The class of 2016 at the University of Minnesota in Minneapolis had an unusual first year. Amid studying and adjusting to life away from home, a number of students on the Minneapolis campus were giving blood samples and anonymously divulging whether they had been ‘deep kissing’ anyone to immunologist Hank Balfour and his team. The aim of the year-long study was to examine in detail the effect of infectious mononucleosis — also known as mono or glandular fever — on students who had not encountered it before, and to inform the design of a vaccine against it.
Glandular fever might seem like an odd choice for vaccine development. It is usually regarded as an unpleasant but trivial illness that has few long-term effects. What’s more, the pathogenic microbe responsible, the Epstein–Barr virus (EBV), infects at least 90% of people, mostly asymptomatically in childhood, and stays in the body indefinitely. Spread through saliva — the reason why glandular fever is nicknamed the ‘kissing disease’ — it infects the skin-like epithelial cells of the throat and moves on to white blood cells called B cells, where its rapid replication can cause the fever, swollen lymph nodes and exhaustion typical of glandular fever. But Balfour’s work has revealed that glandular fever is a more debilitating and economically costly disease than is commonly thought. “This is a nasty virus,” he says.
Part of Nature Outlook: Lymphoma
More than half a century ago, EBV was identified as the first virus to help trigger a cancer in humans — Burkitt’s lymphoma, a type of non-Hodgkin’s lymphoma that typically occurs in children in Africa. Since then, EBV has been associated with an ever-growing list of malignancies, including Hodgkin’s lymphoma, nasopharyngeal cancer and gastric cancer. The virus can also trigger a lymphoma-like condition called post-transplant lymphoproliferative disorder (PTLD) in transplant recipients as well as a range of lymphomas and smooth-muscle tumours in people infected with HIV.
Although only a small proportion of people infected with EBV develop cancer as a result, the virus is associated with about 200,000 new cases each year — about 1% of the global cancer burden — with the problem being especially severe in poorer countries. And although a vaccine to prevent EBV infection has been in the works for years, problems such as a lack of suitable animal models and gaps in the understanding of EBV biology, together with glandular fever’s reputation as a trivial illness, have slowed the impetus to develop it further. But the lengthening list of human ills caused by EBV, including autoimmune diseases such as multiple sclerosis1, is prompting a rethink. “We detect a change in the wind,” says Graham Taylor, an immunologist working on EBV vaccines at the University of Birmingham, UK. “It’s starting to build into a resurgence of interest.” What’s more, innovative technologies that allow scientists to minutely examine the immune environment of cancers are informing the development of ‘therapeutic’ vaccines that train the body’s immune system to tackle tumours the virus has already caused.
Winning battles
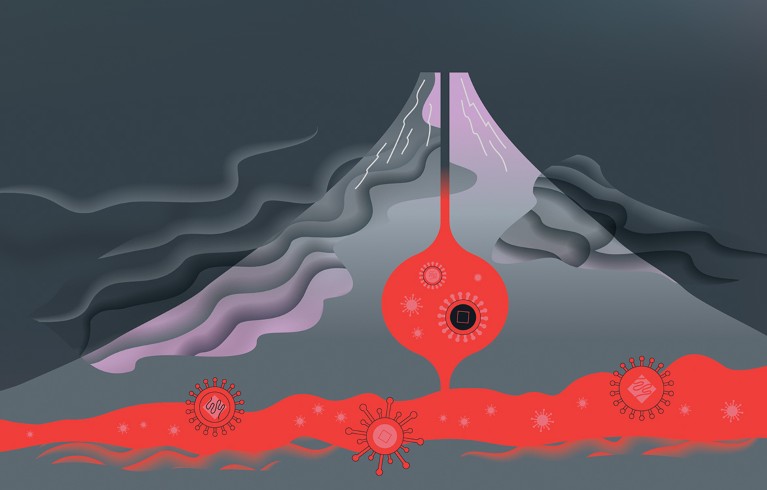
One problem facing vaccine researchers is the complicated life cycle of EBV. In the initial, or ‘lytic’, phase of infection, the virus replicates rapidly, its progeny erupting from each infected B cell before invading the next. This attracts the attention of the immune system, which, in most people, quashes the infection within a few weeks (although the person remains infectious for months).
But the immune system wins only the battle, not the war. EBV goes to ground — its ‘latent’ phase. During this part of its life cycle, no new virus particles are produced. Instead, it tucks its genome away inside a cell, activating just the bare minimum of genes it needs to survive and pass on a copy of its DNA each time its host cell divides. Proteins produced by the virus subvert the host cell’s behaviour to promote the virus’s survival, and slacken the cell’s anticancer defences. Once in a while, the virus switches to its lytic phase again, making its host cell silently infectious, before becoming latent once more. EBV infection is a life long, dynamic infection that is usually kept in check by the immune system in healthy people.
A key consideration for vaccine development is what kind of immune response is needed: one dominated by B cells, which make antibodies that stick to viruses before they enter cells; or one dominated by T cells, which seek out and destroy cells that are already infected.
The B-cell approach is the obvious choice for a preventive EBV vaccine. Researchers have long known that the clearest immune response to primary EBV infection is the production of antibodies against a protein on the virus’s surface called gp350, which the virus needs to infect B cells. And Balfour’s studies of undergraduates showed that people who make more antibodies, and make them sooner and for a longer period of time after initial infection, have milder symptoms of glandular fever. But it is too risky to pre-emptively generate anti-bodies against gp350 by simply injecting a weakened form of EBV into the body, as is the case with some common vaccines — the intact virus would still be able to promote cancer development.
Instead, researchers have turned to ‘sub-unit’ vaccines, which contain proteins, such as gp350, in isolation. So far, only one gp350 vaccine has reached phase II efficacy trials2. This vaccine, containing a solution of gp350, significantly reduced the risk of developing glandular fever, but did not prevent infection — one of the factors that dampened enthusiasm for developing it further. In 2017, Balfour, who had been collaborating on that work, negotiated access to the vaccine materials so that he could continue its development. He has also produced a formulation containing an alternative adjuvant — an immune-boosting ingredient — that he hopes will produce improved immune responses. He and his colleagues are preparing to ask the US Food and Drug Administration (FDA) for permission to test this version of the vaccine in first-year university students by 2020.
Another team developing a preventive vaccine based on gp350 is led by virologist Jeffrey Cohen at the US National Institute of Allergy and Infectious Diseases in Bethesda, Maryland. His team is using nanotechnology to present gp350 to immune cells in a way that maximizes the production of neutralizing antibodies3. These antibodies not only stick to the virus, but also disable its ability to infect cells. Instead of using a solution of gp350, the team attaches fragments, or epitopes, of the protein to nanoparticles, which increases the density of gp350 protein that each immune cell encounters. This also more closely mimics how immune cells might encounter the protein naturally, on viruses. Importantly, the spacing between neighbouring gp350 epitopes makes them particularly effective in activating key surface receptors on B cells that trigger the cells to divide and make antibodies. This helps to stimulate a more potent immune reaction to the vaccine.
The team also selected sections of gp350 that are vulnerable to immune attack to attach to its nanoparticles. As a result, antibody production increased between 10- and 100-fold compared with soluble gp350 in laboratory tests in animals. “We think the way gp350 is presented to the immune system is very important,” says Cohen.
His team is looking at other EBV surface proteins in addition to gp350, including ones that the virus uses to invade epithelial cells. The aim is to stimulate a broad range of neutralizing antibodies. Cohen and his team are seeking FDA approval to begin clinical trials, which they hope will take place in 2019 or 2020.

Hank Balfour (right) and colleagues at the University of Minnesota in Minneapolis.Credit: UMN Medical School
Intriguingly, the measure of success of preventive vaccines might not hinge on whether they can completely prevent infection. Research conducted after the earlier vaccine trials suggests that simply keeping the virus at a minimal level could be enough to prevent the development of both glandular fever and EBV malignancies. Studies of immunosuppressed transplant patients show that the higher the level of EBV in their blood, the higher their chances of developing an EBV lymphoma. “We think if we could keep the level of virus very low in the bloodstream of healthy people, that would potentially reduce the risk of them developing EBV-associated cancers,” says Cohen. For example, people who develop glandular fever have a more than threefold increased risk of developing Hodgkin’s lymphoma in the following decade, although the risk of getting the cancer remains low. “If we could prevent glandular fever, we should be able to prevent some Hodgkin’s lymphoma, and even potentially autoimmune diseases such as multiple sclerosis,” says Balfour.
Given the long gap between infection and disease, determining whether the vaccine prevents cancer will be tricky. That is especially true for conditions such as nasopharyngeal cancer, which can take decades to manifest. But studies of transplant patients might help. When lymphomas arise, they typically develop within three years of a transplant. One way of testing the vaccine’s anticancer properties, therefore, would be to vaccinate people, especially children, who have not been exposed to EBV before transplantation. Another approach would be to look for biomarkers — molecules or other early warning signs — that might indicate whether an individual is likely to develop cancer. These aided the development of the human papillomavirus vaccine, which tackles the viruses that cause cervical cancer. But Cohen downplays hopes of rapid success. “A lot more basic research needs to be done in addition to vaccine trials to learn more about the virus,” he says.
Protein patterns
EBV infection is a double-edged sword. It can increase the risk of developing cancer, but it also offers a neat solution to one of the problems of treating malignancies: finding something unique to cancer cells that can be targeted by therapies, sparing healthy cells. In this case, tumour cells producing EBV proteins could potentially be sought out by T cells capable of destroying infected cells.
The trouble is, EBV is adept at flying under the radar. On entering latency, the virus activates one of four latency programs. In latency 0, no proteins are made; in latency 1, a single protein called EBNA-1 is produced; and in latency 2, the virus activates two further protein-coding genes. The virus also produces proteins in a way that makes it difficult for immune cells to detect them. This allows EBV to persist in a person who has a functioning immune system. In immunosuppressed people, the virus switches to latency 3, in which it makes several proteins and is highly visible to immune cells. All of the various proteins produced at each latency stage have evolved mechanisms to minimize the immune response against them. And after a cell becomes cancerous, there is a further complication: tumours evolve ways to neuter the immune response, such as by producing a molecule called PD-L1 that shuts down active T cells.
Vaccine researchers are taking heart from the success of an immune-based therapy for EBV tumours called adoptive T-cell immunotherapy. Here, scientists extract immune cells from people with cancer, stoke them with EBV proteins and grow armies of responsive immune cells in the lab, before transfusing them back into patients. In 1995, Cliona Rooney, then at St Jude Children’s Research Hospital in Memphis, Tennessee, showed the approach could prevent and control PTLD in transplant patients4. This was the first demonstration that T cells could be targeted to EBV tumours, suggesting that a therapeutic vaccine might indeed work. “That was the major breakthrough,” says Rajiv Khanna, an immunologist at the QIMR Berghofer Medical Research Institute in Brisbane, Australia.
But although Rooney’s work provided a proof of principle, EBV in people with PTLD shows the latency-3 pattern — the easiest for immune cells to detect. The next challenge was extending the approach to lymphomas and nasopharyngeal cancer, in which latencies 1 and 2 predominate. In addition to being only weakly immunogenic, the proteins produced in these programs are involved in turning cells cancerous, so they can’t be included in an intact form in a vaccine. Instead, researchers have to cut the proteins down to include only the epitopes that elicit an immune response.
T-cell stimulation
Scientists are using a range of approaches to tackle this. Khanna’s team, for example, aims to generate an immune broadside against latent EBV by stringing together the key epitopes of the latency-1 and -2 proteins like beads in a necklace, which the group can use to stimulate T cells. The therapy is now in phase II trials in people with nasopharyngeal cancer, and Khanna hopes to test it in people with lymphoma in the near future. Khanna’s team, as well as several other groups around the world, is moving away from the long and involved process of using a patient’s own T cells; instead, the group is trying to generate banks of donor cells that could be used ‘off the shelf’ in tissue-matched patients — an approach that promises to reduce the time and cost of delivering therapies.
Other teams are developing more conventional protein-based therapeutic vaccines to train a patient’s immune system on their EBV-associated cancer. A key attraction of this approach is that it is relatively simple and standardized, says Taylor, who was first drawn into the field by the possibility of developing a therapeutic EBV vaccine for use in resource-limited countries. The vaccine his team has created is standardized and can be mass produced. It takes the form of a commonly used non-virulent virus called modified vaccinia Ankara, which has been loaded with two EBV proteins modified to eliminate their cancer-causing properties. Like Khanna, Taylor is convinced that generating the broadest possible range of immune responses is the best strategy. “If you have a single immune response,” he says, “you have a single point of failure.”
The strategy might pay off: the vaccine has passed two phase I trials, with blood tests revealing a good range of immune responses to the proteins. “We’ve provided proof of principle that it’s possible to boost immunity in patients though a therapeutic-vaccine approach,” says Taylor. The vaccine is now in phase II trials in people with nasopharyngeal cancer.
Taylor envisages the vaccine being used in conjunction with drugs that prevent tumours from using PD-L1 to shut down T-cell activity. Such drugs are already in use in cancer patients, including those with nasopharyngeal cancer, but have limited efficacy. Taylor sees the vaccine as a way to improve the performance of these drugs. There is preliminary evidence that such an approach can work, he says, from studies of people with cancer who are infected with the human papilloma virus.
While EBV-vaccine development continues apace, so do efforts to persuade policymakers of the social and economic value of such a vaccine. Balfour, for example, set up the Mono Project at the University of Minnesota partly to drive forward research, but also, he says, to raise awareness of EBV and glandular fever. And Cohen thinks there is a need for more epidemiological studies to gain a better idea of the economic burden of EBV. Indeed, a call for further studies to predict the possible benefit of a specific EBV vaccine was one of five priorities outlined at an EBV-vaccine meeting organized by the US National Institutes of Health in 2011.
Researchers can point to the success of other antiviral vaccines in preventing cancer. Almost 40 years ago, scientists unveiled a preventive vaccine against hepatitis B, a virus that can cause liver cancer, especially in children infected in infancy. Since being rolled out, the vaccine has prevented about 70% of hepatitis‑B-associated liver cancers. “We should take a great deal of heart from these successes,” says Taylor. “What we need now is the vaccine and the will to use it. If we have those, who knows what we can achieve?”

 Towards the better diagnosis of lymphoma
Towards the better diagnosis of lymphoma
 Genetically modified T cells target lymphoma
Genetically modified T cells target lymphoma
 The cost of surviving cancer
The cost of surviving cancer
 Precision therapies take aim at non-Hodgkin’s lymphoma
Precision therapies take aim at non-Hodgkin’s lymphoma
 Solving lymphoma’s stem-cell problem
Solving lymphoma’s stem-cell problem
 How dogs are teaching researchers new tricks for treating cancer
How dogs are teaching researchers new tricks for treating cancer
 Lymphoma: 4 big questions
Lymphoma: 4 big questions