Abstract
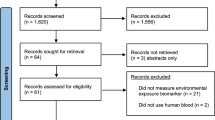
Despite international adoption of newborn bloodspot screening (DBS), no two countries' screening programs are the same. This article aims to understand what factors influence DBS decision-making criteria and how conditions are assessed against them. In doing so, it offers unique insights into the international landscape of DBS. A systematic review on DBS criteria in scientific literature was first undertaken. Through this, five topics were identified for consideration when analyzing DBS decision-making. Using these five topics as a template, a side-by-side comparison was conducted on DBS in policy documents of eight countries. Programs are using different approaches to explore the same policy issues, including: the beneficiary of DBS, definition of criteria, the way conditions are assessed, level of evidence required, and recommendations after assessment. These differences have the potential to result in increased disparity across DBS internationally. Ultimately, governments need to decide on their role and develop an approach to DBS decision-making in line with this role. The analyses presented in this article highlight that despite programs' commonalities, no one 'DBS decision-making solution' exists. Understanding the different approaches to decision-making within the literature and policy settings, provides an objective starting point for structured decision-making approaches for DBS programs.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Grosse SD, Boyle CA, Kenneson A, Khoury MJ, Wilfond BS : From public health emergency to public health service: the implications of evolving criteria for newborn screening panels. Pediatrics 2006; 117: 923–929.
World Health Organization. Early detection of cancer, 2015. Available from: http://who.int/cancer/detection/en/. Accessed on 3 March 2015.
Australian Population Health Development Principal Committee. Screening Subcommittee: Population Based Screening Framework, 2008.
Health Council of The Netherlands Screening: Between Hope and Hype 2008.
Elliman DAC, Dezateux C, Bedford HE : Newborn and childhood screening programmes: criteria, evidence, and current policy. Arch Dis Child 2002; 87: 6–9.
UK National Screening Committee. What is screening? 2015. Available from: http://www.screening.nhs.uk/cms.php?folder=2436. Accessed on 29 March 2015.
Andermann A, Blancquaert I, Beauchamp S, Dery V : Revisiting Wilson and Jungner in the genomic age: a review of screening criteria over the past 40 years. Bull World Health Organ [online] 2008; 86: 317–319.
Therrell BL, Padilla CD, Loeber JG et al: Current status of newborn screening worldwide, 2015 Sem Perinat 2015; 39: 171–187.
Petros M : Revisiting the Wilson-Jungner criteria: how can supplemental criteria guide public health in the era of genetic screening? Genet Med 2012; 14: 129–134.
Pollitt RJ : Introducing new screens: Why are we all doing different things? J Inherit Metab Dis 2007; 30: 423–429.
Wilfond BS, Parad RB, Fost N : Balancing benefits and risks for cystic fibrosis newborn screening: implications for policy decisions. J Pediatr 2005; 147: S109–S113.
Moyer VA, Calonge N, Teutsch SM, Botkin JR : Expanding newborn screening: process, policy, and priorities. Hastings Cent Rep 2008; 38: 32–39.
Plass AMC, van El CG, Pieters T, Cornel MC : Neonatal screening for treatable and untreatable disorders: prospective parents' opinions. Pediatrics 2010; 125: e99–e106.
Avard D, Vallance H, Greenberg C, Potter B : Newborn screening by tandem mass spectrometry: ethical and social issues. Can J Public Health 2007; 98: 284–286.
Calonge N, Green NS, Rinaldo P et al: Committee report: method for evaluating conditions nominated for population-based screening of newborns and children. Genet Med 2010; 12: 153–159.
Maxwell SJ, O'Leary P : Newborn bloodspot screening: setting the Australian national policy agenda. Med J Aust 2014; 200: 142–143.
Pollitt RJ : Newborn blood spot screening: new opportunities, old problems. J Inherit Metab Dis 2009; 32: 395–399.
Seymour CA, Thomason MJ, Chalmers RA et al: Newborn screening for inborn errors of metabolism: a systematic review. Health Technol Assess 1997; 1: i-iv 1–95.
Borte S, von Döbeln U, Hammarström L : Guidelines for newborn screening of primary immunodeficiency diseases. Curr Opin Hematol 2013; 20: 48–54.
Dhondt JL : Expanded newborn screening: social and ethical issues. J Inherit Metab Dis 2010; 33: S211–S217.
Wilson JMG, Jungner G : Principles and Practice of Screening for Disease; World Health Organization: Geneva 1986. Available from: http://www.who.int/bulletin/volumes/86/4/07-050112bp.pdf?ua=1.
Botkin JR : Assessing the new criteria for newborn screening. Health Matrix Clevel 2009; 19: 163–186.
Forman J, Coyle F, Levy-Fisch J, Roberts P, Terry S, Legge M : Screening criteria: the need to deal with new developments and ethical issues in newborn metabolic screening. J Commun Genet 2013; 4: 59–67.
Green A, Pollitt RJ : Population newborn screening for inherited metabolic disease: current UK perspectives. J Inherit Metab Dis 1999; 22: 572–579.
Pollitt RJ : International perspectives on newborn screening. J Inherit Metab Dis 2006; 29: 390–396.
Potter BK, Avard D, Wilson BJ : Newborn blood spot screening in four countries: stakeholder involvement. J Public Health Policy 2008; 29: 121–142.
Bonham JR : Impact of new screening technologies: should we screen and does phenotype influence this decision? J Inherit Metab Dis 2013; 36: 681–686.
Grosse SD, Kalman L, Khoury MJ : Evaluation of the validity and utility of genetic testing for rare diseases. Adv Exp Med Biol 2010; 686: 115–131.
Ross LF : Newborn screening for lysosomal storage diseases: an ethical and policy analysis. J Inherit Metab Dis 2012; 35: 627–634.
Feuchtbaum L, Faulkner L, Verghese S : Tandem mass spectrometry program implementation challenges for state newborn screening programs: national survey of barriers and issues. Pediatrics 2006; 117: S253–S260.
Ross LF : Predictive genetic testing for conditions that present in childhood. Kennedy Inst Ethics J 2002; 12: 225–244.
Waggoner DJ, Tan CA : Expanding newborn screening for lysosomal disorders: opportunities and challenges. Dev Disabil Res Rev 2011; 17: 9–14.
Ross LF, Moon MR : Ethical issues in genetic testing of children. Arch Pediatr Adolesc Med 2000; 154: 873–879.
Cornel MC, Rigter T, Weinreich SS et al: A framework to start the debate on neonatal screening policies in the EU: an expert opinion document. Eur J Hum Genet 2014; 22: 12–17.
Bunnik EM, de Jong A, Nijsingh N, de Wert GMWR : The new genetics and informed consent: differentiating choice to preserve autonomy. Bioethics 2013; 27: 348–355.
Bailey DB Jr., Beskow LM, Davis AM, Skinner D : Changing perspectives on the benefits of newborn screening. Mental Retard Dev Disabil Res Rev 2006; 12: 270–279.
Bombard Y, Miller FA, Hayeems RZ, Avard D, Knoppers BM : Reconsidering reproductive benefit through newborn screening: a systematic review of guidelines on preconception, prenatal and newborn screening. Eur J Hum Genet 2010; 18: 751–760.
Buchbinder M, Timmermans S : Newborn screening and maternal diagnosis: rethinking family benefit. Social Sci Med 2011; 73: 1014–1018.
Natowicz M : Newborn screening—setting evidence-based policy for protection. N Engl J Med 2005; 353: 867–870.
Botkin JR, Clayton EW, Fost NC et al: Newborn screening technology: proceed with caution. Pediatrics 2006; 117: 1793–1799.
Kemper AR, Green NS, Calonge N et al: Decision-making process for conditions nominated to the recommended uniform screening panel: statement of the US Department of Health and Human Services Secretary's Advisory Committee on Heritable Disorders in Newborns and Children. Genet Med 2014; 16: 183–187.
Watson M, Mann MY, Lloyd-Puryear M, Rinaldo P, Howell RR : Newborn screening: toward a uniform screening panel and system—executive summary. Pediatrics 2006; 117: S296–S307.
Kemper AR, Kus CA, Ostrander RJ et al: A framework for key considerations regarding point-of-care screening of newborns. Genet Med 2012; 14: 951–954.
Pollitt RJ : Principles and performance: assessing the evidence. Acta Paediatr Suppl 1999; 432: 110–114.
Zwahlen M, Low N, Borisch B et al: Population based screening - the difficulty of how to do more good than harm and how to achieve it. Swiss Med Wkly 2010; 140: w13061.
American College of Medical Genetics. Newborn Screening: Toward a Uniform Screening Panel and System, 2006.
Advisory Committee on Heritable Disorders in Newborns and Children. Form for Nomination of a Condition for Inclusion in the Uniform Screening Panel: Health Resources and Services Administration, U.S., 2015. Available from: http://www.hrsa.gov/advisorycommittees/mchbadvisory/heritabledisorders/nominatecondition/nominationform.pdf.
Human Genetics Society of Australasia. Newborn bloodspot testing, 2011. Available from: https://www.hgsa.org.au/documents/item/29. Accessed on 29 March 2015.
Ministry of Health. Newborn Metabolic Screening Programma Policy Framework, 2011. Available from: https://www.nsu.govt.nz/system/files/page/newborn_metabolic_screening_programme_policy_framework_june_2011.pdf.
Nørgaard-Pedersen B, Hougaard DM : Newborn Screening for Congenital Disorders in Routine and Research: Handbook of Children with Special Health Care Needs. Springer: New York, NY, USA, 2012, pp 259–269.
Potter B : Addition of conditions to DBS in Ontario, Canada, 2015, (Personal Communication).
Health Council of The Netherlands. Neonatal screening: new recommendations. The Hague, 2015.
Agence d’évaluation des technologies et des modes d’intervention en santé (AETMIS)Tandem Mass Spectrometry and Neonatal Blood Screening in Quebec. Summary Report Prepared by Héla Makni, Carole St-Hilaire, Laura Robb, Kathy Larouche and Ingeborg Blancquaert (AETMIS 07-03) 2007: xviii-79 p.
Gemeinsamer Bundesausschuss. Bericht der Arbeitsgruppe Zuzahlung des UA Prävention zum Regelungsauftrag des par, 62 Abs. 1 Satz 3 SGB V. Berlin, 2007. Available from: https://www.g-ba.de/downloads/40-268-531/2007-11-06-Abschluss-Therapiegerecht.pdf.
Gemeinsamer Bundesausschuss. Kinder-Richtlinien, 2011. Available from: https://www.g-ba.de/informationen/richtlinien/15/. Accessed on 21 March 2015.
Health Council of The Netherlands. Neonatale screening. The Hague, 2005.
Nørgaard-Pedersen B, Hougaard DM : Storage policies and use of the Danish Newborn Screening Biobank. J Inherit Metab Dis 2007; 30: 530–536.
UK National Screening Committee. Evidence review process, 2015. Available from: http://www.screening.nhs.uk/evidencereview. Accessed on 29 March 2015.
UK National Screening Committee: The UK NSC recommendation on Glutaric Aciduria Type 1, 2015. Available from: http://www.screening.nhs.uk/ga1. Accessed on 29 March 2015.
Blancquaert I, Beauchamp S, Andermann A : Decision Support Guide For Population-based Genetic Screening, Québec: APOGEE-Net 2008. Available from: http://www.cangenetest.org/en/publications.html.
Morrison A, Dowler J: Newborn Screening for Disorders and Abnormalities in Canada: Environmental Scan, 26 edn. Canadian Agency for Drugs and Technologies in Health: Ottawa, ON, Canada, 2011.
Axmann B : Addition of SCID to NBS in Germany, 2015, (Personal Communication).
GKV: Antrag auf Bewertung eines Screenings auf schwere angeborene Immundefekte ("SCID-Screening) bei Neugeborenen gemäB par, 135 Abs. 1 SGB V i. V. m. par. 26 SGB V. Berlin 2014. Available from: https://www.g-ba.de/downloads/40-268-3132/2015-02-19_135-SN_SCID-Screening_Antrag.pdf.
Lindner M, Gramer G, Haege G et al: Efficacy and outcome of expanded newborn screening for metabolic diseases—report of 10 years from South-West Germany. Orphanet J Rare Dis 2011; 6: 1.
Fischer KE, Grosse SD, Rogowski WH : The role of health technology assessment in coverage decisions on newborn screening. Int J Technol Assess Health care 2011; 27: 313–321.
Therrell BL : US newborn screening policy dilemmas for the twenty-first century. Mol Genet Metab 2001; 74: 64–74.
Howard HC, Knoppers BM, Cornel MC, Clayton EW, Sénécal K, Borry P : Whole-genome sequencing in newborn screening? A statement on the continued importance of targeted approaches in newborn screening programmes. Eur J Hum Genet 2015; 23: 1593–1600.
Bombard Y, Miller FA, Hayeems RZ et al: Public views on participating in newborn screening using genome sequencing. Eur J Hum Genet 2014; 22: 1248–1254.
Borry P, Henneman L, Lakeman P, Leo P, Cornel MC, Howard HC : Preconceptional genetic carrier testing and the commercial offer directly-to-consumers. Hum Reprod 2011; 26: 972–977.
Acknowledgements
MEJ acknowledges APOGEE-Net/CanGèneTest (Canada, PI Prof A Brand, PhD MD) and Haak Bastiaanse Kuneman Stichting (Netherlands, PI ME Jansen, MSc) for their financial support. The financial support facilitated a research visit to the Office of Population Health Genomics, Perth Western Australia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Jansen, M., Metternick-Jones, S. & Lister, K. International differences in the evaluation of conditions for newborn bloodspot screening: a review of scientific literature and policy documents. Eur J Hum Genet 25, 10–16 (2017). https://doi.org/10.1038/ejhg.2016.126
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/ejhg.2016.126
This article is cited by
-
The potential and translational application of infant genetic research
Nature Genetics (2024)
-
The case for screening in early life for ‘non-treatable’ disorders: ethics, evidence and proportionality. A report from the Health Council of the Netherlands
European Journal of Human Genetics (2022)
-
Comparison of dried blood spot and plasma sampling for untargeted metabolomics
Metabolomics (2021)
-
Österreichisches Neugeborenen-Screening – Früherkennung von Vitamin-B12-Mangel im Fokus
Pädiatrie & Pädologie (2021)
-
Neonatal and carrier screening for rare diseases: how innovation challenges screening criteria worldwide
Journal of Community Genetics (2021)