Abstract
Aim:
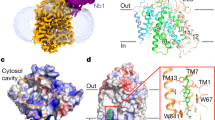
The sodium glucose cotransporter 2 (SGLT2) plays an important role in renal glucose reabsorption, thus serves as a new target for the treatment of diabetes. The purpose of this study was to evaluate SHR3824 as a novel selective SGLT2 inhibitor and to characterize its in vivo effects on glucose homeostasis. The effects of chronic administration of SHR3824 on peripheral insulin sensitivity and pancreatic β-cell function were also investigated.
Methods:
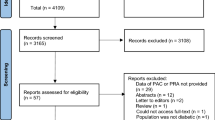
The in vitro potency and selectivity of SHR3824 were assessed in HEK293 cells transfected with human SGLT2 or SGLT1. Acute and multi-dose studies were performed on ICR mice, GK rats and db/db mice to assess the ability of SHR3824 to enhance urinary glucose excretion and improve blood glucose levels. 2-Deoxyglucose uptake and insulin immunohistochemical staining were performed in the soleus muscle and pancreas, respectively, of db/db mice. A selective SGLT2 inhibitor BMS512148 (dapagliflozin) was taken as positive control.
Results:
SHR3824 potently inhibited human SGLT2 in vitro, but exerted much weak inhibition on human SGLT1 (the IC50 values of SHR3824 against human SGLT2 and SGLT1 were 2.38 and 4324 nmol/L, respectively). Acute oral administration of SHR3824 (0.3, 1.0, 3.0 mg/kg) dose-dependently improved glucose tolerance in ICR mice, and reduced hyperglycemia by increasing urinary glucose excretion in GK rats and db/db mice. Chronic oral administration of SHR3824 (0.3, 1.0, 3.0 mg·kg−1·d−1) dose-dependently reduced blood glucose and HbA1c levels in GK rats and db/db mice, and significantly increased insulin-stimulated glucose uptake in the soleus muscles and enhanced insulin staining in the islet cells of db/db mice.
Conclusion:
SHR3824 is a potent and selective SGLT2 inhibitor and exhibits antidiabetic efficacy in several rodent models, suggesting its potential as a new therapeutic agent for the treatment of type 2 diabetes.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, et al. China National Diabetes and Metabolic Disorders Study Group. Prevalence of diabetes among men and women in China. N Engl J Med 2010; 362: 1090–101.
Kalra S, Mukherjee JJ, Venkataraman S, Bantwal G, Shaikh S, Saboo B, et al. Hypoglycemia: the neglected complication. Indian J Endocrinol Metab 2013; 17: 819–34.
Wright EM . Renal Na+-glucose cotransporters. Am J Physiol Renal Physiol 2001; 280: F10–8.
Hediger MA, Rhoads DB . Molecular physiology of sodium-glucose cotransporters. Physiol Rev 1994; 74: 993–1026.
Turk E, Zabel B, Mundlos S, Wright EM . Glucose/galactose malabsorption caused by a defect in the Na+/glucose cotransporter. Nature 1991; 350: 354–6.
Van den Heuvel LP, Assink K, Willemsen M, Monnens L . Autosomal recessive renal glucosuria attributable to a mutation in the sodium glucose cotransporter (SGLT2). Hum Genet 2002; 111: 544–7.
Ehrenkranz JR, Lewis NG, Kahn CR, Roth J . Phlorizin: a review. Diabetes Metab Res Rev 2005; 21: 31–8.
Oku A, Ueta K, Arakawa K, Ishihara T, Nawano M, Kuronuma Y, et al. T-1095, an inhibitor of renal Na+-glucose cotransporters, may provide a novel approach to treating diabetes. Diabetes 1999; 48: 1794–800.
Calado J . Dapagliflozin, an oral sodium glucose cotransporter type 2 inhibitor for the treatment of type 2 diabetes mellitus. IDrugs 2009; 12: 785–98.
Lamos EM, Younk LM, Davis SN . Canagliflozin, an inhibitor of sodium-glucose cotransporter 2, for the treatment of type 2 diabetes mellitus. Expert Opin Drug Metab Toxicol 2013; 9: 763–75.
Grempler R, Thomas L, Eckhardt M, Himmelsbach F, Sauer A, Sharp DE, et al. Empagliflozin, a novel selective sodium glucose cotransporter-2 (SGLT-2) inhibitor: characterisation and comparison with other SGLT-2 inhibitors. Diabetes Obes Metab 2012; 14: 83–90.
Miao Z, Nucci G, Amin N, Sharma R, Mascitti V, Tugnait M, et al. Pharmacokinetics, metabolism, and excretion of the antidiabetic agent ertugliflozin (PF-04971729) in healthy male subjects. Drug Metab Dispos 2013; 41: 445–56.
Han S, Hagan DL, Taylor JR, Xin L, Meng W, Biller SA, et al. Dapagliflozin, a selective SGLT2 inhibitor, improves glucose homeostasis in normal and diabetic rats. Diabetes 2008; 57: 1723–9.
Arakawa K, Ishihara T, Oku A, Nawano M, Ueta K, Kitamura K, et al. Improved diabetic syndrome in C57BL/KsJ-db/db mice by oral administration of the Na+-glucose cotransporter inhibitor T-1095. Br J Pharmacol 2001; 132: 578–86.
Thomas L, Grempler R, Eckhardt M, Himmelsbach F, Sauer A, Klein T, et al. Long-term treatment with empagliflozin, a novel, potent and selective SGLT-2 inhibitor, improves glycaemic control and features of metabolic syndrome in diabetic rats. Diabetes Obes Metab 2012; 14: 94–6.
Robertson RP, Harmon J, Tran PO, Poitout V . Beta-cell glucose toxicity, lipotoxicity, and chronic oxidative stress in type 2 diabetes. Diabetes 2004; 53: S119–24.
Jurczak MJ, Lee HY, Birkenfeld AL, Jornayvaz FR, Frederick DW, Pongratz RL, et al. SGLT2 deletion improves glucose homeostasis and preserves pancreatic beta-cell function. Diabetes 2011; 60: 890–8.
Kjorholt C, Akerfeldt MC, Biden TJ, Laybutt DR . Chronic hyperglycemia, independent of plasma lipid levels, is sufficient for the loss of beta cell differentiation and secretory function in the db/db mouse model of diabetes. Diabetes 2005; 54: 2755–63.
Jonas JC, Sharma A, Hasenkamp W, Ilkova H, Patanè G, Laybutt R, et al. Chronic hyperglycemia triggers loss of pancreatic beta cell differentiation in an animal model of diabetes. J Biol Chem 1999; 274: 14112–21.
Rossetti L, Shulman GI, Zawalich W, DeFronzo RA . Effect of chronic hyperglycemia on in vivo insulin secretion in partially pancreatectomized rats. J Clin Invest 1987; 80: 1037–44.
Liang Y, Arakawa K, Ueta K, Matsushita Y, Kuriyama C, Martin T, et al. Effect of canagliflozin on renal threshold for glucose, glycemia, and body weight in normal and diabetic animal models. PLoS One 2012; 7: e30555.
Macdonald FR, Peel JE, Jones HB, Mayers RM, Westgate L, Whaley JM, et al. The novel sodium glucose transporter 2 inhibitor dapagliflozin sustains pancreatic function and preserves islet morphology in obese, diabetic rats. Diabetes Obes Metab 2010; 12: 1004–12.
Wallberg-Henriksson H, Zetan N, Henriksson J . Reversibility of decreased insulin-stimulated glucose transport capacity in diabetic muscle with in vitro incubation. Insulin is not required. J Biol Chem 1987; 262: 7665–71.
Washburn WN . Development of the renal glucose reabsorption inhibitors: a new mechanism for the pharmacotherapy of diabetes mellitus type 2. J Med Chem 2009; 52: 1785–94.
Freeman JS . Review of insulin-dependent and insulin-independent agents for treating patients with type 2 diabetes mellitus and potential role for sodium-glucose co-transporter 2 inhibitors. Postgrad Med 2013; 125: 214–26.
Akash MS, Rehman K, Chen S . Goto-Kakizaki rats: its suitability as non-obese diabetic animal model for spontaneous type 2 diabetes mellitus. Curr Diabetes Rev 2013; 9: 387–96.
Herberg L, Leiter EH . Obesity/diabetes in mice with mutations in the leptin or leptin receptor genes. In: Shima, AAF, Shafrir, E (Eds), Animal Models of Diabetes A Primer. Harwood academic publishers, Amsterdam, 2001. pp 63–107.
Fujimori Y, Katsuno K, Nakashima I, Ishikawa-Takemura Y, Fujikura H, Isaji M . Remogliflozin etabonate, in a novel category of selective low-affinity sodium glucose cotransporter (SGLT2) inhibitors, exhibits antidiabetic efficacy in rodent models. J Pharmacol Exp Ther 2008; 327: 268–76.
Fujimori Y, Katsuno K, Ojima K, Nakashima I, Nakano S, Ishikawa-Takemura Y, et al. Sergliflozin etabonate, a selective SGLT2 inhibitor, improves glycemic control in streptozotocin-induced diabetic rats and Zucker fatty rats. Eur J Pharmacol 2009; 609: 148–54.
Araújo TG, Oliveira AG, Saad MJ . Insulin-resistance-associated compensatory mechanisms of pancreatic beta cells: a current opinion. Front Endocrinol (Lausanne) 2013; 4: 146.
DeFronzo RA, Tripathy D . Skeletal muscle insulin resistance is the primary defect in type 2 diabetes. Diabetes Care. 2009; 32: S157–63.
DeFronzo RA . The triumvirate: beta-cell, muscle, liver. A collusion responsible for NIDDM. Diabetes 1988; 37: 667–87.
Tsao TS, Burcelin R, Charron MJ . Regulation of hexokinase II gene expression by glucose flux in skeletal muscle. J Biol Chem 1996; 271: 14959–63.
Robertson RP, Zhang HJ, Pyzdrowski KL, Walseth TF . Preservation of insulin mRNA levels and insulin secretion in HIT cells by avoidance of chronic exposure to high glucose concentrations. J Clin Invest 1992; 90: 320–5.
Rossetti L . Glucose toxicity: the implications of hyperglycemia in the pathophysiology of diabetes mellitus. Clin Invest Med 1995; 18: 255–60.
Mooradian AD, Thurman JE . Glucotoxicity: potential mechanisms. Clin Geriatr Med 1999; 15: 255.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yan, Pk., Zhang, Ln., Feng, Y. et al. SHR3824, a novel selective inhibitor of renal sodium glucose cotransporter 2, exhibits antidiabetic efficacy in rodent models. Acta Pharmacol Sin 35, 613–624 (2014). https://doi.org/10.1038/aps.2013.196
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/aps.2013.196