Abstract
Angiotensin receptor blockers (ARBs) are the recommended first-line antihypertensive treatment for managing chronic kidney disease, and strict blood pressure (BP) regulation is crucial for the reduction of proteinuria. Valsartan and candesartan are commonly used ARBs in Japan, with maximum permissible doses of 160 mg/day and 12 mg/day, respectively. We evaluated BP and proteinuria after changeover from the maximum dose of candesartan to the maximum dose of valsartan, in 55 poorly controlled hypertensive patients undergoing candesartan treatment who were unable to achieve optimal BP according to the Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2004). We measured BP and pulse rate and assessed urinary protein excretion (UPE) before and after changeover. Changeover was associated with decreases in systolic BP and diastolic BP from 158/89 mmHg to 150/86 mmHg (p<0.01). Changeover was also associated with a reduction in UPE adjusted to urinary creatinine from 0.35±0.19 g/g creatinine to 0.19±0.37 g/g creatinine (p=0.0271) in patients who had high urinary protein levels prior to changeover without significant decreases in BP (p=0.0184). According to multiple regression analysis, higher UPE (p<0.0001) and a lower glomerular filtration rate (GFR) (p=0.0011) prior to changeover were independently correlated with reduction in UPE. Our results suggest that the maximum dose of valsartan is more effective than the maximum dose of candesartan for reducing BP and proteinuria.
Similar content being viewed by others
Article PDF
References
Peralta CA, Kurella M, Lo JC, Chertow GM : The metabolic syndrome and chronic kidney disease. Curr Opin Nephrol Hypertens 2006; 15: 361–365.
Segura J, Campo C, Gil P, et al: Development of chronic kidney disease and cardiovascular prognosis in essential hypertensive patients. J Am Soc Nephrol 2004; 15: 1616–1622.
De Leeuw PW, Thijs L, Birkenhager WH, et al: Prognostic significance of renal function in elderly patients with isolated systolic hypertension: results from the Syst-Eur trial. J Am Soc Nephrol 2002; 13: 2213–2222.
Marin R, Gorostidi M, Fernandez-Vega F, Alvarez-Navascues R : Systemic and glomerular hypertension and progression of chronic renal disease: the dilemma of nephrosclerosis. Kidney Int Suppl 2005; ( 99): S52–S56.
Hayashi K, Wakino S, Homma K, Sugano N, Saruta T : Pathophysiological significance of T-type Ca2+ channels: role of T-type Ca2+ channels in renal microcirculation. J Pharmacol Sci 2005; 99: 221–227.
Wang T, Takabatake T : Effects of vasopeptidase inhibition on renal function and tubuloglomerular feedback in spontaneously hypertensive rats. Hypertens Res 2005; 28: 611–618.
Caldicott WJ, Taub KJ, Margulies SS, Hollenberg NK : Angiotensin receptors in glomeruli differ from those in renal arterioles. Kidney Int 1981; 19: 687–693.
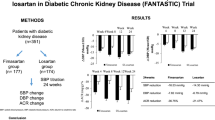
Brenner BM, Cooper ME, de Zeeuw D, et al: Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med 2001; 345: 861–869.
Ruggenenti P, Perna A, Loriga G, et al: Blood-pressure control for renoprotection in patients with non-diabetic chronic renal disease (REIN-2): multicentre, randomised controlled trial. Lancet 2005; 365: 939–946.
Julius S, Kjeldsen SE, Weber M, et al: Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trial. Lancet 2004; 363: 2022–2031.
Parving HH, Lehnert H, Brochner-Mortensen J, et al: The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. N Engl J Med 2001; 345: 870–878.
Fujikawa K, Hasebe N, Kikuchi K : Cost-effectiveness analysis of hypertension treatment: controlled release nifedipine and candesartan low-dose combination therapy in patients with essential hypertension—the Nifedipine and Candesartan Combination (NICE-Combi) Study. Hypertens Res 2005; 28: 585–591.
Pfeffer MA, Swedberg K, Granger CB, et al: Effects of candesartan on mortality and morbidity in patients with chronic heart failure: the CHARM-Overall programme. Lancet 2003; 362: 759–766.
Cohn JN, Tognoni G : A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med 2001; 345: 1667–1675.
Pfeffer MA, McMurray JJ, Velazquez EJ, et al: Valsartan, captopril, or both in myocardial infarction complicated by heart failure, left ventricular dysfunction, or both. N Engl J Med 2003; 349: 1893–1906.
Imai E, Horio M, Nitta K, et al: Estimation of glomerular filtration rate by the MDRD study equation modified for Japanese patients with chronic kidney disease. Clin Exp Nephrol 2007; 11: 41–50.
Fogari R, Mugellini A, Zoppi A, et al: A double-blind crossover study of the antihypertensive efficacy of angiotensin II–receptor antagonists and their activationof the renin-angiotensin system. Curr Ther Res Clin Exp 2000; 61: 669–679.
Guidelines Committee : 2003 European Society of Hypertension–European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens 2003; 21: 1011–1053.
Chobanian AV, Bakris GL, Black HR, et al: The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289: 2560–2572.
The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group: Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002; 288: 2981–2997.
Peterson JC, Adler S, Burkart JM, et al: Blood pressure control, proteinuria, and the progression of renal disease. The Modification of Diet in Renal Disease Study. Ann Intern Med 1995; 123: 754–762.
Weinberg M, Weinberg A, Cord R, Zappe D : The effect of high-dose angiotensin II receptor blockade beyond maximal recommended doses in reducing urinary protein excretion. JRAAS 2001; 2: S196–S198.
Hollenberg NK, Parving HH, Viberti G, Remuzzi G : The Diovan Reduction of Proteinuiria (DROP) Study: albuminuria response to high-doses of valsartan in type 2 diabetes mellitus. Circulation 2006; 114: II-61.
Lithell H, Hansson L, Skoog I, et al: The Study on Cognition and Prognosis in the Elderly (SCOPE): principal results of a randomized double-blind intervention trial. J Hypertens 2003; 21: 875–886.
Suzuki H, Kanno Y : Effects of candesartan on cardiovascular outcomes in Japanese hypertensive patients. Hypertens Res 2005; 28: 307–314.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ohishi, M., Takagi, T., Ito, N. et al. Renal Protective Effect in Hypertensive Patients: The High Doses of Angiotensin II Receptor Blocker (HARB) Study. Hypertens Res 30, 1187–1192 (2007). https://doi.org/10.1291/hypres.30.1187
Received:
Accepted:
Issue date:
DOI: https://doi.org/10.1291/hypres.30.1187
Keywords
This article is cited by
-
Is the reno-protective effect of valsartan dose dependent? A comparative study of 80 and 160 mg day−1
Hypertension Research (2010)
-
Strong suppression of the renin–angiotensin system has a renal-protective effect in hypertensive patients: High-dose ARB with ACE inhibitor (Hawaii) study
Hypertension Research (2010)