Key Points
-
During the first six weeks of treatment, the occlusal surface of the splint made no significant contribution to any of the outcomes measured suggesting that the occlusion is a relatively unimportant factor influencing recovery in the majority of TMD patients seen in practice.
-
A small proportion of patients needed treatment for up to five months to obtain a satisfactory response. These were the patients who crossed over from the non-occluding control splint to the stabilising splint. They tended to be older with TMJ clicking.
-
Clicking was not especially responsive to treatment with the stabilising splint, but discomfort was reduced in three quarters of patients with clicking TMJs. It was difficult to make a reliable diagnosis of disc displacement with reduction using the trial criteria.
-
Suitably trained and interested GDPs can manage four out of five TMD patients in general practice; a link with specialist services is recommended to deal with non-responding patients.
Abstract
Introduction Little is known about how effective general dental practitioners (GDPs) are in treating temporomandibular disorders (TMD). The overall aim of this study was to compare the lower stabilising splint (SS) with a non-occluding control (CS) for the management of TMD in general dental practice.
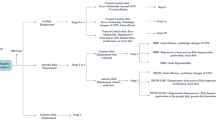
Method A total of 93 TMD patients attending 11 GDPs were randomly allocated to SS or CS. Diagnosis was according to International Headache Society Criteria. Outcome criteria included pain visual analogue scale (VAS), number of tender muscles, aggregate joint tenderness, inter-incisal opening, TMJ clicks and headaches. Splints were fitted one week after baseline and patients were followed-up every three weeks to three months; those not responding to CS after six weeks (< 50% VAS reduction) were crossed over to SS for a further three months.
Results Documentation was returned from nine GDPs for 72 patients (38 for SS, 34 for CS). At six weeks, mean improvements were noted for all outcome criteria, but less so for clicking. There were no significant differences between splints [χ2]. Seventeen CS patients had < 50% VAS reduction and were provided with SS in the cross-over group. CS patients with >50% VAS reduction were significantly younger than CS patients who crossed-over (ANOVA, p=0.009) and had significantly less diagnoses of TMJ clicking (χ2, p<0.05). At the conclusion of the trial 16 patients were referred for specialist management: 11 non-responders (< 50% VAS reduction), one of whom needed occlusal adjustment and five responders also needing occlusal adjustment.
Conclusions At six weeks SS gave similar relief to CS for all outcome criteria. Patients who crossed-over from CS to SS were more likely to be older and have clicking TMJs. At the end of treatment nine of 11 non-responders to SS had a diagnosis of disc displacement with reduction. However, 80% TMD patients were managed effectively by GDPs using splints for periods of up to five months
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Dworkin SF, LeResche L . Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord 1992; 6: 301–355.
Oleson J . Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalgia. Olso: Norwegian University Press, 1988.
American Academy of Craniomandibular Disorders. In: McNeill C. (ed.) Craniomandibular disorders: guidelines for evaluation, diagnosis and management. Chicago: Quintessence, 1990.
Forssell H, Kalso E, Koskela P, Vehmanen R, Puukka P, Alanen P . Occlusal treatments in temporomandibular disorders: a qualitative systematic review of randomized controlled trials. Pain 1999; 83: 549–560.
Okeson JP . Management of temporomandibular disorders and occlusion. 4th Edition. St Louis: Mosby, 1998. pp. 474–487.
Dao TT, Lavigne GJ, Charbonneau A, Feine JS, Lund JP . The efficacy of oral splints in the treatment of myofascial pain of the jaw muscles: a controlled clinical trial. Pain 1994; 56: 85–94.
Rubinoff MS, Gross A, McCall WD, Jr . Conventional and nonoccluding splint therapy compared for patients with myofascial pain dysfunction syndrome. Gen Dent 1987; 35: 502–506.
Ekberg EC, Vallon D, Nilner M . Occlusal appliance therapy in patients with temporomandibular disorders. A double-blind controlled study in a short-term perspective. Acta Odontol Scand 1998; 56: 122–128.
Nichols WP, Dookun R . Research in general practice—the germination of an idea. Br Dent J 1998; 185: 220–222.
Steele JG, Nohl FS, Wassell RW . Crowns and other extra-coronal restorations: occlusal considerations and articulator selection. Br Dent J 2002; 192: 377–380, 383–387.
Okeson JP . Management of temporomandibular disorders and occlusion. 4th Edition ed. St Louis: Mosby, 1998. pp. 357–358.
Major PW, Nebbe B . Use and effectiveness of splint appliance therapy: review of literature. Cranio 1997; 15: 159–166.
Feine JS, Lund JP . An assessment of the efficacy of physical therapy and physical modalities for the control of chronic musculoskeletal pain. Pain 1997; 71: 5–23.
Santacatterina A, Paoli M, Peretta R, Bambace A, Beltrame A . A comparison between horizontal splint and repositioning splint in the treatment of 'disc dislocation with reduction'. Literature meta-analysis. J Oral Rehabil 1998; 25: 81–88.
Gray RJM, Davies SJ, Quayle AA . A clinical approach to temporomandibular disorders: 6 Splint therapy. Br Dent J 1994; 170: 135–142.
Dworkin SF, Huggins KH, Wilson L, Mancl L, Turner J, Massoth D et al. A randomized clinical trial using research diagnostic criteria for temporomandibular disorders-axis II to target clinic cases for a tailored self-care TMD treatment program. J Orofac Pain 2002; 16: 48–63.
Acknowledgements
The authors would like to thank the British Dental Association Research Foundation for sponsoring this project through the Shirley Glasstone Hughes Memorial Prize. In particular the authors are deeply indebted to Professor Jack Rowe for his wise counsel and encouragement during the application process. Pivotal to the success of this study was the commitment of the nine dentists: Bill Nichols, Nigel Adams, Roy Dookun, Doris Canning, Malcolm Howat, Joan Davidson, Phil Dixon, Mike Atkinson and Rob Wain. The essential roles of study coordinator, secretary, group convenor and group librarian assumed by Dr Adams, Dr Davidson, Dr Howat and Dr Nichols respectively. Drs Adams and Wassell presented initial trial results at IADR, Seattle 1999 and Drs Nichols and Wassell presented further follow-up at the British Prosthodontic Conference, London 1999. The group is grateful to Mr Michael Adair, of David Bird Dental Ceramics, who made all of the splints.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Wassell, R., Adams, N. & Kelly, P. Treatment of temporomandibular disorders by stabilising splints in general dental practice: results after initial treatment. Br Dent J 197, 35–41 (2004). https://doi.org/10.1038/sj.bdj.4811420
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sj.bdj.4811420
This article is cited by
-
Quantitative and qualitative condylar changes following stabilization splint therapy in patients with temporomandibular joint disorders
Clinical Oral Investigations (2023)
-
Centric relation and increasing the occlusal vertical dimension: concepts and clinical techniques - part two
British Dental Journal (2021)
-
Efficacy of Appliance Therapy on Temporomandibular Disorder Related Facial Pain and Mandibular Mobility: A Randomized Controlled Study
The Journal of Indian Prosthodontic Society (2014)
-
Retrospective examination of the healthcare 'journey' of chronic orofacial pain patients referred to oral and maxillofacial surgery
British Dental Journal (2013)
-
'Management is a black art' – professional ideologies with respect to temporomandibular disorders
British Dental Journal (2007)