Abstract
Objective
To compare, in patients with cancer and in healthy subjects, measured resting energy expenditure (REE) from traditional indirect calorimetry to a new portable device (MedGem™) and predicted REE.
Design
Cross-sectional clinical validation study.
Setting
Private radiation oncology centre, Brisbane, Australia.
Subjects
Cancer patients (n=18) and healthy subjects (n=17) aged 37–86 y, with body mass indices ranging from 18 to 42 kg/m2.
Interventions
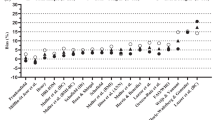
Oxygen consumption (VO2) and REE were measured by VMax229 (VM) and MedGem (MG) indirect calorimeters in random order after a 12-h fast and 30-min rest. REE was also calculated from the MG without adjustment for nitrogen excretion (MGN) and estimated from Harris–Benedict prediction equations. Data were analysed using the Bland and Altman approach, based on a clinically acceptable difference between methods of 5%.
Results
The mean bias (MGN–VM) was 10% and limits of agreement were –42 to 21% for cancer patients; mean bias −5% with limits of −45 to 35% for healthy subjects. Less than half of the cancer patients (n=7, 46.7%) and only a third (n=5, 33.3%) of healthy subjects had measured REE by MGN within clinically acceptable limits of VM. Predicted REE showed a mean bias (HB–VM) of −5% for cancer patients and 4% for healthy subjects, with limits of agreement of −30 to 20% and −27 to 34%, respectively.
Conclusions
Limits of agreement for the MG and Harris Benedict equations compared to traditional indirect calorimetry were similar but wide, indicating poor clinical accuracy for determining the REE of individual cancer patients and healthy subjects.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Barak N, Wall-Alonso E & Sitrin MD (2002): Evaluation of stress factors and body weight adjustments currently used to estimate energy expenditure in hospitalized patients. J. Parenter. Enteral. Nutr. 26, 231–238.
Bauer J, Reeves MM & Capra S (2004): The agreement between measured and predicted resting energy expenditure in patients with pancreatic cancer—a pilot study. JOP. J. Pancreas (Online) 5, 32–40.
Bland JM & Altman DG (1986): Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1, 307–310.
Branson RD (1990): The measurement of energy expenditure: instrumentation, practical considerations, and clinical application. Respir. Care 35, 640–659.
Bursztein S, Saphar P, Singer P & Elwyn DH (1989): A mathematical analysis of indirect calorimetry measurements in acutely ill patients. Am. J. Clin. Nutr. 50, 227–230.
Daly JM, Heymsfield SB, Head CA, Harvey LP, Nixon DW, Katzeff H & Grossman GD (1985): Human energy requirements: overestimation by widely used prediction equation. Am. J. Clin. Nutr. 42, 1170–1174.
Demark-Wahnefried W, Peterson BL, Winer EP, Marks L, Aziz N, Marcom PK, Blackwell K & Rimer BK (2001): Changes in weight, body composition, and factors influencing energy balance among premenopausal breast cancer patients receiving adjuvant chemotherapy. J. Clin. Oncol. 19, 2381–2389.
Falconer JS, Fearon KC, Plester CE, Ross JA & Carter DC (1994): Cytokines, the acute-phase response, and resting energy expenditure in cachectic patients with pancreatic cancer. Ann. Surg. 219, 325–331.
Fearon KC, Hansell DT, Preston T, Plumb JA, Davies J, Shapiro D, Shenkin A, Calman KC & Burns HJ (1988): Influence of whole body protein turnover rate on resting energy expenditure in patients with cancer. Cancer Res. 48, 2590–2595.
Feurer ID & Mullen JL (1986): Bedside measurement of resting energy expenditure and respiratory quotient via indirect calorimetry. Nutr. Clin. Pract. 1, 43–49.
Flancbaum L, Choban PS, Sambucco S, Verducci J & Burge JC (1999): Comparison of indirect calorimetry, the Fick method, and prediction equations in estimating the energy requirements of critically ill patients. Am. J. Clin. Nutr. 69, 461–466.
Garby L & Lammert O (1984): Within-subjects between-days-and-weeks variation in energy expenditure at rest. Hum. Nutr. Clin. Nutr. 38, 395–397.
Glynn CC, Greene GW, Winkler MF & Albina JE (1999): Predictive versus measured energy expenditure using limits-of-agreement analysis in hospitalized, obese patients. J. Parenter. Enteral. Nutr. 23, 147–154.
Hamwi GJ (1964): Therapy: changing dietary concepts. In: Diabetes Mellitus: Diagnosis and Treatment, ed. Danowski TS, Vol. 1, pp 73–78. New York, American Diabetes Association.
Hansell DT, Davies JW & Burns HJ (1986): The relationship between resting energy expenditure and weight loss in benign and malignant disease. Ann. Surg. 203, 240–245.
Harris JA & Benedict FG (1919): A Biometric Study of Basal Metabolism in Man. Washington DC: Carnegie Institution of Washington.
HealtheTech (2002): MedGem:Operator's Manual. Golden, CO: HealtheTech Inc.
Henry CJ, Hayter J & Rees DG (1989): The constancy of basal metabolic rate in free-living male subjects. Eur. J. Clin. Nutr. 43, 727–731.
Heymsfield SB (2002): Heat and life: the ongoing scientific odyssey. J. Parenter. Enteral. Nutr. 26, 319–332.
Jequier E & Schutz Y (1983): Long-term measurements of energy expenditure in humans using a respiration chamber. Am. J. Clin. Nutr. 38, 989–998.
Leenders KL (1994): PET: blood flow and oxygen consumption in brain tumors. J. Neurooncol. 22, 269–273.
McClave SA, Lowen CC, Kleber MJ, McConnell JW, Jung LY & Goldsmith LJ (2003a): Clinical use of the respiratory quotient obtained from indirect calorimetry. J. Parenter. Enteral. Nutr. 27, 21–26.
McClave SA, Spain DA, Skolnick JL, Lowen CC, Kieber MJ, Wickerham PS, Vogt JR & Looney SW (2003b): Achievement of steady state optimizes results when performing indirect calorimetry. J. Parenter. Enteral. Nutr. 27, 16–20.
McLean JA & Tobin G (1987): Animal and Human Calorimetry. Cambridge: Cambridge University Press.
Nieman DC, Trone GA & Austin MD (2003): A new handheld device for measuring resting metabolic rate and oxygen consumption. J. Am. Dietet. Assoc. 103, 588–592.
Platz EA (2002): Energy imbalance and prostate cancer. J. Nutr. 132, 3471S–3481S.
Reeves MM & Capra S (2003): Predicting energy requirements in the clinical setting: are current methods evidence based? Nutr. Rev. 61, 143–151.
Reeves MM, Davies PSW, Bauer J & Battistutta D (2004): Reducing the time period of steady state does not affect the accuracy of energy expenditure measurements by indirect calorimetry. J. Appl. Physiol. 97, 130–134.
Segal K (1987): Comparison of indirect calorimetric measurements of resting energy expenditure with a ventilated hood, face mask, and mouthpiece. Am. J. Clin. Nutr. 45, 1420–1423.
Siervo M, Boschi V & Falconi C (2003): Which REE prediction equation should we use in normal-weight, overweight and obese women? Clin. Nutr. 22, 193–204.
Soares MJ, Sheela ML, Kurpad AV, Kulkarni RN & Shetty PS (1989): The influence of different methods on basal metabolic rate measurements in human subjects. Am. J. Clin. Nutr. 50, 731–736.
Soares MJ & Shetty PS (1986): Intra-individual variations in resting metabolic rates of human subjects. Hum. Nutr. Clin. Nutr. 40, 365–369.
Taaffe DR, Thompson J, Butterfield G & Marcus R (1995): Accuracy of equations to predict basal metabolic rate in older women. J. Am. Diet. Assoc. 95, 1387–1392.
Toth MJ (1999): Energy expenditure in wasting diseases: current concepts and measurement techniques. Curr. Opin. Clin. Nutr. Metab. Care. 2, 445–451.
Weir JB DeV (1949): New methods for calculating metabolic rate with special reference to protein metabolism. J. Physiol. 109, 1–9.
Weissman C, Askanazi J, Milic-Emili J & Kinney JM (1984): Effect of respiratory apparatus on respiration. J. Appl. Physiol. 57, 475–480.
Author information
Authors and Affiliations
Corresponding author
Additional information
Guarantor: M Reeves.
Contributors: MMR was responsible for writing the manuscript, initiated and designed the study, carried out data collection, data analysis, interpretation and discussion of results. SC initiated the study and assisted in the design of the study. JB contributed to the study design and assisted with data collection. PSWD and DB contributed to the study design, data analysis, interpretation and discussion of results and manuscript preparation.
Rights and permissions
About this article
Cite this article
Reeves, M., Capra, S., Bauer, J. et al. Clinical accuracy of the MedGem™ indirect calorimeter for measuring resting energy expenditure in cancer patients. Eur J Clin Nutr 59, 603–610 (2005). https://doi.org/10.1038/sj.ejcn.1602114
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sj.ejcn.1602114
Keywords
This article is cited by
-
Assessing resting energy expenditure in overweight and obese adolescents in a clinical setting: validity of a handheld indirect calorimeter
Pediatric Research (2017)
-
Key determinants of energy expenditure in cancer and implications for clinical practice
European Journal of Clinical Nutrition (2016)
-
Estimating resting energy expenditure in patients requiring nutritional support: a survey of dietetic practice
European Journal of Clinical Nutrition (2008)
-
MedGem Hand-Held Indirect Calorimeter Is Valid for Resting Energy Expenditure Measurement in Healthy Children*
Obesity (2006)
-
Comparison between Medgem and Deltatrac resting metabolic rate measurements
European Journal of Clinical Nutrition (2005)