Key Points
-
Systematic reviews of implementation trials in medicine have shown that implementation strategies are not effective under all circumstances and few studies have investigated their effectiveness in dentistry.
-
There is a need to find effective and cost effective implementation strategies to optimise the integration of evidence into current dental practice.
-
In this sample of Scottish general dental practitioners' adherence to the SIGN Guideline of the management of impacted and unerupted third molars was high.
-
There is no simple answer to getting research evidence into practice.
Abstract
Objective To investigate the effectiveness and cost-effectiveness of different guideline implementation strategies, using the Scottish Intercollegiate Guidelines Network (SIGN) Guideline 42 'Management of unerupted and impacted third molar teeth' (published 2000) as a model.
Design A pragmatic, cluster RCT (2×2 factorial design).
Subjects Sixty-three dental practices across Scotland. Clinical records of all 16—24-year-old patients over two, four-month periods in 1999 (pre-intervention) and 2000 (post-intervention) were searched by a clinical researcher blind to the intervention group. Data were also gathered on the costs of the interventions.
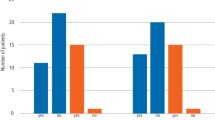
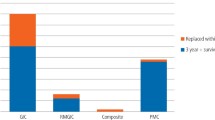
Interventions Group 1 received a copy of SIGN 42 Guideline and had an opportunity to attend a postgraduate education course (PGEC). In addition to this, group 2 received audit and feedback (A and F). Group 3 received a computer aided learning (CAL) package. Group 4 received A and F and CAL.
Principal outcome measurement The proportion of patients whose treatment complied with the guideline.
Results The weighted t-test for A and F versus no A and F (P=0.62) and CAL versus no CAL (P=0.76) were not statistically significant. Given the effectiveness results (no difference) the cost effectiveness calculation became a cost-minimisation calculation. The minimum cost intervention in the trial consisted of providing general dental practitioners (GDPs) with guidelines and the option of attending PGEC courses. Routine data which subsequently became available showed a Scotland-wide fall in extractions prior to data collection.
Conclusion In an environment in which pre-intervention compliance was unexpectedly high, neither CAL nor A and F increased the dentists' compliance with the SIGN guideline compared with mailing of the guideline and the opportunity to attend a postgraduate course. The cost of the CAL arm of the trial was greater than the A and F arm. Further work is required to understand dental professionals' behaviour in response to guideline implementation strategies.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
NHS. A first class service: quality in the new NHS. England: NHS 1998.
Richards D, Lawrence A . Evidence-based dentistry. Br Dent J 1995; 179: 270–273.
Scottish Home and Health Department. Clinical guidelines. Edinburgh, 1993.
Davidoff F, Haynes B, Sackett D, Smith R . Evidence-based medicine. Br Med J 1995; 310: 1085–1086.
McGlone P, Watt R, Sheiham A . Evidence-based dentistry: an overview of the challenges in changing professional practice. Br Dental J 2001; 190: 636–639.
Institute for Medicine Committee on Clinical Practice Guidelines. Guidelines for clinical practice: from development to use. National Academy Press: Washington DC, USA, 1992.
Grimshaw JM, Russell IT . Effect of clinical guidelines on medical practice: A systemic review of rigorous evaluations. Lancet 1993; 342: 1317–1322.
Effective Health Care Bulletin. Implementing clinical guidelines: can guidelines be used to improve clinical practice. York: University of York, 1994; 8, 1–12.
Lomas J . Words without action? The production, dissemination, and impact of consensus recommendations. Ann Rev Public Health. 1991; 12: 41–65.
Getting evidence into practice. Effective Health Care Bulletin 1999; 5: 1.
Feder G, Eccles M, Grol R, Griffiths C, Grimshaw J . Using clinical guidelines. Br Med J 1999; 318: 728–730.
Bero LA, Grilli R, Grimshaw JM, Harvey E, Oxman AD, Thomson MA . Getting research finding into practice: closing the gap between research and practice: an overview of systemic reviews of interventions to promote the implementation of research findings. Br Med J 1998; 317: 465–468.
Oxman A . No magic bullets: a systematic review of 102 trials of interventions to help health care professionals deliver services more effectively or efficiently. Can Med Assoc J 1995; 153: 1423–1431.
O'Brien K, Wright J, Conboy F, et al. The effect of orthodontic referral guidelines: a randomised controlled trial. Br Dent J 2000; 188: 392–397.
Goodey RD, Brickley MR, Hill CM, Shepherd JP . A controlled trial of three referral methods for patients with third molars. Br Dent J 2000; 189: 556–560.
Kay EJ, Silkstone B, Worthington HV . Evaluation of computer aided learning in developing clinical decision-making skills. Br Dent J 2001; 190: 554–557.
Scottish Intercollegiate Guidelines Network (SIGN). Management of unerupted and impacted third molar teeth, a National Clinical Guideline. SIGN 2000.
Carmichael FA, McGowan DA . Incidence of nerve damage following third molar removal: A West of Scotland Oral Surgery Research Group Study. Br J Oral Maxillofac Surg 1992; 30: 78–82.
Blackburn CW, Bramley PA . Lingual nerve damage associated with the removal of lower third molars. Br Dent J 1989; 167: 103–106.
Chiapasco M, De Cicco L, Marrone G . Side effects and complications associated with third molar surgery. Oral Surg Oral Med Oral Pathol 1993; 76: 412–420.
Effectiveness Matters: Prophylactic removal of impacted third molars: is it justified? The Centre for Reviews and Dissemination, University of York, 1998; 3: issue 2.
Sadler A, Davidson M, Houpis C, Watt-Smith S . Specialist practice for minor oral surgery: a comparative audit of third molar surgery. Br Dent J 1993; 174: 273–277.
Dental Practice Board Annual Report. Scottish Dental Practice Board, Trinity Park House, Edinburgh, 1997.
Brickley MR, Shepherd JP . An investigation of the rationality of lower third molar removal, based on USA National Institutes of Health criteria. Br Dent J 1996; 180: 249–254.
Grimshaw J, Campbell M, Eccles M, Steen N . Experimental and quasi-experimental designs for evaluating guideline implementation strategies. Family prac 2000; 17 (suppl): 1–16.
Deery C, Fyffe HE, Nuttall NM, Nugent ZJ, Pitts NB . The dental caries status of Scottish adolescents reported to be regular attenders. Initial results from a primary dental care based research network. Br Dent J 1999; 187: 95–99.
Bonetti D, Johnston M, Pitts NB, Deery C, Ricketts I, Bahrami M, Ramsay, Johnston J . Can psychological models bridge the gap between clinical guidelines and clinicians' behaviour: a randomised controlled trial of an intervention to influence intention to implement evidence-based practice. Br Dent J 2003; 195: 403–407.
Bland J, Kerry S . Statistical Notes: Weighted comparison of means. Br Med J 1998: 316: 129.
NHS management information and dental accounting system (MIDAS), Practitioner services division, Edinburgh.
Grimshaw JM, Freemantle N, Langhorne P, Song F . Complexity and systemic reviews. Report to the US Congress of Technology Assessment. Office of Technology Assessment, Washingon DC, 1995.
Eccles M, Steen N, Grimshaw J, Thomas L, McNamee P, Soutter J, Wilsdon J, Matowe L, Needham G, Gilbert F, et al. Effect of audit and feedback, and reminder messages on primary-care radiology referrals: a randomised trial. Lancet 2001; 357: 1406–1409.
Lands D . The relationship between dental health and variations in the level of third molar removals experienced by populations. Community Dent Health 1998; 15: 67–71.
Song F, Landes D, Glenny A-M, Sheldon TA . Prophylactic removal of impacted third molars: an assessment of published reviews. Br Dent J 1997; 182: 339–346.
Daley T . Third molar prophylactic extraction: a review and analysis of the literature. Gen Dent J 1996; 44: 310–320.
Mercier P, Precious D . Risks and benefits of removal of impacted third molars. J Oral Maxillofac Surg 1992; 21: 17–27.
Edwards SJL, Lilford RJ, Braunholtz DA, et al. Ethics of randomised trials. In Black N, Braizier J, Fitzpatrick R, Reeves B: Health services research methods. A guide to best practice. pp 98–107, London: BMJ publication, 1998.
NICE Guidance to the NHS on the removal of wisdom teeth. National Institute for Clinical Excellence. NICE Ref 2000/003a. 2000.
Acknowledgements
The authors would like to thank:
Professor Graham Ogden, Dundee Dental Hospital and School, University of Dundee, for help with the development of the CAL Package and the postgraduate courses.
For additional statistical advice, Marion Campbell of the Health Services Research Unit (HSRU), University of Aberdeen.
Professor Jeremy Grimshaw, Ottawa Health Research Institute, Canada (formerly HSRU) and Professor Trevor Sheldon, University of York for methodological advice.
Elaine Humphries, Audit Facilitator, NHS Education for Scotland for her support and Dr James Rennie Dental Director of NHS Education Scotland for his intellectual input into the study.
The following General Dental Practitioners assisted with the development of the CAL package. Dr Iain Hunter, Dr Andrew Wright, Dr Jim McCafferty, Dr Colin Yule.
We would also like to thank everyone involved in the study, particularly Marilyn Laird, jenny Johnson, Louise Cardno and the participating dental practices.
This project was supported by Scottish Executive's Chief Scientists Office and NHS R&D Programme (Trial R2-64). The Dental Health Services Research Unit is core funded by the Chief Scientist Office of the Scottish Executive Health Department. The views expressed are those of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Bahrami, M., Deery, C., Clarkson, J. et al. Effectiveness of strategies to disseminate and implement clinical guidelines for the management of impacted and unerupted third molars in primary dental care, a cluster randomised controlled trial. Br Dent J 197, 691–696 (2004). https://doi.org/10.1038/sj.bdj.4811858
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sj.bdj.4811858
This article is cited by
-
What maximizes the effectiveness and implementation of technology-based interventions to support healthcare professional practice? A systematic literature review
BMC Medical Informatics and Decision Making (2018)
-
Evaluating the impact of caries prevention and management by caries risk assessment guidelines on clinical practice in a dental teaching hospital
BMC Oral Health (2016)
-
Practice change toward better adherence to evidence-based treatment of early dental decay in the National Dental PBRN
Implementation Science (2014)
-
A systematic review of the use of theory in randomized controlled trials of audit and feedback
Implementation Science (2013)
-
Audit and feedback had small but potentially important improvements in professional practice
Evidence-Based Dentistry (2013)