Abstract
Study design:
Case report.
Setting:
Temple University Children's Medical Center in USA.
Objectives:
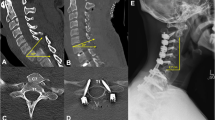
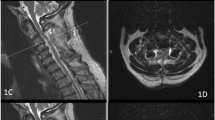
To report a patient whose recurrent and transient episodes of quadriplegia mimicked cervical cord neurapraxia. Cervical spine neuroimaging revealed congenital intersegmental fusion of C5 through C7 (consistent with Klippel–Feil anomaly), corresponding abnormal spinal cord signals on T2-weighted images and enhancing focal lesion opposite the C4 vertebral body. A posterior cervical decompression at C4–C5 and lateral mass fixation was performed, and the episodic quadriplegia has not recurred.
Conclusion:
Understanding of the biomechanics of Klippel–Feil anomaly may facilitate prompt referral for surgical management and avoidance of permanent disability.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Goetz CG . Textbook of Clinical Neurology, 2nd edn, Copyright © 2003 Saunders, an Imprint of Elsevier: Philadelphia, pp 578–579.
Behrman RE . Nelson Textbook of Pediatrics, 17th edn, Copyright © 2004 Saunders, an Imprint of Elsevier: Philadelphia, p 2289.
Torg JS et al. Cervical cord neurapraxia: classification, pathomechanics, morbidity, and management guidelines. J Neurosurg 1997; 87: 843–850.
Nagib MG, Maxwell RE, Chou SN . Identification and management of high-risk patients with Klippel–Feil syndrome. J Neurosurg 1984; 61: 523–530.
Silva MR, Chiamolera MI, Kasamatsu TS, Cerutti JM, Maciel RM . Thyrotoxic hypokalemic periodic paralysis, an endocrine emergency: clinical and genetic features in 25 patients. Arq Bras Endocrinol Metab 2004; 48: 196–215.
Torg JS et al. The pathomechanics and pathophysiology of cervical spinal cord injury. Clin Orthop 1995; 321: 259–269.
Pizzutillo PD, Woods M, Nicholson L, MacEwen GD . Risk factors in Klippel–Feil syndrome. Spine 1994; 19: 2110–2116.
Dickerman RD, Colle KO, Mittler MA . Intramedullary inflammatory mass dorsal to the Klippel–Feil deformity: error in development or response to an abnormal motion segment? Spinal Cord 2004; 42: 720–722.
Hensinger RN, Lang JE, MacEwen GD . Klippel–Feil syndrome; a constellation of associated anomalies. J Bone Joint Surg Am 1974; 56: 1246–1253.
Rouvreau P, Glorion C, Langlais J, Noury H, Pouliquen JC . Assessment and neurologic involvement of patients with cervical spine congenital synostosis as in Klippel–Feil syndrome: study of 19 cases. J Pediatr Orthop B 1998; 7: 179–185.
Vaidyanathan S, Hughes PL, Soni BM, Singh G, Sett P . Klippel–Feil syndrome – the risk of cervical spinal cord injury. BMC Fam Pract 2002; 3: 6.
Nagashima H, Morio Y, Teshima R . No neurological involvement for more than 40 years in Klippel–Feil syndrome with severe hypermobility of the upper cervical spine. Arch Orthop Trauma Surg 2001; 121: 99–101.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Gupta, S., Piatt, J. & Belay, B. Cervical spinal cord neurapraxia in the setting of Klippel–Feil anomaly: a diagnostic and therapeutic challenge. Spinal Cord 45, 637–640 (2007). https://doi.org/10.1038/sj.sc.3101999
Published:
Issue date:
DOI: https://doi.org/10.1038/sj.sc.3101999