Abstract
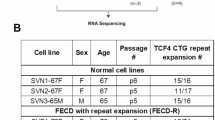
Fuchs’ endothelial dystrophy (FED) is a disease affecting the corneal endothelium. Recent studies reported significant association of polymorphisms in the TCF4 (transcription factor 4) gene, and a borderline association of PTPRG (protein tyrosine phosphatase, receptor type, G) variants with late-onset FED in Caucasians from the United States. Association of TCF4 has also been reported in the Chinese population. We aimed to determine association of the reported polymorphisms in TCF4 and PTPRG, and association of polymorphisms in the candidate genes ZEB1 (zinc-finger E-box binding homoebox 1), COL8A2 (collagen, type VIII, alpha 2), TGFBI (transforming growth factor, β-induced) and CLU (clusterin) in Australian cases. We also compared the expression of TGFBI and CLU proteins between FED and normal whole corneas. In all, 30 single-nucleotide polymorphisms (SNPs) from the candidate genes were genotyped in 103 cases and 275 controls. Each SNP and haplotype was assessed for association with the disease. SNP analysis identified an association of TCF4 (rs613872 (P=5.25 × 10−15, OR=4.05), rs9954153 (P=3.37 × 10−7, OR=2.58), rs2286812 (P=4.23 × 10−6, OR=2.55) and rs17595731 (P=3.57 × 10−5, OR=3.79)), CLU (rs17466684; P=0.003, OR=1.85) and one haplotype of TGFBI SNPs (P=0.011, OR=2.29) with FED in Caucasian Australians. No evidence for genetic association of PTPRG, ZEB1 and COL8A2 was found. Immunohistochemistry showed differential expression of CLU and TGFBI proteins in FED-affected compared with normal corneas. In conclusion, variation in TCF4, CLU and TGFBI, but not PTPRG, ZEB1 and COL8A2 genes are associated with FED in Caucasian Australian cases. Differential expression of CLU and TGFBI proteins in FED-affected corneas provides novel insights into the disease mechanism.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Kannabiran C : Genetics of corneal endothelial dystrophies. J Genet 2009; 88: 487–494.
Klintworth G : Corneal dystrophies. Orphanet J Rare Dis 2009; 4: 7.
Adamis AP, Filatov V, Tripathi BJ, Tripathi RC : Fuchs’ endothelial dystrophy of the cornea. Surv Ophthalmol 1993; 38: 149–168.
Kenney MC, Labermeier U, Hinds D, Waring GO : Characterization of the Descemet's membrane/posterior collagenous layer isolated from Fuchs’ endothelial dystrophy corneas. Exp Eye Res 1984; 39: 267–277.
Price MO, Gorovoy M, Benetz BA et al: Descemet's stripping automated endothelial keratoplasty outcomes compared with penetrating keratoplasty from the cornea donor study. Ophthalmology 2010; 117: 438–444.
Riazuddin SA, Zaghloul NA, Al-Saif A et al: Missense mutations in TCF8 cause late-onset Fuchs corneal dystrophy and interact with FCD4 on chromosome 9p. Am J Human Genet 2010; 86: 45–53.
Santo RM, Yamaguchi T, Kanai A, Okisaka S, Nakajima A : Clinical and histopathologic features of corneal dystrophies in Japan. Ophthalmology 1995; 102: 557–567.
Vithana EN, Morgan PE, Ramprasad V et al: SLC4A11 mutations in Fuchs endothelial corneal dystrophy. Hum Mol Genet 2008; 17: 656–666.
Williams KL, Bartlett MT, Kelly CM, Coster LDJ : The Australian Corneal Graft Registry: 2007 Report Adelaide: Flinders University 2007.
Biswas S, Munier FL, Yardley J et al: Missense mutations in COL8A2, the gene encoding the α2 chain of type VIII collagen, cause two forms of corneal endothelial dystrophy. Hum Mol Genet 2001; 10: 2415–2423.
Mok JW, Kim HS, Joo CK : Q455V mutation in COL8A2 is associated with Fuchs’ corneal dystrophy in Korean patients. Eye 2008; 23: 895–903.
Kabosova A, Azar DT, Bannikov GA et al: Compositional differences between infant and adult human corneal basement membranes. Invest Ophthalmol Vis Sci 2007; 48: 4989–4999.
Weiss JS : Corneal dystrophies: molecular genetics to therapeutic intervention—Fifth ARVO/Pfizer Ophthalmics Research Institute Conference. Invest Ophthalmol Vis Sci 2010; 51: 5391–5402.
Mehta JS, Vithana EN, Tan DTH et al: Analysis of the posterior polymorphous corneal dystrophy 3 gene, TCF8, in late-onset Fuchs endothelial corneal dystrophy. Invest Ophthalmol Vis Sci 2008; 49: 184–188.
Hurt E, Saykally J, Anose B, Kalli K, Sanders M : Expression of the ZEB1 (δEF1) transcription factor in human: additional insights. Mol Cell Biochem 2008; 318: 89–99.
Liu Y, El-Naggar S, Darling DS, Higashi Y, Dean DC : Zeb1 links epithelial–mesenchymal transition and cellular senescence. Development 2008; 135: 579–588.
Vandewalle C, Van Roy F, Berx G : The role of the ZEB family of transcription factors in development and disease. Cell Mol Life Sci 2009; 66: 773–787.
Riazuddin SA, Vithana EN, Seet L-F et al: Missense mutations in the sodium borate cotransporter SLC4A11 cause late-onset Fuchs corneal dystrophya. Hum Mutat 2010; 31: 1261–1268.
Baratz KH, Tosakulwong N, Ryu E et al: E2-2 protein and Fuchs’ corneal dystrophy. N Engl J Med 2010; 363: 1016–1024.
Riazuddin SA, McGlumphy EJ, Yeo WS, Wang J, Katsanis N, Gottsch JD : Replication of the TCF4 intronic variant in late-onset Fuchs corneal dystrophy and evidence of independence from the FCD2 locus. Invest Ophthalmol Vis Sci 2011; 52: 2825–2829.
Thalamuthu A, Khor CC, Venkataraman D et al: Association of TCF4 gene polymorphisms with Fuchs corneal dystrophy in the chinese. Invest Ophthalmol Vis Sci 2011; 52: 5573–5578.
Jurkunas UV, Bitar M, Rawe I : Colocalization of increased transforming growth factor-{beta}-induced protein (TG. Invest Ophthalmol Vis Sci 2009; 50: 1129–1136.
Kim JH, Kim JH, Jun HO et al: Protective effect of clusterin from oxidative stress-induced apoptosis in human retinal pigment epithelial cells. Invest Ophthalmol Vis Sci 2010; 51: 561–566.
Borderie VM, Baudrimont M, Vallee A, Ereau TL, Gray F, Laroche L : Corneal endothelial cell apoptosis in patients with Fuchs’ dystrophy. Invest Ophthalmol Vis Sci 2000; 41: 2501–2505.
Jurkunas UV, Bitar MS, Funaki T, Azizi B : Evidence of oxidative stress in the pathogenesis of Fuchs endothelial corneal dystrophy. Am J Pathol 2010; 177: 2278–2289.
Fuxe J, Vincent T, Garcia de Herreros A : Transcriptional crosstalk between TGF-beta and stem cell pathways in tumor cell invasion: role of EMT promoting Smad complexes. Cell Cycle 2010; 9: 2363–2374.
Wright AFMCP, Dhillon BBB : Major progress in Fuchs's corneal dystrophy. N Engl J Med 2010; 363: 1072–1075.
Krachmer JH, Purcell Jr JJ, Young CW, Bucher KD : Corneal endothelial dystrophy: a study of 64 families. Arch Ophthalmol 1978; 96: 2036–2039.
Barrett JC, Fry B, Maller J, Daly MJ : Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics 2005; 21: 263–265.
Purcell S, Neale B, Todd-Brown K et al: PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet 2007; 81: 559–575.
Purcell S, Cherny SS, Sham PC : Genetic Power Calculator: design of linkage and association genetic mapping studies of complex traits. Bioinformatics 2003; 19: 149–150.
Sharma S, Chataway T, Burdon KP et al: Identification of LOXL1 protein and apolipoprotein E as components of surgically isolated pseudoexfoliation material by direct mass spectrometry. Exp Eye Res 2009; 89: 479–485.
Sobrado VR, Moreno-Bueno G, Cubillo E et al: The class I bHLH factors E2-2A and E2-2B regulate EMT. J Cell Sci 2009; 122: 1014–1024.
Eger A, Aigner K, Sonderegger S et al: DeltaEF1 is a transcriptional repressor of E-cadherin and regulates epithelial plasticity in breast cancer cells. Oncogene 2005; 24: 2375–2385.
Sundin OH, Broman KW, Chang HH, Vito ECL, Stark WJ, Gottsch JD : A common locus for late-onset Fuchs corneal dystrophy maps to 18q21.2–q21.32. Invest Ophthalmol Vis Sci 2006; 47: 3919–3926.
Johnson DH, Bourne WM, Campbell RJ : The ultrastructure of Descemet's membrane: I. Changes with age in normal corneas. Arch Ophthalmol 1982; 100: 1942–1947.
Waring GO III : Posterior collagenous layer of the cornea. Ultrastructural classification of abnormal collagenous tissue posterior to Descemet's membrane in 30 cases. Arch Ophthalmol 1982; 100: 122–134.
Burdon KP, Sharma S, Hewitt AW et al: Genetic analysis of the clusterin gene in pseudoexfoliation syndrome. Mol Vis 2008; 14: 1727–1736.
Krumbiegel M, Pasutto F, Mardin CY et al: Exploring functional candidate genes for genetic association in German patients with pseudoexfoliation syndrome and pseudoexfoliation glaucoma. Invest Ophthalmol Vis Sci 2009; 50: 2796–2801.
Wilson SE, Bourne WM : Fuchs’ dystrophy. Cornea 1988; 7: 2–18.
Yellore VS, Rayner SA, Aldave AJ : TGFB1-induced extracellular expression of TGFBIp and inhibition of TGFBIp expression by RNA interference in a human corneal epithelial cell line. Invest Ophthalmol Vis Sci 2011; 52: 757–763.
Hecker LA, McLaren JW, Bachman LA, Patel SV : Anterior keratocyte depletion in Fuchs endothelial dystrophy. Arch Ophthalmol 2011; 129: 555–561.
Billings PC, Whitbeck JC, Adams CS et al: The transforming growth factor-Î2-inducible matrix protein Î2ig-h3 interacts with fibronectin. J Biol Chem 2002; 277: 28003–28009.
Takeyama Y, Sato M, Horio M et al: Knockdown of ZEB1, a master epithelial-to-mesenchymal transition (EMT) gene, suppresses anchorage-independent cell growth of lung cancer cells. Cancer Lett 2010; 296: 216–224.
Aldave AJ, Principe AH, Lin DY, Yellore VS, Small KW : Lattice dystrophy-like localized amyloidosis of the cornea secondary to trichiasis. Cornea 2005; 24: 112–115.
Suesskind D, Auw-Haedrich C, Schorderet DF, Munier FL, Loeffler KU : Keratoepithelin in secondary corneal amyloidosis. Graefes Arch Clin Exp Ophthalmol 2006; 244: 725–725-731.
Acknowledgements
We thank all the participants for taking part in this study. This work was supported by grant from the Ophthalmic Research Institute of Australia. KPB and JEC are, respectively, supported by the National Health and Medical Research Council of Australia Career Development Award and Practitioner Fellowship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kuot, A., Hewitt, A., Griggs, K. et al. Association of TCF4 and CLU polymorphisms with Fuchs’ endothelial dystrophy and implication of CLU and TGFBI proteins in the disease process. Eur J Hum Genet 20, 632–638 (2012). https://doi.org/10.1038/ejhg.2011.248
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/ejhg.2011.248
Keywords
This article is cited by
-
Influence of clusterin genetic variants on IOP elevation in pseudoexfoliation syndrome and pseudoexfoliative glaucoma in Turkish population
BMC Ophthalmology (2023)
-
The Molecular Basis of Fuchs’ Endothelial Corneal Dystrophy
Molecular Diagnosis & Therapy (2019)
-
Genome-wide association study identifies three novel loci in Fuchs endothelial corneal dystrophy
Nature Communications (2017)
-
Association of TCF4 polymorphisms and fuchs’ endothelial dystrophy: a meta-analysis
BMC Ophthalmology (2015)
-
What does the future hold for the treatment of Fuchs endothelial dystrophy; will ‘keratoplasty’ still be a valid procedure?
Eye (2013)