Abstract
Aim:
Gefitinib is effective in only approximately 20% of patients with non-small-cell lung cancer (NSCLC), and the underlying mechanism remains unclear. FoxM1 is upregulated in NSCLC and associated with a poor prognosis in NSCLC patients. In this study, we examined the possible role of FoxM1 in gefitinib resistance and the related mechanisms.
Methods:
Gefitinib resistant human lung adenocarcinoma cell line SPC-A-1 and gefitinib-sensitive human lung mucoepidermoid carcinoma cell line NCI-H292 were used. mRNA and protein expression of FoxM1 and other factors were tested with quantitative RT PCR and Western blot analysis. RNA interference was performed to suppress FoxM1 expression in SPC-A-1 cells, and lentiviral infection was used to overexpress FoxM1 in H292 cells. MTT assay and flow cytometry were used to examine the proliferation and apoptosis of the cells.
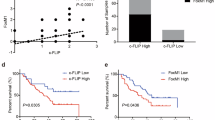
Results:
Treatment of SPC-A-1 cells with gefitinib (1 and 10 μmol/L) upregulated the expression of FoxM1 in time- and concentration-dependent manners, while gefitinib (1 μmol/L) downregulated in H292 cells. In SPC-A-1 cells treated with gefitinib (1 μmol/L), the expression of several downstream targets of FoxM1, including survivin, cyclin B1, SKP2, PLK1, Aurora B kinase and CDC25B, were significantly upregulated. Overexpression of FoxM1 increased the resistance in H292 cells, while attenuated FoxM1 expression restored the sensitivity to gefitinib in SPC-A-1 cells by inhibiting proliferation and inducing apoptosis.
Conclusion:
The results suggest that FoxM1 plays an important role in the resistance of NSCLC cells to gefitinib in vitro. FoxM1 could be used as a therapeutic target to overcome the resistance to gefitinib.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Elzagallaai AA, Garcia-Bournissen F, Finkelstein Y, Bend JR, Rieder MJ, Koren G . Severe bullous hypersensitivity reactions after exposure to carbamazepine in a HAN-Chinese child with a positive HLA-B*1502 and negative in vitro toxicity assays: evidence for different pathophysiological mechanisms. J Popul Ther Clin Pharmacol 2011; 18: e1–9.
Raychaudhuri P . FoxM1: a master regulator of tumor metastasis. Cancer Res 2011; 71: 4329–33.
Sun H, Teng M, Liu J, Jin D, Wu J, Yan D, et al. FOXM1 expression predicts the prognosis in hepatocellular carcinoma patients after orthotopic liver transplantation combined with the Milan criteria. Cancer Lett 2011; 306: 214–22.
Yu J, Deshmukh H, Payton JE, Dunham C, Scheithauer BW, Tihan T, et al. Array-based comparative genomic hybridization identifies CDK4 and FOXM1 alterations as independent predictors of survival in malignant peripheral nerve sheath tumor. Clin Cancer Res 2011; 17: 1924–34.
Balli D, Zhang Y, Snyder J, Kalinichenko VV, Kalin TV . Endothelial cell-specific deletion of transcription factor FoxM1 increases urethane-induced lung carcinogenesis. Cancer Res 2011; 71: 40–50.
Wang X, Kiyokawa H, Dennewitz MB, Costa RH . The forkhead box m1b transcription factor is essential for hepatocyte DNA replication and mitosis during mouse liver regeneration. Proc Natl Acad Sci U S A 2002; 99: 16881–6.
Wang IC, Chen YJ, Hughes D, Petrovic V, Major ML, Park HJ, et al. Forkhead box M1 regulates the transcriptional network of genes essential for mitotic progression and genes encoding the SCF (SKP2-1) ubiquitin ligase. Mol Cell Biol 2005; 25: 10875–94.
aoukili J, Kooistra MR, Brás A, Kauw J, Kerkhoven RM, Morrison A, et al. FoxM1 is required for execution of the mitotic rogramme and chromosome stability. Nat Cell Biol 2005; 7: 126–36.
Wonsey DR, Follettie MT . Loss of the forkhead transcription factor FoxM1 causes centrosome amplification and mitotic catastrophe. Cancer Res 2005; 65: 5181–9.
lin TV, Wang IC, Ackerson TJ, Major ML, Detrisac CJ, Kalinichenko VV, et al. Increased levels of the FoxM1 transcription factor accelerate development and progression of prostate carcinamas in both TRAMP and LADY transgenic mice. Cancer Res 2006; 66: 1712–20.
Kim IM, Ackerson T, Ramakrishna S, Tretiakova M, Wang IC, Kalin TV, et al. The Forkhead Box m1 transcription factor stimulates the proliferation of tumor cells during development of lung cancer. Cancer Res 2006; 66: 2153–61.
Le XF, Pruefer F . Bast RC Jr . HER2-targeting antibodies modulate the cyclin-dependent kinase inhibitor p27Kip1 via multiple signaling pathways. Cell Cycle 2005; 4: 87–95.
Wakeling AE . Epidermal growth factor receptor tyrosine kinase inhibitors. Curr Opin Pharmacol 2002; 2: 382–7.
F Ciardiello . Epidermal growth factor receptor inhibitors in cancer treatment. Future Onclo 2005; 1: 221–34.
Nelson MH, Dolder CR . Lapatinib: a novel dual tyrosine kinase inhibitor with activity in solid tumors. Ann Pharmacother 2006; 40: 261–9.
Wakeling AE, Guy SP, Woodburn JR, Ashton SE, Curry BJ, Barker AJ, et al. ZD1839 (Iressa): an orally active inhibitor of epidermal growth factor signaling with potential for cancer therapy. Cancer Res 2002; 62: 5749–54.
Hay N . The Akt-mTOR tango and its relevance to cancer. Cancer Cell 2005; 8: 179–83.
Morgillo F, Lee HY . Resistance to epidermal growth factor receptor-targeted therapy. Drug Resist Update 2005; 8: 298–310.
Jia D, Yan M, Wang X, Hao X, Liang L, Liu L, et al. Development of a highly metastatic model that reveals a crucial role of fibronectin in lung cancer cell migration and invasion. BMC Cancer 2010; 10: 364–75.
Macha MA, Matta A, Chauhan S, Siu KM, Ralhan R . 14-3-3 zeta is a molecular target in guggulsterone induced apoptosis in head and neck cancer cells. BMC Cancer 2010; 10: 655–66.
Zheng Y, Ritzenthaler JD, Roman J, Han S . Nicotine stimulates human lung cancer cell growth by inducing fibronectin expression. Am J Respir Cell Mol Biol 2007; 37: 681–90.
Uchida A, Hirano S, Kitao H, Ogino A, Rai K, Toyooka S, et al. Activation of downstream epidermal growth factor receptor (EGFR) signaling provides efitinibresistance in cells carrying EGFR mutation. Cancer Sci 2007; 98: 357–63.
Laoukili J, Stahl M, Medema RH . FoxM1: at the crossroads of ageing and cancer. Biochim Biophys Acta 2007; 1775: 92–102.
Myatt SS, Lam EW . The emerging roles of forkhead box (Fox) proteins in cancer. Nat Rev Cancer 2007; 7: 847–59.
Kwok JM, Peck B, Monteiro LJ, Schwenen HD, Millour J, Coombes RC, et al. FOXM1 confers acquired cisplatin resistance in breast cancer cells. Mol Cancer Res 2010; 8: 24–34.
Carr JR, Park HJ, Wang Z, Kiefer MM, Raychaudhuri P . FoxM1 mediates resistance to Herceptin and Paclitaxel. Cancer Res 2010; 70: 5054–63.
McGovern UB, Francis RE, Peck B, Guest SK, Wang J, Myatt SS, et al. Gefitinib (Iressa) represses FOXM1 expression via FOXO3a in breast cancer. Mol Cancer Ther 2009; 8: 582–91.
Estève PO, Chin HG, Pradhan S . Molecular mechanisms of transactivation and doxorubicin-mediated repression of survivin gene in cancer cells. J Biol Chem 2007; 282: 2615–25.
Androic I, Krämer A, Yan R, Rödel F, Gätje R, Kaufmann M, et al. Targeting cyclin B1 inhibits proliferation and sensitizes breast cancer cells to taxol. BMC Cancer 2008; 8: 391.
Rödel F, Hoffmann J, Distel L, Herrmann M, Noisternig T, Papadopoulos T, et al. Survivin as a radioresistance factor, and prognostic and therapeutic target for radiotherapy in rectal cancer. Cancer Res 2005; 65: 4881–7.
Kato J, Kuwabara Y, Mitani M, Shinoda N, Sato A, Toyama T, et al. Expression of survivin in esophageal cancer: correlation with the prognosis and response to chemotherapy. Int J Cancer 2001; 95: 92–5.
Zaffaroni N, Pennati M, Colella G, Perego P, Supino R, Gatti L, et al. Expression of the anti-apoptotic gene survivin correlates with taxol resistance in human ovarian cancer. Cell Mol Life Sci 2002; 59: 1406–12.
Suzuki T, Urano T, Miki Y, Moriya T, Akahira J, Ishida T, et al. Nuclear cyclin B1 in human breast carcinoma as a potent prognostic factor. Cancer Sci 2007; 98: 644–51.
Hassan KA, Ang KK, El-Naggar AK, Story MD, Lee JI, Liu D, et al. Cyclin B1 overexpression and resistance to radiotherapy in head and neck squamous cell carcinama. Cancer Res 2002; 62: 6414–17.
Thatcher N, Chang A, Parikh P, Rodrigues Pereira J, Ciuleanu T, von Pawel J, et al. Gefitinib plus best supportive care in previously treated patients with refractory advanced non-small-cell lung cancer: results from a randomised, placebo-controlled, multicentre study (Iressa Survival Evaluation in Lung Cancer). Lancet 2005; 366: 1527–37.
Acknowledgements
This work was supported by the Shanghai Leading Academic Discipline Project (No B115) and China National “985” Project (phase III).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Xu, N., Zhang, X., Wang, X. et al. FoxM1 mediated resistance to gefitinib in non-smallcell lung cancer cells. Acta Pharmacol Sin 33, 675–681 (2012). https://doi.org/10.1038/aps.2011.188
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/aps.2011.188
Keywords
This article is cited by
-
GPC3 affects the prognosis of lung adenocarcinoma and lung squamous cell carcinoma
BMC Pulmonary Medicine (2021)
-
Deregulation of extracellular matrix modeling with molecular prognostic markers revealed by transcriptome sequencing and validations in Oral Tongue squamous cell carcinoma
Scientific Reports (2021)
-
CHD4 mediates proliferation and migration of non-small cell lung cancer via the RhoA/ROCK pathway by regulating PHF5A
BMC Cancer (2020)
-
The multifaceted roles of FOXM1 in pulmonary disease
Cell Communication and Signaling (2019)
-
GLRX inhibition enhances the effects of geftinib in EGFR-TKI-resistant NSCLC cells through FoxM1 signaling pathway
Journal of Cancer Research and Clinical Oncology (2019)