loss for the prevention of cardiovascular disease in type 2 diabetes. Control Clin Trials 2003; 24: 610–628.
Kronmal RA . Spurious correlation and the fallacy of the ratio standard revisited. J R Statist Soc A 1993; 156 (Part 3): 379–392.
Zhu S, Wang Z, Shen W, Heymsfield SB, Heshka S . Percentage body fat ranges associated with metabolic syndrome risk: results based on the third National Health and Nutrition Examination Survey (1988–1994). Am J Clin Nutr 2003; 78: 228–235.
Han TS, Feskens EJ, Lean ME, Seidell JC . Associations of body composition with type 2 diabetes mellitus. Diabet Med 1998; 15: 129–135.
Chang CJ, Wu CH, Lu FH, Wu JS, Chiu NT, Yao WJ . Discriminating glucose tolerance status by regions of interest of dual-energy X-ray absorptiometry. Clinical implications of body fat distribution. Diabetes Care 1999; 22: 1938–1943.
Ferreira I, Snijder MB, Twisk JW, van Mechelen W, Kemper HC, Seidell JC et al. Central fat mass versus peripheral fat and lean mass: opposite (adverse versus favorable) associations with arterial stiffness? The Amsterdam Growth and Health Longitudinal Study. J Clin Endocrinol Metab 2004; 89: 2632–2639.
Snijder MB, Visser M, Dekker JM, Goodpaster BH, Harris TB, Kritchevsky SB et al. Low subcutaneous thigh fat is a risk factor for unfavourable glucose and lipid levels, independently of high abdominal fat. The Health ABC Study. Diabetologia 2005; 48: 301–308.
Hofbauer LC, Brueck CC, Singh SK, Dobnig H . Osteoporosis in patients with diabetes mellitus. J Bone Miner Res 2007; 22: 1317–1328.
Strotmeyer ES, Cauley JA, Schwartz AV, Nevitt MC, Resnick HE, Zmuda JM et al. Diabetes is associated independently of body composition with BMD and bone volume in older white and black men and women: The Health, Aging, and Body Composition Study. J Bone Miner Res 2004; 19: 1084–1091.
Christensen JO, Svendsen OL . Bone mineral in pre- and postmenopausal women with insulin-dependent and non-insulin-dependent diabetes mellitus. Osteoporos Int 1999; 10: 307–311.
Okuno Y, Nishizawa Y, Sekiya K, Hagiwara S, Miki T, Morii H . Total and regional bone mineral content in patients with non-insulin dependent diabetes mellitus. J Nutr Sci Vitaminol (Tokyo) 1991; 37 (Suppl): S43–S49.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Heshka, S., Ruggiero, A., Bray, G. et al. Altered body composition in type 2 diabetes mellitus. Int J Obes 32, 780–787 (2008). https://doi.org/10.1038/sj.ijo.0803802
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sj.ijo.0803802
Keywords
This article is cited by
-
A cohort study on the predictive capability of body composition for diabetes mellitus using machine learning
Journal of Diabetes & Metabolic Disorders (2023)
-
The visceral fat area to leg muscle mass ratio is significantly associated with the risk of hyperuricemia among women: a cross-sectional study
Biology of Sex Differences (2021)
-
The Association between Body Composition using Dual energy X-ray Absorptiometry and Type-2 Diabetes: A Systematic Review and Meta-Analysis of Observational studies
Scientific Reports (2019)
-
Falls and Fractures in Diabetes—More than Bone Fragility
Current Osteoporosis Reports (2019)
-
Insulin does not rescue cortical and trabecular bone loss in type 2 diabetic Goto-Kakizaki rats
The Journal of Physiological Sciences (2018)