Abstract
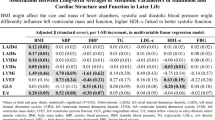
The purpose of the present study was to elucidate the cardiac structure and function in patients who have metabolic syndrome but no history of cardiovascular disease by analyzing echocardiographic findings. Echocardiographic examination was performed to screen for cardiovascular disease in 135 patients who were in their sixties. Patients were divided into metabolic syndrome (n=65, age: 65±2.7 years) and non–metabolic syndrome (n=70, age: 66±2.5 years) groups based on the criteria for metabolic syndrome proposed by the Japanese Society of Hypertension and seven other societies in 2005. The left ventricular (LV) wall thickness and dimension were measured by M-mode echocardiography. The relative wall thickness, LV mass index, and LV ejection fraction (LVEF) were calculated. LV diastolic function was assessed by the peak velocity of early rapid filling (E velocity) and the peak velocity of atrial filling (A velocity), and the ratio of E to A (E/A) was assessed by the transmitral flow. The Tei index, which reflects both LV diastolic and systolic function, was also calculated. There were no differences in relative wall thickness, LV mass index, or LVEF between the two groups. However, both the E/A and Tei index were significantly different between the metabolic syndrome (0.66±0.14 and 0.36±0.07, respectively) and non–metabolic syndrome (0.88±0.25 and 0.29±0.09) groups (p<0.001). These results indicate that patients with metabolic syndrome can have cardiac diastolic dysfunction even if they have neither LV hypertrophy nor systolic dysfunction.
Similar content being viewed by others
Article PDF
References
Hunt SA, Abraham WT, Chin MH, et al: ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult—summary article. Circulation 2005; 112: 1825–1852.
Lakka HM, Laaksonen DE, Lakka TA, et al: The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA 2002; 288: 2709–2716.
Takeuchi H, Saitoh S, Takagi S, et al: Metabolic syndrome and cardiac disease in Japanese men: applicability of the concept of metabolic syndrome defined by the National Cholesterol Education Program–Adult Treatment Panel III to Japanese men—the Tanno and Sobetsu Study. Hypertens Res 2005; 28: 203–208.
Tsubakimoto A, Saito I, Mannami T, et al: Impact of metabolic syndrome on brachial-ankle pulse wave velocity in Japanese. Hypertens Res 2006; 29: 29–37.
Nakanishi N, Shiraishi T, Wada M : Brachial-ankle pulse wave velocity and metabolic syndrome in a Japanese population: the Minoh study. Hypertens Res 2005; 28: 125–131.
Ishizaka N, Ishizaka Y, Toda E, Hashimoto H, Nagai R, Yamakado M : Hypertension is the most common component of metabolic syndrome and the greatest contributor to carotid arteriosclerosis in apparently healthy Japanese individuals. Hypertens Res 2005; 28: 27–34.
Imai Y, Otsuka K, Kawano Y, et al: Japanese Society of Hypertension (JSH) guidelines for self-monitoring of blood pressure at home. Hypertens Res 2003; 26: 771–782.
Japan Diabetes Society : Guidelines for diagnosis of diabetes mellitus. J Jpn Diabetes Soc 1999; 42: 385–404.
Hata Y, Mabuchi H, Saito Y, et al: Report of the Japan Atherosclerosis Society (JAS) guideline for diagnosis and treatment of hyperlipidemia in Japanese adults. J Atheroscler Thromb 2002; 9: 1–27.
Examination Committee of Criteria for Metabolic Syndrome : Definition and criteria for metabolic syndrome. J Jpn Soc Intern Med 2005; 94: 794–809 ( in Japanes).
Sahn DJ, DeMaria A, Kisslo J, Weyman A : Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation 1978; 58: 1072–1083.
Schiller NB, Shah PM, Crawford M, et al: Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. J Am Soc Echocardiogr 1989; 2: 358–367.
Devereux RB, Wallerson DC : Reproducibility of echocardiographic left ventricular measurements. Hypertension 1987; 9 ( Suppl II): II-6–II-18.
Patel CD, Nadig MR, Kurien S, Barai S, Narang R, Malhotra A : Left ventricular ejection fraction and volumes on rest gated 201Tl perfusion SPECT: comparison with two-dimensional echocardiography. Nucl Med Commun 2006; 27: 425–429.
Appleton CP, Firstenberg MS, Garcia MJ, Thomas JD : The echo-Doppler evaluation of left ventricular diastolic function. A current perspective. Cardiol Clin 2000; 18: 513–546.
Poerner TC, Goebel B, Unglaub P, et al: Detection of a pseudonormal mitral inflow pattern: an echocardiographic and tissue Doppler study. Echocardiography 2003; 20: 345–356.
Tei C, Ling LH, Hodge DO, et al: New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function—a study in normals and dilated cardiomyopathy. J Cardiol 1995; 26: 357–366.
Tei C, Dujardin KS, Hodge DO, Kyle RA, Tajik AJ, Seward JB : Doppler index combining systolic and diastolic myocardial performance: clinical value in cardiac amyloidosis. J Am Coll Cardiol 1996; 28: 658–664.
Wong CY, O'Moore-Sullivan T, Fang ZY, Haluska B, Leano R, Marwick TH : Myocardial and vascular dysfunction and exercise capacity in the metabolic syndrome. Am J Cardiol 2005; 96: 1686–1691.
Grandi AM, Maresca AM, Giudici E, et al: Metabolic syndrome and morphofunctional characteristics of the left ventricle in clinically hypertensive nondiabetic subjects. Am J Hypertens 2006; 19: 199–205.
Zile MR, Brutsaert DL : New concepts in diastolic dysfunction and diastolic heart failure: Part II. Causal mechanisms and treatment. Circulation 2002; 105: 1503–1508.
Scognamiglio R, Avogaro A, Negut C, et al: Early myocardial dysfunction in the diabetic heart: current research and clinical applications. Am J Cardiol 2004; 93 ( 8A): 17A–20A.
Mizushige K, Yao L, Noma T, et al: Alteration in left ventricular diastolic filling and accumulation of myocardial collagen at insulin-resistant prediabetic stage of a type II diabetic rat model. Circulation 2000; 101: 899–907.
Bajraktari G, Koltai MS, Ademaj F, et al: Relationship between insulin resistance and left ventricular diastolic dysfunction in patients with impaired glucose tolerance and type 2 diabetes. Int J Cardiol 2006; 110: 206–211.
Horio T, Suzuki M, Suzuki K, et al: Pioglitazone improves left ventricular diastolic function in patients with essential hypertension. Am J Hypertens 2005; 18: 949–957.
Roman MJ, Ganau A, Saba PS, Pini R, Pickering TG, Devereux RB : Impact of arterial stiffening on left ventricular structure. Hypertension 2000; 36: 489–494.
Moulopoulos SD, Stamatelopoulos SF, Zakopoulos NA, et al: Effect of 24-hour blood pressure and heart rate variations on left ventricular hypertrophy and dilation in essential hypertension. Am Heart J 1990; 119: 1147–1152.
Aeschbacher BC, Hutter D, Fuhrer J, Weidmann P, Delacretaz E, Allemann Y : Diastolic dysfunction precedes myocardial hypertrophy in the development of hypertension. Am J Hypertens 2001; 14: 106–113.
Chang NC, Lai ZY, Wang TC : Enalapril does not improve left ventricular diastolic dysfunction in young and mild hypertensives without concomitant hypertrophy. Am J Hypertens 1996; 14: 909–914.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Masugata, H., Senda, S., Goda, F. et al. Left Ventricular Diastolic Dysfunction as Assessed by Echocardiography in Metabolic Syndrome. Hypertens Res 29, 897–903 (2006). https://doi.org/10.1291/hypres.29.897
Received:
Accepted:
Issue date:
DOI: https://doi.org/10.1291/hypres.29.897
Keywords
This article is cited by
-
Regional myocardial function abnormalities are associated with macro- and microcirculation dysfunction in the metabolic syndrome: the RESOLVE study
Heart and Vessels (2018)
-
Effects of Metformin and Exercise Training, Alone or in Combination, on Cardiac Function in Individuals with Insulin Resistance
Cardiology and Therapy (2016)
-
Diastolic dysfunction in the diabetic continuum: association with insulin resistance, metabolic syndrome and type 2 diabetes
Cardiovascular Diabetology (2015)
-
Cardiac steatosis and left ventricular function in men with metabolic syndrome
Journal of Cardiovascular Magnetic Resonance (2013)
-
QTLs of factors of the metabolic syndrome and echocardiographic phenotypes: the hypertension genetic epidemiology network study
BMC Medical Genetics (2008)