Abstract
Data sources
The Cochrane Oral Health Group's Trials Register, the Cochrane Central Register of Controlled Trials (CENTRAL), Medline, Embase, CINAHL, LILACS, Chinese Biomedical Literature Database, China National Knowledge Infrastructure, Wan Fang Database, OpenGrey and ClinicalTrials.gov databases were searched. Reference lists of identified articles were also scanned for relevant papers. There were no language restrictions.
Study selection
Randomised controlled trials (RCTs) evaluating OHC in the form of mouthwashes, swabs, toothbrushing or in combination in critically ill patients receiving mechanical ventilation were included.
Data extraction and synthesis
Data extraction was carried out independently by two reviewers. Study authors were contracted for additional information. Random-effects meta-analyses were performed where data could be pooled.
Results
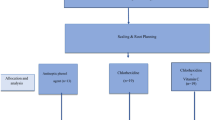
Thirty-five RCTs (5374 participants) were included. Five trials (14%) were assessed at low risk of bias, 17 studies (49%) were at high risk of bias and 13 studies (37%) were assessed at unclear risk of bias in at least one domain. There were four main comparisons; chlorhexidine (CHX mouthrinse or gel) versus placebo/usual care, toothbrushing versus no toothbrushing, powered versus manual toothbrushing and comparisons of oral care solutions.
Seventeen RCTs (2402 participants, two at high, 11 at unclear and four at low risk of bias) provide moderate quality evidence that CHX mouthrinse or gel, as part of OHC, compared to placebo or usual care is associated with a reduction in VAP (OR 0.60, 95% confidence intervals (CI) 0.47 to 0.77, P < 0.001, I2 = 21%) A number needed to treat (NNT) of 15 (95% CI 10 to 34). There is no evidence of a difference between CHX and placebo/usual care in the outcomes of mortality, duration of mechanical ventilation or duration of ICU stay. There was insufficient evidence to determine whether there is a difference between CHX and placebo/usual care in the outcomes of duration of use of systemic antibiotics, oral health indices, microbiological cultures, caregivers' preferences or cost. Only three studies reported any adverse effects, and these were mild with similar frequency in CHX and control groups.
Three trials in children found no evidence of a difference between OHC with CHX and placebo, and there was insufficient evidence to determine the effect of other outcomes. Four RCTs (828 participants, low quality evidence) compared to OHC without toothbrushing (± CHX), and for the outcome of VAP no evidence of a difference was found (OR 0.69, 95% CI 0.36 to 1.29, P = 0.24, I2 = 64%). There was insufficient evidence to determine the effect of other outcomes.
Only one trial compared use of a powered toothbrush with a manual toothbrush, providing insufficient evidence to determine the effect on any of the outcomes of this review.
A range of other oral care solutions were compared. There is some weak evidence that povidone iodine mouthrinse is more effective than saline in reducing VAP (OR 0.35, 95% CI 0.19 to 0.65, P = 0.0009, I2 = 53%) (two studies, 206 participants, high risk of bias). Due to the variation in comparisons and outcomes among the trials in this group there is insufficient evidence concerning the effects of other oral care solutions on the outcomes of this review.
Conclusions
Effective OHC is important for ventilated patients in intensive care. OHC that includes either chlorhexidine mouthwash or gel is associated with a 40% reduction in the odds of developing ventilator-associated pneumonia in critically ill adults. However, there is no evidence of a difference in the outcomes of mortality, duration of mechanical ventilation or duration of ICU stay. There is no evidence that OHC including both CHX and toothbrushing is different from OHC with CHX alone, and some weak evidence to suggest that povidone iodine mouthrinse is more effective than saline in reducing VAP. There is insufficient evidence to determine whether powered toothbrushing or other oral care solutions are effective in reducing VAP.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Alhazzani W, Smith O, Muscedere J, Medd J, Cook D . Toothbrushing for critically ill mechanically ventilated patients: a systematic review and meta-analysis of randomized trials evaluating ventilator-associated pneumonia. Crit Care Med 2013; 41: 646–655. doi: 10.1097/CCM.0b013e3182742d45. Review. PubMed PMID: 23263588.
Pineda LA, Saliba RG, El Solh AA . Effect of oral decontamination with chlorhexidine on the incidence of nosocomial pneumonia: a meta-analysis. Crit Care 2006; 10: R35.
Labeau SO, Van de Vyver K, Brusselaers N, Vogelaers D, Blot SI . Prevention of ventilator-associated pneumonia with oral antiseptics: a systematic review and meta-analysis. Lancet Infect Dis 2011; 11: 845–854.
Bekaert M, Timsit JF, Vansteelandt S, et al. Attributable mortality of ventilator-associated pneumonia: a reappraisal using causal analysis. Am J Respir Crit Care Med 2011; 184: 1133–1139.
Author information
Authors and Affiliations
Additional information
Address for correspondence: Luisa Fernandez Mauleffinch, Review Group Co-ordinator, Cochrane Oral Health Group, MANDEC, School of Dentistry, University of Manchester, Higher Cambridge Street, Manchester, M15 6FH, UK. E-mail: luisa.fernandez@manchester.ac.uk
Shi Z, Xie H, Wang P, et al. Oral hygiene care for critically ill patients to prevent ventilator-associated pneumonia. Cochrane Database Syst Rev 2013; Issue 8. Art. No.: CD008367. DOI: 10.1002/14651858.CD008367.pub2.
This paper is based on a Cochrane Review published in the Cochrane Library 2013, issue 8 (see www.thecochranelibrary.com for information). Cochrane Reviews are regularly updated as new evidence emerges and in response to feedback, and the Cochrane Library should be consulted for the most recent version of the review.
Rights and permissions
About this article
Cite this article
Richards, D. Oral hygiene regimes for mechanically ventilated patients that use chlorhexidine reduce ventilator-associated pneumonia. Evid Based Dent 14, 91–92 (2013). https://doi.org/10.1038/sj.ebd.6400957
Published:
Issue date:
DOI: https://doi.org/10.1038/sj.ebd.6400957