Abstract
Aim:
To reinvestigate the characteristics of reserpine-induced gastric mucosal lesions (GMLs).
Methods:
The GML-inducing effect of reserpine and the time-course of recovery from reserpine-induced GMLs were examined in Sprague-Dawley (SD) rats. The GML-inducing and blood pressure-decreasing effects of Compound Hypotensive Tablets (CHTs) were investigated in spontaneously hypertensive rats (SHRs). Intracerebroventricular (icv) injection and vagotomy were performed to verify the central vagal mechanism in reserpine-induced GMLs.
Results:
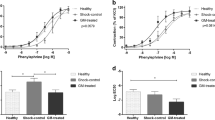
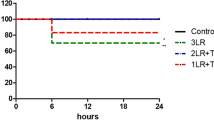
Single intraperitoneal (ip) injections of reserpine (0.25, 0.5, 1, 2, 4, and 6 mg/kg) dose-dependently induced GMLs in SD rats. Both single and repeated (2 weeks) oral administrations of reserpine led to slight GMLs at doses of 24 mg/kg and 10 mg/kg, respectively. Blood pressure was significantly decreased in SHRs after 2 months of CHT administration (0.01 and 0.03 mg/kg; doses were expressed as the amount of reserpine in the CHT). CHT doses of 0.3 mg/kg induced GMLs, but 0.1 mg/kg did not. Examining the time course of recovery from GMLs, severe GMLs occurred 18 h after ip reserpine (4 mg/kg), obviously lessened at 1 week and healed spontaneously at 3 weeks. Intracerebroventricular injections of reserpine caused GMLs at much lower doses (0.08 and 0.4 mg/kg), and reserpine-induced GMLs were greatly inhibited by vagotomy, suggesting the involvement of a central vagal mechanism.
Conclusion:
Reserpine-induced GMLs were dose-dependent, and the lesions healed spontaneously within 3 weeks. Long-term treatment with CHT at doses adequate to decrease blood pressure will not induce GMLs. A central vagal mechanism was involved in reserpine-induced GMLs.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Jia Q, Liu LP, Wang YJ . Stroke in China. Clin Exp Pharmacol Physiol 2010; 37: 259–64.
Luepker RV, Arnett DK, Jacobs DR Jr, Duval SJ, Folsom AR, Armstrong C, et al. Trends in blood pressure, hypertension control, and stroke mortality: the Minnesota Heart Survey. Am J Med 2006; 119: 42–9.
Bansal D, Chahoud G, Smith ES, Mehta JL . Prevention of heart failure. Curr Opin Cardiol 2006; 21: 510–6.
Tocci G, Sciarretta S, Volpe M . Development of heart failure in recent hypertension trials. J Hypertens 2008; 26: 1477–86.
Zoungas S, Asmar RP . Arterial stiffness and cardiovascular outcome. Clin Exp Pharmacol Physiol 2007; 34: 647–51.
Neal B, MacMahon S, Chapman N . Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomized trials. Lancet 2000; 356: 1955–64.
Sheldon MB, Kotte JH . Effect of rauwolfia serpentina and reserpine on the blood pressure in essential hypertension: a long-term double-blind study. Circulation 1957; 16: 200–6.
Finnerty FA Jr, Kakaviatos N, Chupkovich V . Value of chlorthalidone plus reserpine in moderately severe and severe hypertension: a two-year study. Circulation 1965; 32: 13–8.
Dillon D, Swain JM . Gastro-intestinal hemorrhage as a complication of reserpine administration: report of two cases. Am J Psychiatry 1956; 113: 462–3.
Locket S . Oral preparations of Reuwolfia serpentina in treatment of essential hypertension. Br Med J 1955; 1: 809–16.
Bulpitt CJ, Dollery CT . Side effects of hypotensive agents evaluated by a self administered questionnaire. Br Med J 1973; 3: 485–90.
Sandor V, Cuparencu B . Analysis of the mechanism of the protective activity of some sympathomimetic amines in experimental ulcers. Pharmacology 1977; 15: 208–17.
Yamaguchi Y, Hirio J, Puke H, Kumada S . Mechanism of gastric secretagogue effect of reserpine in rats. J Pharmacol Exp Ther 1978; 205: 710–7.
Kim KS, Shore PA . Mechanism of action of reserpine and insulin on gastric amines and gastric acid secretion, and the effect of monoamine oxidase inhibition. J Pharmacol Exp Ther 1963; 141: 321–5.
Gamberini MT, Skorupa LA, Souccar C, Lapa AJ . Inhibition of gastric secretion by a water extract from Baccharis triptera, Mart. Mem Inst Oswaldo Cruz 1991; 86 Suppl 2: 137–9.
Ma XJ, Shen FM, Liu AJ, Shi KY, Wu YL, Su DF . Clonidine, moxonidine, folic acid, and mecobalamin improve baroreflex function in stroke-prone, spontaneously hypertensive rats. Acta Pharmacol Sin 2007; 28: 1550–8.
Zheng RM, Zou CJ, Zhu SG . p38 MAPK mediates cardiovascular and behavioral responses induced by central IL-1 beta and footshock in conscious rats. Acta Pharmacol Sin 2004; 25: 266–70.
Li HL, Kang YM, Yu L, Xu HY, Zhao H . Melatonin reduces blood pressure in rats with stress-induced hypertension via GABAA receptors. Clin Exp Pharmacol Physiol 2009; 36: 436–40.
Yalcin M, Aydin C . Cardiovascular effects of centrally administered arachidonic acid in haemorrhage-induced hypotensive rats: investigation of a peripheral mechanism. Clin Exp Pharmacol Physiol 2009; 36: 447–53.
Wang JL, Wang L, Wu ZT, Yuan WJ, Su DF, Ni X, et al. Low dose of moxonidine within the rostral ventrolateral medulla improves the baroreflex sensitivity control of sympathetic activity in hypertensive rat. Acta Pharmacol Sin 2009; 30: 1594–600.
Onoma M, Yogo K, Ozaki K, Kamei K, Akima M, Koga H, et al. Oral mitemcinal (GM-611), an erythromycin-derived prokinetic, accelerates normal and experimentally delayed gastric emptying in conscious dogs. Clin Exp Pharmacol Physiol 2008; 35: 35–42.
Wang XQ, Zhang HG, Cheng YQ, Li XH . Inhibition of left ventricular remodelling in spontaneously hypertensive rats by G alpha q-protein carboxyl terminus imitation polypeptide GCIP-27 is not entirely dependent on blood pressure. Clin Exp Pharmacol Physiol 2008; 35: 1215–21.
Krug S, Zhang Y, Mori TA, Croft KD, Vickers JJ, Langton LK, et al. N-Acetylcysteine prevents but does not reverse dexamethasone-induced hypertension. Clin Exp Pharmacol Physiol 2008; 35: 979–81.
Acknowledgements
This study was supported by grants from the National Science and Technology Major Project (No 2009ZX09303-002), the China Postdoctoral Science Foundation Funded Project (No 20080441303) and the Shanghai Postdoctoral Sustentation Fund (No 08R214101).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Ma, Xj., Lu, Gc., Song, Sw. et al. The features of reserpine-induced gastric mucosal lesions. Acta Pharmacol Sin 31, 938–943 (2010). https://doi.org/10.1038/aps.2010.74
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/aps.2010.74
Keywords
This article is cited by
-
Impact of depositional environment and diagenesis on the Upper Triassic Xujiahe tight-sand reservoir in Guang’an area, Central Sichuan Basin, SW China
Carbonates and Evaporites (2019)
-
Characteristics of the tight sand reservoirs in the delta front in the Xu-2 Member of the Upper Triassic Xujiahe Formation (Hechuan area of the central Sichuan Basin, SW China)
Arabian Journal of Geosciences (2018)