Key Points
-
Mandibular repositioning splints can be used to treat the symptoms of sleep-related breathing disorders with high rates of compliance and highly positive reported treatment outcome.
-
Much of the suffering caused by sleep-related breathing disorders is borne by the sleeping partner.
-
The majority of patients experience only mild, reversible side effects during MRS therapy.
Abstract
Aim To determine in detail the complications associated with the use of mandibular repositioning splints (MRS) to treat sleep-related breathing disorders.
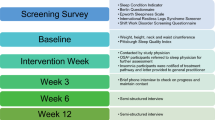
Method This prospective cross-sectional cohort study audits the management with mandibular repositioning splints of 121 patients suffering from sleep-related breathing disorders. Investigation of patients' and sleeping partners' perspectives on treatment was undertaken with the use of a questionnaire based study.
Results Sixty-eight per cent of respondents reported that they were compliant with treatment; various side effects were reported of which excess salivation was the most common. Investigation of sleeping partners' perspectives revealed that 70% felt that their partners' snoring was improved and 47% felt that their partner's breathing pauses during sleep were reduced. Sixty-four per cent of the sleeping partners also reported that their own sleep pattern had improved since their partner's treatment.
Conclusion Mandibular repositioning splints used in the manner described by this paper are demonstrated to have a good compliance rate, provide successful treatment and exhibit only minor, reversible side effects.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Battagel J . Obstructive sleep apnoea: Fact not fiction. Br Dent J 1996; 23: 315–324.
Guilleminault C . Obstructive sleep apnoea. The clinical syndrome and historical perspective. Med Clin N Am 1985; 69: 6.
Young TM, Dempsey J, Skatrud J, et al. The occurrence of sleep disordered breathing among middle-aged adults. New Eng J Med 1993; 328: 1230–1235.
Semple SJG, Gibson GJ . Sleep apnoea and related conditions. JRCP 1993; 27: 363–364.
Terran-Santos J . The association between sleep apnoea and the risk of traffic accidents. New Engl J Med 1999; 340: 847–851.
Taylor JF . Medical aspects of fitness to drive: a guide for medical practitioners. Medical Commission on Accident Prevention. London: HMSO, 1995.
Robin P . Glossoptosis due to atresia and hypertrophy of the mandible. Am J Dis Child 1934; 48: 541–547.
Johns MW . A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep 1991; 14: 540–545.
SAS version 8. © 2002 SAS Institute, SAS Campus Drive, Cary, North Carolina 27513, USA.
Schmidt-Nowara W, Lowe A, Wiegand L . An American Sleep Disorders Association review. Oral appliances for the treatment of snoring and obstructive sleep apnoea: a review. Sleep 1995; 8: 501–510.
Johal A, Battagel JM . Current principles in the management of obstructive sleep apnoea with mandibular advancement appliances. Br Dent J 2001; 190: 532–536.
Shadaba A, Battagel JM, Owa A, et al. Evaluation of the Herbst mandibular advancement splint in the management of patients with sleep related breathing disorders. Clin Otolaryngol 2000; 25: 404–412.
Johnston CD, Gleadhill IC, Cinnamond MJ . Mandibular advancement appliances and obstructive sleep apnoea: a randomized clinical trial. EJO 2002; 24: 251–262.
McGown AD, Makker HK, Battagel JM, L'Estrange PR . Long-term use of mandibular advancement splints for snoring and obstructive sleep apnoea: a questionnaire survey. E Resp J 2001; 17: 462–466.
Grunstein RR . Nasal Continuous Positive Airway Pressure treatment for obstructive sleep apnoea. Thorax 1995; 50: 1106–1111.
Clark GT, Arand D, Chung E, Tong D . Effect of anterior mandibular positioning on obstructive sleep apnoea. Am Rev Respir Dis 1993; 147: 624–629.
Mehta A, Qin J, Petocz P, et al. A randomized, controlled study of a mandibular advancement splint for obstructive sleep apnoea. AJRCCM 2001; 163: 1457–1461.
Sullivan CE, Issa FG, Berthon-Jones M, Eves L . Reversal of obstructive sleep apnoea by Continuous Positive Airway Pressure applied through the nares. Lancet 1981; 1: 862–865.
Engleman HM, McDonald JP, Graham D et al. Randomized crossover trial of two treatments for sleep apnoea/hypopnoea syndrome. Continuous Positive Airway Pressure and mandibular repositioning splint. AJRCCM 2002; 166: 855–859.
Wilhelmsson B, Tegelberg A, Walker-Engstrom ML et al. A prospective randomised study of a dental appliance compared with uvulopalatopharyngoplasty in the treatment of obstructive sleep apnoea. Acta Oto-Laryng 1999; 119: 503–509.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Bates, C., McDonald, J. Patients' and sleeping partners' experience of treatment for sleep-related breathing disorders with a mandibular repositioning splint. Br Dent J 200, 95–101 (2006). https://doi.org/10.1038/sj.bdj.4813149
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sj.bdj.4813149
This article is cited by
-
Factors associated with treatment adherence to mandibular advancement devices: a scoping review
Sleep and Breathing (2023)
-
Obstructive sleep apnoea and the role of the dental team
British Dental Journal (2020)
-
Mandibular exercises improve mandibular advancement device therapy for obstructive sleep apnea
Sleep and Breathing (2011)
-
Are general dental practitioners effective in the management of non-apnoeic snoring using mandibular advancement appliances?
British Dental Journal (2009)
-
Review of oral appliances for treatment of sleep-disordered breathing
Sleep and Breathing (2007)