Abstract
Aim:
Caveolin-1 (cav-1) is a major multifunctional scaffolding protein of caveolae. Cav-1 is primarily expressed in mesangial cells, renal proximal tubule cells and podocytes in kidneys. Recent evidence shows that the functional connections between cav-1 and ROS play a key role in many diseases. In this study we investigated whether regulating the functional connections between cav-1 and ROS in kidneys contributed to the beneficial effects of curcumin in treating diabetic nephropathy in vitro and in vivo.
Methods:
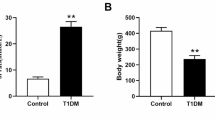
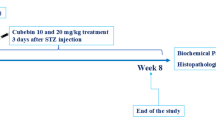
Cultured mouse podocytes (mpc5) were incubated in a high glucose (HG, 30 mmol/L) medium for 24, 48 or 72 h. Male rats were injected with STZ (60 mg/kg, ip) to induce diabetes. ROS generation, SOD activity, MDA content and caspase-3 activity in the cultured cells and kidney cortex homogenate were determined. Apoptotic proteins and cav-1 phosphorylation were analyzed using Western blot analyses.
Results:
Incubation in HG-containing medium time-dependently increased ROS production, oxidative stress, apoptosis, and cav-1 phosphorylation in podocytes. Pretreatment with curcumin (1, 5, and 10 μmol/L) dose-dependently attenuated these abnormalities in HG-treated podocytes. Furthermore, in HG-containing medium, the podocytes transfected with a recombinant plasmid GFP-cav-1 Y14F (mutation at a cav-1 phosphorylation site) exhibited significantly decreased ROS production and apoptosis compared with the cells transfected with empty vector. In diabetic rats, administration of curcumin (100 or 200 mg/kg body weight per day, ig, for 8 weeks) not only significantly improved the renal function, but also suppressed ROS levels, oxidative stress, apoptosis and cav-1 phosphorylation in the kidneys.
Conclusion:
Curcumin attenuates high glucose-induced podocyte apoptosis in vitro and diabetic nephropathy in vivo partly through regulating the functional connections between cav-1 phosphorylation and ROS.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Mogensen CE . Microalbuminuria and hypertension with focus on type 1 and type 2 diabetes. J Intern Med 2003; 254: 45–66.
Jim B, Ghanta M, Qipo A, Fan Y, Chuang PY, Cohen HW, et al. Dysregulated nephrin in diabetic nephropathy of type 2 diabetes: a cross sectional study. PLoS One 2012; 7: e36041.
Wei Q, Dong Z . HDAC4 blocks autophagy to trigger podocyte injury: non-epigenetic action in diabetic nephropathy. Kidney Int 2014; 6: 666–8.
Shankland SJ, Pippin JW, Reiser J, Mundel P . Podocytes in culture: past, present, and future. Kidney Int 2007; 72: 26–36.
Inoki K, Mori H, Wang J, Suzuki T, Hong S, Yoshida S, et al. mTORC1 activation in podocytes is a critical step in the development of diabetic nephropathy in mice. J Clin Invest 2011; 121: 2181–96.
Gupta SC, Patchva S, Koh W, Aggarwal BB . Discovery of curcumin, a component of golden spice, and its miraculous biological activities. Clin Exp Pharmacol Physiol 2012; 39: 283–99.
Sharma S, Kulkarni SK, Chopra K . Curcumin, the active principle of turmeric (Curcuma longa), ameliorates diabetic nephropathy in rats. Clin Exp Pharmacol Physiol 2006; 33: 940–5.
Liu JP, Feng L, Zhu MM, Wang RS, Zhang MH, Hu SY, et al. The in vitro protective effects of curcumin and demethoxycurcumin in Curcuma longa extract on advanced glycation end products-induced mesangial cell apoptosis and oxidative stress. Planta Med 2012; 78: 1757–60.
Neale TJ, Ullrich R, Ojha P, Poczewski H, Verhoeven AJ, Kerjaschki D . Reactive oxygen species and neutrophil respiratory burst cytochrome b558 are produced by kidney glomerular cells in passive Heymann nephritis. Proc Natl Acad Sci U S A 1993; 90: 3645–9.
Susztak K, Raff AC, Schiffer M, Bottinger EP . Glucose-induced reactive oxygen species cause apoptosis of podocytes and podocyte depletion at the onset of diabetic nephropathy. Diabetes 2006; 55: 225–33.
Piwkowska A, Rogacka D, Audzeyenka I, Jankowski M, Angielski S . High glucose concentration affects the oxidant-antioxidant balance in cultured mouse podocytes. J Cell Biochem 2011; 112: 1661–72.
Razani B, Engelman JA, Wang XB, Schubert W, Zhang XL, Marks CB, et al. Caveolin-1 null mice are viable but show evidence of hyperproliferative and vascular abnormalities. J Biol Chem 2001; 276: 38121–38.
Schubert W, Frank PG, Woodman SE, Hyogo H, Cohen DE, Chow CW, et al. Microvascular hyperpermeability in caveolin-1 (−/−) knock-out mice. Treatment with a specific nitric-oxide synthase inhibitor, L-name, restores normal microvascular permeability in cav-1 null mice. J Biol Chem 2002; 277: 40091–8.
Zhao YY, Zhao YD, Mirza MK, Huang JH, Potula HH, Vogel SM, et al. Persistent eNOS activation secondary to caveolin-1 deficiency induces pulmonary hypertension in mice and humans through PKG nitration. J Clin Invest 2009; 119: 2009–18.
Pavlides S, Tsirigos A, Vera I, Flomenberg N, Frank PG, Casimiro MC, et al. Loss of stromal caveolin-1 leads to oxidative stress, mimics hypoxia and drives inflammation in the tumor microenvironment, conferring the "reverse Warburg effect": a transcriptional informatics analysis with validation. Cell Cycle 2010; 9: 2201–19.
Cao H, Courchesne WE, Mastick CC . A phosphotyrosine-dependent protein interaction screen reveals a role for phosphorylation of caveolin-1 on tyrosine 14: recruitment of C-terminal Src kinase. J Biol Chem 2002; 277: 8771–4.
Zhang B, Peng F, Wu D, Ingram AJ, Gao B, Krepinsky JC . Caveolin-1 phosphorylation is required for stretch-induced EGFR and Akt activation in mesangial cells. Cell Signal 2007; 19: 1690–700.
Sun LN, Yang ZY, Lv SS, Liu XC, Guan GJ, Liu G . Curcumin prevents diabetic nephropathy against inflammatory response via reversing caveolin-1 Tyr phosphorylation influenced TLR4 activation. Int Immunopharmacol 2014; 23: 236–46.
Wang H, Madhusudhan T, He T, Hummel B, Schmidt S, Vinnikov IA, et al. Low but sustained coagulation activation ameliorates glucose-induced podocyte apoptosis: protective effect of factor V Leiden in diabetic nephropathy. Blood 2011; 117: 5231–42.
Riedl E, Pfister F, Braunagel M, Brinkkotter P, Sternik P, Deinzer M, et al. Carnosine prevents apoptosis of glomerular cells and podocyte loss in STZ diabetic rats. Cell Physiol Biochem 2011; 28: 279–88.
Xu J, Li Z, Xu P, Yang Z . Protective effects of leukemia inhibitory factor against oxidative stress during high glucose-induced apoptosis in podocytes. Cell Stress Chaperones 2012; 17: 485–93.
Liu BC, Song X, Lu XY, Li DT, Eaton DC, Shen BZ, et al. High glucose induces podocyte apoptosis by stimulating TRPC6 via elevation of reactive oxygen species. Biochim Biophys Acta 2013; 1833: 1434–42.
Chen J, Chen JK, Harris RC . EGF receptor deletion in podocytes attenuates diabetic nephropathy. J Am Soc Nephrol 2015; 26: 1115–25.
Pal PB, Sinha K, Sil PC . Mangiferin attenuates diabetic nephropathy by inhibiting oxidative stress mediated signaling cascade, TNFalpha related and mitochondrial dependent apoptotic pathways in streptozotocin-induced diabetic rats. PLoS One 2014; 9: e107220.
Deres P, Halmosi R, Toth A, Kovacs K, Palfi A, Habon T, et al. Prevention of doxorubicin-induced acute cardiotoxicity by an experimental antioxidant compound. J Cardiovasc Pharmacol 2005; 45: 36–43.
Nunez G, Benedict MA, Hu Y, Inohara N . Caspases: The proteases of the apoptotic pathway. Oncogene 1998; 17: 3237–45.
Elkady AI, Hussein RA, Abu-Zinadah OA . Effects of crude extracts from medicinal herbs Rhazya stricta and Zingiber officinale on growth and proliferation of human brain cancer cell line in vitro. Biomed Res Int 2014; 2014: 260210.
Couet J, Li S, Okamoto T, Ikezu T, Lisanti MP . Identification of peptide and protein ligands for the caveolin-scaffolding domain. Implications for the interaction of caveolin with caveolae-associated proteins. J Biol Chem 1997; 272: 6525–33.
Razani B, Woodman SE, Lisanti MP . Caveolae: from cell biology to animal physiology. Pharmacol Rev 2002; 54: 431–67.
Zhang Y, Peng F, Gao B, Ingram AJ, Krepinsky JC . High glucose-induced RhoA activation requires caveolae and PKCbeta1-mediated ROS generation. Am J Physiol Renal Physiol 2012; 302: F159–72.
Wu T, Zhang B, Ye F, Xiao Z . A potential role for caveolin-1 in VEGF-induced fibronectin upregulation in mesangial cells: involvement of VEGFR2 and Src. Am J Physiol Renal Physiol 2013; 304: F820–30.
Wu SZ, Peng FF, Li JL, Ye F, Lei SQ, Zhang BF . Akt and RhoA activation in response to high glucose require caveolin-1 phosphorylation in mesangial cells. Am J Physiol Renal Physiol 2014; 306: F1308–17.
Cerqueira DM, Tran U, Romaker D, Abreu JG, Wessely O . Sterol carrier protein 2 regulates proximal tubule size in the Xenopus pronephric kidney by modulating lipid rafts. Dev Biol 2014; 394: 54–64.
Lee YJ, Kim MO, Ryu JM, Han HJ . Regulation of SGLT expression and localization through Epac/PKA-dependent caveolin-1 and F-actin activation in renal proximal tubule cells. Biochim Biophys Acta 2012; 1823: 971–82.
Ren Z, Liang W, Chen C, Yang H, Singhal PC, Ding G . Angiotensin II induces nephrin dephosphorylation and podocyte injury: role of caveolin-1. Cell Signal 2012; 24: 443–50.
Chen F, Barman S, Yu Y, Haigh S, Wang Y, Black SM, et al. Caveolin-1 is a negative regulator of NADPH oxidase-derived reactive oxygen species. Free Radic Biol Med 2014; 73: 201–13.
Martinez-Outschoorn UE, Balliet RM, Rivadeneira DB, Chiavarina B, Pavlides S, Wang C, et al. Oxidative stress in cancer associated fibroblasts drives tumorstroma co-evolution: a new paradigm for understanding tumor metabolism, the field effect and genomic instability in cancer cells. Cell Cycle 2010; 9: 3256–76.
Martinez-Outschoorn UE, Pavlides S, WhitakerMenezes D, Daumer KM, Milliman JN, Chiavarina B, et al. Tumor cells induce the cancer associated fibroblast phenotype via caveolin-1 degradation: implications for breast cancer and dcis therapy with autophagy inhibitors. Cell Cycle 2010; 9: 2423–33.
Martinez-Outschoorn UE, Trimmer C, Lin Z, Whitaker-Menezes D, Chiavarina B, Zhou J, et al. Autophagy in cancer associated fibroblasts promotes tumor cell survival: role of hypoxia, hif1 induction and nfκb activation in the tumor stromal microenvironment. Cell Cycle 2010; 9: 3515–33.
Shiroto T, Romero N, Sugiyama T, Sartoretto JL, Kalwa H, Yan Z, et al. Caveolin-1 is a critical determinant of autophagy, metabolic switching, and oxidative stress in vascular endothelium. PLoS One 2014; 9: e87871.
Chanvorachote P, Chunhacha P . Caveolin-1 regulates endothelial adhesion of lung cancer cells via reactive oxygen species-dependent mechanism. PLoS One 2013; 8: e57466.
Anand P, Kunnumakkara AB, Newman RA, Aggarwal BB . Bioavailability of curcumin: problems and promises. Mol Pharm 2007; 4: 807–18.
Acknowledgements
We thank the Central Research Laboratory in The Second Hospital of Shandong University for constructive comments and suggestions. We also thank the Laboratory Animal Center of the Second Hospital of Shandong University for the excellent rat care.
This study was supported by the Ministry of Health as “Twelve Five-Year” National Science and Technology Support Program, China (No 2011BAI10B00).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Sun, Ln., Liu, Xc., Chen, Xj. et al. Curcumin attenuates high glucose-induced podocyte apoptosis by regulating functional connections between caveolin-1 phosphorylation and ROS. Acta Pharmacol Sin 37, 645–655 (2016). https://doi.org/10.1038/aps.2015.159
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/aps.2015.159
Keywords
This article is cited by
-
Therapeutic effect of curcumin and C60 fullerene against hyperglycemia-mediated tissue damage in diabetic rat lungs
Journal of Bioenergetics and Biomembranes (2021)
-
Curcumin induces therapeutic angiogenesis in a diabetic mouse hindlimb ischemia model via modulating the function of endothelial progenitor cells
Stem Cell Research & Therapy (2017)
-
Chrysin ameliorates podocyte injury and slit diaphragm protein loss via inhibition of the PERK-eIF2α-ATF-CHOP pathway in diabetic mice
Acta Pharmacologica Sinica (2017)
-
Caveolin-1 in the Pathogenesis of Diabetic Nephropathy: Potential Therapeutic Target?
Current Diabetes Reports (2017)