Abstract
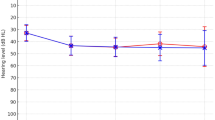
Molecular diagnosis makes a substantial contribution to precise diagnosis, subclassification, prognosis, and selection of therapy. Mutations in the PDS (SLC26A4) gene are known to be responsible for both Pendred syndrome and nonsyndromic hearing loss associated with enlarged vestibular aqueduct, and the molecular confirmation of the PDS gene has become important in the diagnosis of these conditions. In the present study, PDS mutation analysis confirmed that PDS mutations were present and significantly responsible in 90% of Pendred families, and in 78.1% of families with nonsyndromic hearing loss associated with enlarged vestibular aqueduct. Furthermore, variable phenotypic expression by the same combination of mutations indicated that these two conditions are part of a continuous category of disease. Interestingly, the PDS mutation spectrum in Japanese, including the seven novel mutations revealed by this study, is very different from that found in Caucasians. Of the novel mutations detected, 53% were the H723R mutation, suggesting a possible founder effect. Ethnic background is therefore presumably important and should be noted when genetic testing is being performed. The PDS gene mutation spectrum in Japanese may be representative of those in Eastern Asian populations and its elucidation is expected to facilitate the molecular diagnosis of a variety of diseases.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Pendred V : Deaf mutism and goitre. Lancet 2 1896; 532.
Fraser GR : Association of congenital deafness with goitre (Pendred's syndrome): a study of 207 families. Ann Hum Genet 1965; 28: 411–422.
Reardon W, Coffey R, Phelps PD et al: Pendred syndrome: 100 years of underascertainment? Q J Med 1997; 90: 443–447.
Everett LA, Glaser B, Beck JC et al: Pendred syndrome is caused by mutations in a putative sulphate transporter gene (PDS). Nat Genet 1997; 17: 411–422.
Usami S, Abe S, Weston MD et al: Non-syndromic hearing loss associated with enlarged vestibular aqueduct is caused by PDS mutations. Hum Genet 1999; 104: 188–192.
Valvassori GE, Clemis JD : The large vestibular aqueduct syndrome. Laryngoscope 1978; 88: 723–728.
Abe S, Usami S, Shinkawa H : Three familial cases of hearing loss associated with enlargement of the vestibular aqueduct. Ann Otol Rhinol Laryngol 1997; 106: 1063–1069.
Campbell C, Cucci RA, Prasad S et al: Pendred syndrome, DFNB4, and PDS/SLC26A4: identification of eight novel mutations and possible genotype–phenotype correlations. Hum Mutat 2001; 17: 403–411.
Lopez-Bigas N, Melchionda S, de Cid R et al: Identification of five new mutations of PDS/SLC26A4 in Mediterranean families with hearing impairment. Hum Mutat 2002; 18: 548.
Kopp P, Arseven OK, Sabacan L et al: Phenocopies for deafness and goiter development in a large inbred Brazilian kindred with Pendred's syndrome associated with a novel mutation in the PDS gene. J Clin Endocrinol Metab 1999; 84: 336–341.
Coyle B, Reardon W, Herbrick JA et al: Molecular analysis of the PDS gene in Pendred syndrome. Hum Mol Genet 1998; 7: 1105–1112.
Reardon W, O Mahoney CF, Trembath R et al: Enlarged vestibular aqueduct: a radiological marker of Pendred syndrome, and mutation of the PDS gene. Q J Med 2000; 93: 99–104.
Van Hauwe P, Everett LA, Coucke P et al: Two frequent missense mutations in Pendred syndrome. Hum Mol Genet 1998; 7: 1099–1104.
Lopez-Bigas N, Rabionet R, de Cid R et al: Splice-site mutation in the PDS gene may result in intrafamilial variability for deafness in Pendred syndrome. Hum Mutat 1999; 14: 520–526.
Adato A, Raskin L, Petit C et al: Deafness heterogeneity in a Druze isolate from the Middle East: novel OTOF and PDS mutations, low prevalence of GJB2 35delG mutation and indication for a new DFNB locus. Eur J Hum Genet 2000; 8: 437–442.
Park HJ, Shaukat S, Liu XZ et al: Origins and frequencies of SLC26A4 (PDS) mutations in east and south Asians: global implications for the epidemiology of deafness. J Med Genet 2003; 40: 242–248.
Coucke PJ, Van Hauwe P, Everett LA et al: Identification of two different mutations in the PDS gene in an inbred family with Pendred syndrome. J Med Genet 1999; 36: 475–477.
Yong AM, Goh SS, Zhao Y et al: Two Chinese families with Pendred's syndrome: radiological imaging of the ear and molecular analysis of the pendrin gene. J Clin Endocrinol Metab 2001; 86: 3907–3911.
Scott DA, Wang R, Kreman TM : Functional differences of the PDS gene product are associated with phenotypic variation in patients with Pendred syndrome and non-syndromic hearing loss (DFNB4). Hum Mol Genet 2000; 9: 1709–1715.
Li XC, Everett LA, Lalwani AK et al: A mutation in PDS causes non-syndromic recessive deafness. Nat Genet 1998; 18: 215–217.
Bogazzi F, Raggi F, Ultimieri F et al: A novel mutation in the pendrin gene associated with Pendred's syndrome. Clin Endocrinol (Oxf) 2000; 52: 279–285.
Namba A, Abe S, Shinkawa H et al: Genetic features of hearing loss associated with ear anomalies: PDS and EYA1 mutation analysis. J Hum Genet 2001; 46: 518–521.
Fugazzola L, Mannavola D, Cerutti N et al: Molecular analysis of the Pendred's syndrome gene and magnetic resonance imaging studies of the inner ear are essential for the diagnosis of true Pendred's syndrome. J Clin Endocrinol Metab 2000; 85: 2469–2475.
Phelps PD, Coffey RA, Trembath RC et al: Radiological malformations of the ear in Pendred syndrome. Clin Radiol 1998; 53: 268–2273.
Kitamura K, Takahashi K, Noguchi Y et al: Mutations of the Pendred syndrome gene (PDS) in patients with large vestibular aqueduct. Acta Otolaryngol 2000; 120: 137–141.
Van Laer L, Coucke P, Mueller RF et al: A common founder for the 35delG GJB2 gene mutation in connexin 26 hearing impairment. J Med Genet 2001; 38: 515–518.
Ohtsuka A, Yuge I, Kimura S et al: GJB2 deafness gene shows a specific spectrum of mutations in Japan, including a frequent founder mutation. Hum Genet 2003; 112: 329–333.
Royaux IE, Wall SM, Karniski LP et al: Pendrin, encoded by the Pendred syndrome gene, resides in the apical region of renal intercalated cells and mediates bicarbonate secretion. Proc Natl Acad Sci USA 2001; 98: 4221–4226.
Scott DA, Wang R, Kreman TM et al: The Pendred syndrome gene encodes a chloride–iodide transport protein. Nat Genet 1999; 2: 440–443.
Ishinaga H, Shimizu T, Yuta A et al: Pendred's syndrome with goiter and enlarged vestibular aqueducts diagnosed by PDS gene mutation. Head Neck 2002; 24: 710–713.
Masmoudi S, Charfedine I, Hmani M et al: Pendred syndrome: phenotypic variability in two families carrying the same PDS missense mutation. Am J Med Genet 2000; 90: 38–44.
Hulander M, Kiernan AE, Blomqvist SR et al: Lack of pendrin expression leads to deafness and expansion of the endolymphatic compartment in inner ears of Foxi1 null mutant mice. Development 2003; 130: 2013–2025.
Acknowledgements
We thank all the subjects who participated in the present project. We also thank Dr Kyoko Nagai (Gunma University School of Medicine), Dr Satoshi Iwasaki (Hamamatsu University School of Medicine), Dr Tatsuo Matsunaga (International University of Health and Welfare), Drs Noriko Minami and Yumiko Hosoya (Iwate Medical University), Drs Hajime Ishinaga and Atsushi Yuta (Mie University), Dr Tetsuya Tono (Miyazaki Medical College), Dr Yukihiko Kanda (Nagasaki University School of Medicine), Dr Hitoshi Sato (Niigata University School of Medicine), Drs Tatsuhiko Harada and Ryuichi Osanai (Saitama Medical School), Drs Hitome Kobayashi and Yasuya Nomura (Showa University), and Dr Tatsuya Yamasoba (Tokyo University) for sending the samples of their patients. This work was supported by the Ministry of Health and Welfare, Japan (SU), and a Grant-in-Aid for Scientific Research from the Ministry of Education, Science and Culture of Japan (SU).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsukamoto, K., Suzuki, H., Harada, D. et al. Distribution and frequencies of PDS (SLC26A4) mutations in Pendred syndrome and nonsyndromic hearing loss associated with enlarged vestibular aqueduct: a unique spectrum of mutations in Japanese. Eur J Hum Genet 11, 916–922 (2003). https://doi.org/10.1038/sj.ejhg.5201073
Published:
Issue date:
DOI: https://doi.org/10.1038/sj.ejhg.5201073
Keywords
This article is cited by
-
Comparison of vestibular function in hereditary hearing loss patients with GJB2, CDH23, and SLC26A4 variants
Scientific Reports (2024)
-
Enlarged vestibular aqueduct and Mondini Malformation: audiological, clinical, radiologic and genetic features
European Archives of Oto-Rhino-Laryngology (2021)
-
A novel genotyping technique for discriminating LVAS-associated high-frequency variants in SLC26A4 gene
AMB Express (2020)
-
Comprehensive genetic testing of Chinese SNHL patients and variants interpretation using ACMG guidelines and ethnically matched normal controls
European Journal of Human Genetics (2020)
-
Next-generation sequencing-based mutation analysis of genes associated with enlarged vestibular aqueduct in Chinese families
European Archives of Oto-Rhino-Laryngology (2020)