Abstract
There is increasing evidence that aldosterone exerts major adverse cardiovascular effects through classical mineralocorticoid receptors (MR) in nonepithelial tissues such as the brain and heart. This nonepithelial role of aldosterone has been underscored by the recent Randomized Aldactone Evaluation Study (RALES) and the Eplerenone Post-AMI Heart Failure Efficacy and Survival Study (EPHESUS). These studies also showed that when using MR antagonist as an “organ protecting” drug, further organ protection could be derived by the addition of an angiotensin-converting enzyme (ACE) inhibitor or angiotensin II type 1 receptor blocker (ARB). The long-term effect of aldosterone was not inhibited in some subjects, so the possibility of organ damage due to so-called “breakthrough” aldosterone cannot be ignored. Nonepithelial MR–mediated effects played a major role in this aldosterone effect. These effects can be inhibited by MR antagonist at a small dose, not lower blood pressure. Therefore, the idea is now to combine a small dose of MR antagonist with an ACE inhibitor or ARB. However, warnings have been given recently due to the emergence of hyperkalemia and other adverse effects associated with inappropriate combination therapy. It is important to note that, if the eligibility criteria of RALES and EPHESUS are fulfilled, the potassium level will rarely become problematic. Therefore, the recent increase in the incidence of adverse effects can be attributed to the incorrect application of combination therapy. Elderly patients or those with dehydration, renal dysfunction, and aggravated heart failure require further close monitoring or termination of spironolactone administration. The combination of an MR antagonist and renin-angiotensin inhibitors should be a useful strategy if subjects are carefully selected, and carefully monitored. Adverse effects will occur only if the usage recommendations based on previous researches are not followed.
Similar content being viewed by others
Article PDF
References
Pitt B, Zannad F, Remme WJ, et al, for the Randomized Aldactone Evaluation Study : The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med 1999; 341: 709–717.
Pitt B, Remme W, Zannad F, et al, for the Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival Study Investigators : Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med 2003; 348: 1309–1321.
Juurlink DN, Mamdani MM, Lee DS, et al: Rates of hyperkalemia after publication of the Randomized Aldactone Evaluation Study. N Engl J Med 2004; 351: 543–551.
Sligl W, McAlister FA, Ezekowitz J, Armstrong PW : Usefulness of spironolactone in a specialized heart failure clinic. Am J Cardiol 2004; 94: 443–447.
Greenberg B : Treatment of heart failure: state of the art and prospectives. J Cardiovasc Pharmacol 2002; 38: 59–63.
Remme WJ, Swedberg K : Comprehensive guideline for the diagnosis and treatment of chronic heart failure. Eur J Heart Fail 2002; 4: 11–22.
Rocha R, Funder JW : The pathophysiology of aldosterone in the cardiovascular system. Ann N Y Acad Sci 2002; 970: 89–100.
Young M, Head G, Funder JW : Determinants of cardiac fibrosis in experimental hypermineralocorticoid states. Am J Physiol 1995; 269: 657–662.
Brilla CG, Weber KT : Mineralocorticoid excess, dietary sodium and myocardial fibrosis. J Lab Clin Med 1992; 120: 893–901.
Funder JW : Aldosterone, salt and cardiac fibrosis. Clin Exp Hypertens 1997; 19: 885–899.
Sato A, Saruta T : Aldosterone-induced organ damage: plasma aldosterone level and inappropriate salt status. Hypertens Res 2004; 27: 303–310.
Funder JW : Is aldosterone bad for the heart? Trends Endocrinol Metab 2004; 15: 139–142.
Sato A, Suzuki Y, Saruta T : Effects of spironolactone and angiotensin-converting enzyme inhibitor on left ventricular hypertrophy in patients with essential hypertension. Hypertens Res 1999; 22: 17–27.
The RALES Investigators : Effectiveness of spironolactone added to an angiotensin-converting enzyme inhibitor and a loop diuretic for severe chronic congestive heart failure (the Randomized Aldactone Evaluation Study). Am J Cardiol 1996; 78: 902–907.
Sato A, Saruta T : Aldosterone escape during angiotensin-converting enzyme inhibitor therapy in essential hypertensive patients with left ventricular hypertrophy. J Int Med Res 2001; 29: 13–21.
Sato A, Hayashi K, Naruse M, Saruta T : Effectiveness of aldosterone blockade in patients with diabetic nephropathy. Hypertension 2003; 41: 64–68.
Sato A, Saruta T : Aldosterone breakthrough during angiotensin-converting enzyme inhibitor therapy. Am J Hypertens 2003; 16: 781–788.
van Vliet AA, Donker AJM, Nauta JJP, Verheugt FWA : Spironolactone in congestive heart failure refractory to high-dose loop diuretic and low-dose angiotensin-converting enzyme inhibitor. Am J Cardiol 1993; 71: 21A–28A.
Barr CS, Lang CC, Hanson J, Arnott M, Kennedy N, Struthers AD : Effects of adding spironolactone to an angiotensin-converting enzyme inhibitor in chronic congestive heart failure secondary to coronary artery disease. Am J Cardiol 1995; 76: 1259–1265.
Fung JWH, Yu CM, Yip G, et al: Effect of beta blockade (carvedilol or metoprolol) on activation of the renin-angiotensin-aldosterone system and natriuretic peptides in chronic heart failure. Am J Cardiol 2003; 92: 406–410.
Pitt B, Reichek N, Willenbrock R, et al: Effects of eplerenone, enalapril, and eplerenone/enalapril in patients with essential hypertension and left ventricular hypertrophy: the 4E-left ventricular hypertrophy study. Circulation 2003; 108: 1831–1838.
Sato A, Hayashi K, Saruta T : Antiproteinuric effects of mineralocorticoid receptor blockade in patients with chronic renal disease. Am J Hypertens 2005; 18: 44–49.
Cohn JN, Anand IS, Latini R, et al, for Valsartan Heart Failure Trial Investigators : Sustained reduction of aldosterone in response to the angiotensin receptor blocker valsartan in patients with chronic heart failure: results from the Valsartan Heart Failure Trial. Circulation 2003; 108: 1306–1309.
McKlelvie RS, Yusuf S, Mmath P, et al, The RESOLVD Pilot Study Investigators : Comparison of candesartan, enalapril, and their combination in congestive heart failure. Randomized Evaluation of Strategies for Left Ventricular Dysfunction (RESOLVD) pilot study. Circulation 1999; 100: 1056–1064.
Azizi M, Menard J : Combined blockade of the renin-angiotensin system with angiotensin-converting enzyme inhibitors and angiotensin II type 1 receptor antagonists. Circulation 2004; 109: 2492–2499.
Bozkurt B, Agoston I, Knowlton AA : Complications of inappropriate use of spironolactone in heart failure: when an old medicine spirals out of new guidelines. J Am Coll Cardiol 2003; 41: 211–214.
Svensson M, Gustafsson F, Galatius S, Hildebrandt PR, Atar D : Hyperkalemia and impaired renal function in patients taking spironolactone for congestive heart failure: retrospective study. BMJ 2003; 327: 1141–1142.
Wrenger E, Muller R, Moesenthin M, Welte T, Frolich JC, Neumann KH : Interaction of spironolactone with ACE inhibitors or angiotensin receptor blockers: analysis of 44 cases. BMJ 2003; 327: 147–149.
Schepkens H, Vanholder R, Billiouw JM, Lameire N : Life-threatening hyperkalemia during combined therapy with angiotensin-converting enzyme inhibitors and spironolactone: an analysis of 25 cases. Am J Med 2001; 110: 438–441.
Tamirisa KP, Aaronson KD, Koelling TM : Spironolactone-induced renal insufficiency and hyperkalemia in patients with heart failure. Am Heart J 2004; 148: 971–978.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sato, A., Saruta, T. & Funder, J. Combination Therapy with Aldosterone Blockade and Renin-Angiotensin Inhibitors Confers Organ Protection. Hypertens Res 29, 211–216 (2006). https://doi.org/10.1291/hypres.29.211
Received:
Accepted:
Issue date:
DOI: https://doi.org/10.1291/hypres.29.211
Keywords
This article is cited by
-
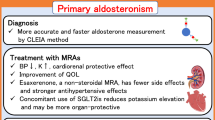
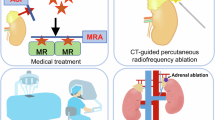
Management of primary aldosteronism and mineralocorticoid receptor-associated hypertension
Hypertension Research (2020)
-
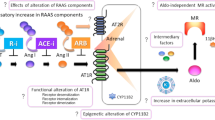
Pathophysiological mechanisms of mineralocorticoid receptor-dependent cardiovascular and chronic kidney disease
Hypertension Research (2019)
-
The necessity and effectiveness of mineralocorticoid receptor antagonist in the treatment of diabetic nephropathy
Hypertension Research (2015)
-
Salt controls endothelial and vascular phenotype
Pflügers Archiv - European Journal of Physiology (2015)
-
Mineralocorticoid receptor antagonists: their use and differentiation in Japan
Hypertension Research (2013)