Abstract
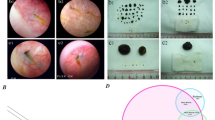
Hypomotility is a common symptom of gallstone disease, which is accompanied by a loss of interstitial Cajal-like cells (ICLCs) in the gallbladder. Ursodeoxycholic acid (UDCA) is widely used in treating gallstone disease, and has shown anti-apoptotic and anti-inflammatory effects apart from its ability to dissolve gallstones. In this study, we investigated the anti-apoptotic and anti-inflammatory effects of UDCA on ICLCs in guinea pigs with gallstones. Guinea pigs were fed a high-cholesterol diet for 8 weeks to induce the formation of gallstones. A group of animals was administered UDCA (50 mg·kg−1·d−1, ig) simultaneously. At the end of 8 weeks, the animals were euthanized with anesthesia, cholecystectomy was performed immediately and gallbladder was collected for further analysis. We showed that in the model group the contractility of gallbladder muscle strips in response to both acetylcholine (ACh) and CCK-8 was severely impaired, which was significantly improved by UDCA administration. Furthermore, UDCA administration significantly reduced the apoptotic ratio of ICLCs, based on the observation of co-localization imaging of apoptotic cells and c-kit-positive cells. Western blotting analysis and real-time PCR results revealed that the TNF-α/Caspase8/Caspase3 pathway was suppressed in the UDCA-treated animals, confirming the anti-apoptotic effect of UDCA in the gallbladder. The H&E staining showed that UDCA administration significantly attenuated inflammatory cell infiltration in the gallbladder wall. In conclusion, UDCA can protect ICLCs in the gallbladder from undergoing apoptosis by inhibiting the TNF-α/Caspase8/caspase3 pathway.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Lammert F, Gurusamy K, Ko CW, Miquel JF, Méndez-Sánchez N, Portincasa P, et al. Gallstones. Nat Rev Dis Primers 2016; 2: 1–7.
Pasternak A, Gajda M, Gil K, Matyja A, Tomaszewski KA, Walocha JA, et al. Evidence of interstitial Cajal-like cells in human gallbladder. Folia Histochem Cytobiol 2012; 50: 581–5.
Ahmadi O, Nicholson M de L, Gould ML, Mitchell A, Stringer MD. Interstitial cells of Cajal are present in human extrahepatic bile ducts. J Gastroenterol Hepatol 2010; 25: 277–85.
Hinescu ME, Ardeleanu C, Gherghiceanu M, Popescu LM. Interstitial Cajal-like cells in human gallbladder. J Mol Histol 2007; 38: 275–84.
Sanders KM, Ward SM, Koh SD. Interstitial cells: regulators of smooth muscle function. Physiol Rev 2014; 94: 859–907.
Pasternak A, Gil K, Gajda M, Tomaszewski KA, Matyja A, Walocha JA. Interstitial cajal-like cell: a new player in cholelithiasis? Am J Gastroenterol 2014; 109: 603–4.
Franks I. Gallbladder: Loss of interstitial Cajal-like cells in the gallbladder might contribute to gallstone formation. Nat Rev Gastroenterol Hepatol 2012; 9: 689.
Pasternak A, Gil K, Matyja A, Gajda M, Sztefko K, Walocha JA, et al. Loss of gallbladder interstitial Cajal-like cells in patients with cholelithiasis. Neurogastroenterol Motil 2013; 25: e17–24.
Bellentani S. Immunomodulating and anti-apoptotic action of ursodeoxycholic acid: where are we and where should we go? Eur J Gastroenterol Hepatol 2005; 17: 137–40.
Tomida S, Abei M, Yamaguchi T, Matsuzaki Y, Shoda J, Tanaka N, et al. Long-term ursodeoxycholic acid therapy is associated with reduced risk of biliary pain and acute cholecystitis in patients with gallbladder stones: a cohort analysis. Hepatology 1999; 30: 6–13.
Guarino MP, Carotti S, Morini S, Perrone G, Behar J, Altomare A, et al. Decreased number of activated macrophages in gallbladder muscle layer of cholesterol gallstone patients following ursodeoxycholic acid. Gut 2008; 57: 1740–1.
Cajal SR. Histologie du systeme Nerveux de I'Homme et des vertebres. Pairs: Maloine, 1911.
Marín VG, Freire MA. The interstitial cells of Cajal in pancreas. J Cell Mol Med 2005; 9: 475.
Wickramasinghe SR, Patel VV. Local innervation and atrial fibrillation. Circulation 2013; 128: 1566–75.
Drumm BT, Koh SD, Andersson KE, Ward SM. Calcium signalling in Cajal-like interstitial cells of the lower urinary tract. Nat Rev Urol 2014; 11: 555–64.
Popescu LM, Ciontea SM, Cretoiu D. Interstitial Cajal-like cells in human uterus and fallopian tube. Ann N Y Acad Sci 2007; 1101: 139–65.
Huang Y, Mei F, Yu B, Zhang HJ, Han J, et al. Distribution of the interstitial Cajal-like cells in the gallbladder and extrahepatic biliary duct of the guinea-pig. Acta Histochem 2009; 111: 157–65.
Balemba OB, Bartoo AC, Nelson MT, et al. Role of mitochondria in spontaneous rhythmic activity and intracellular calcium waves in the guinea pig gallbladder smooth muscle. Am J Physiol Gastrointest Liver Physiol 2008; 294: G467–76.
Lennartsson J, Ronnstrand L. Stem cell factor receptor/c-Kit: from basic science to clinical implications. Physiol Rev 2012; 92: 1619–49.
Lavoie B, Balemba OB, Nelson MT, Ward SM, Mawe GM. Morphological and physiological evidence for interstitial cell of Cajal-like cells in the guinea pig gallbladder. J Physiol 2007; 579: 487–501.
Sun X, Yu B, Xu L, Dong W, Luo H. Interstitial cells of Cajal in the murine gallbladder. Scand J Gastroenterol 2006; 41: 1218–26.
Xu D, Yu BP, Luo HS, Chen LD. Control of gallbladder contractions by cholecystokinin through cholecystokinin-A receptors on gallbladder interstitial cells of Cajal. World J Gastroenterol 2008; 14: 2882–7.
Ward SM, Beckett EA, Wang X, Baker F, Khoyi M, Sanders KM. Interstitial cells of Cajal mediate cholinergic neurotransmission from enteric motor neurons. J Neurosci 2000; 20: 1393–403.
Huang ZP, Qiu H, Yang Y, Yu BP. Effect of neutrophils on gallbladder interstitial Cajal-like cells in guinea pig model of acute cholecystitis. Cell Physiol Biochem 2016; 39: 2033–43.
Guarino MP, Cong P, Cicala M, Alloni R, Carotti S, Behar J. Ursodeoxycholic acid improves muscle contractility and inflammation in symptomatic gallbladders with cholesterol gallstones. Gut 2007; 56: 815–20.
Weitzel C, Stark D, Kullmann F, Schölmerich J, Holstege A, Falk W. Ursodeoxycholic acid induced activation of the glucocorticoid receptor in primary rat hepatocytes. Eur J Gastroenterol Hepatol 2005; 17: 169–77.
Fischer S, Müller I, Zündt BZ, Jüngst C, Meyer G, Jüngst D. Ursodeoxycholic acid decreases viscosity and sedimentable fractions of gallbladder bile in patients with cholesterol gallstones. Eur J Gastroenterol Hepatol 2004; 16: 305–11.
Xiao ZL, Amaral J, Biancani P, Behar J. Impaired cytoprotective function of muscle in human gallbladders with cholesterol stones. Am J Physiol Gastrointest Liver Physiol 2005; 288: G525–32.
Wang DQ, Schmitz F, Kopin AS, Carey MC. Targeted disruption of the murine cholecystokinin-1 receptor promotes intestinal cholesterol absorption and susceptibility to cholesterol cholelithiasis. J Clin Invest 2004; 114: 521–8.
Torihashi S, Nishi K, Tokutomi Y, Nishi T, Ward S, Sanders KM. Blockade of kit signaling induces transdifferentiation of interstitial cells of cajal to a smooth muscle phenotype. Gastroenterology 1999; 117: 140–8.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (81473570, U1402221, 81560663, and 81560685), Beijing Key Laboratory of New Drug Mechanisms and Pharmacological Evaluation Study (BZ0150), CAMS Innovation Fund for Medical Sciences (CIFMS) (2016-I2M-1-004), the Scientific Research Foundation of the Higher Education Institutions of Hunan Province (15K091), State Key Laboratory Fund Open Project (GTZK201610), and China Postdoctoral Science Foundation (2013M540066).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wan, Jf., Chu, Sf., Zhou, X. et al. Ursodeoxycholic acid protects interstitial Cajal-like cells in the gallbladder from undergoing apoptosis by inhibiting TNF-α expression. Acta Pharmacol Sin 39, 1493–1500 (2018). https://doi.org/10.1038/aps.2017.206
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/aps.2017.206
Keywords
This article is cited by
-
Metrnl deficiency decreases blood HDL cholesterol and increases blood triglyceride
Acta Pharmacologica Sinica (2020)