Abstract
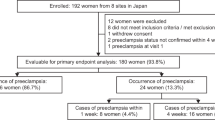
It has been established that serum soluble endoglin (sEng) increases in women with preeclampsia. However, sEng levels have not been evaluated using a normal reference value specific to each gestational age. First, we established the normal reference value for sEng using 85 pregnant controls without preeclampsia, from whom serum samples were collected three times at 20–23, 27–30, and 36–38 weeks of gestation. Second, we evaluated the serum sEng levels after the onset of preeclampsia in 56 preeclamptic patients. In three women (3.5%) with normal pregnancies, sustained high sEng levels (>15 ng/mL) were observed. We calculated the reference value for sEng using the remaining 82 normal controls. The log10sEng was almost normally distributed at each gestational week during 20–38 weeks, and the mean log10sEng was represented as a quadratic curve of gestational week. The SD of log10sEng was represented as a linear equation of gestational week. The mean log10sEng significantly and gradually increased from 20–23 weeks to 27–30 weeks of gestation and then rapidly increased at 36–38 weeks of gestation. Ninety-three percent of preeclamptic women showed sEng≥95th percentile of the reference value. The log10sEng levels and the SD score (SDS) of log10sEng in women with early-onset preeclampsia (onset<32 weeks of gestation) were significantly higher than those in women with late-onset preeclampsia (onset≥32 weeks of gestation) (1.97±0.23 vs. 1.78±0.28, 9.94±2.61 vs. 4.47±2.06, respectively). In conclusion, alteration of serum sEng levels after the onset of preeclampsia was more pronounced in women with early-onset preeclampsia compared to those with late onset.
Similar content being viewed by others
Article PDF
References
Ohkuchi A, Iwasaki R, Suzuki H, et al: Normal and high-normal blood pressures, but not body mass index, are risk factors for the subsequent occurrence of both preeclampsia and gestational hypertension: a retrospective cohort study. Hypertens Res 2006; 29: 161–167.
Nagaya K, Fetters MD, Ishikawa M, et al: Causes of maternal mortality in Japan. JAMA 2000; 283: 2661–2667.
Hecher K, Campbell S, Doyle P, Harrington K, Nicolaides K : Assessment of fetal compromise by Doppler ultrasound investigation of the fetal circulation. Arterial, intracardiac, and venous blood flow velocity studies. Circulation 1995; 91: 129–138.
Maruyama A, Nakayama T, Sato N, Mizutani Y, Furuya K, Yamamoto T : Association study using single nucleotide polymorphisms in the estrogen receptor beta (ESR2) gene for preeclampsia. Hypertens Res 2004; 27: 903–909.
Chappell S, Morgan L : Searching for genetic clues to the causes of pre-eclampsia. Clin Sci (Lond) 2006; 110: 443–458.
Molvarec A, Vér A, Fekete A, et al: Association between estrogen receptor α (ESR1) gene polymorphisms and severe preeclampsia. Hypertens Res 2007; 30: 205–211.
Levine RJ, Maynard SE, Qian C, et al: Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med 2004; 350: 672–683.
Maynard SE, Min JY, Merchan J, et al: Excess placental soluble fms-like tyrosine kinase 1 (sF1t1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Invest 2003; 111: 649–658.
Ohkuchi A, Hirashima C, Matsubara S, et al: Alterations in placental growth factor levels before and after the onset of preeclampsia are more pronounced in women with early onset severe preeclampsia. Hypertens Res 2007; 30: 151–159.
Hirashima C, Ohkuchi A, Arai F, et al: Establishing reference values for both total soluble fms-like tyrosine kinase 1 and free placental growth factor in pregnant women. Hypertens Res 2005; 28: 727–732.
Chaiworapongsa T, Romero R, Kim YM, et al: Plasma soluble vascular endothelial growth factor receptor-1 concentration is elevated prior to the clinical diagnosis of preeclampsia. J Matern Fetal Neonatal Med 2005; 17: 3–18.
Venkatesha S, Toporsian M, Lam C, et al: Soluble endoglin contributes to the pathogenesis of preeclampsia. Nat Med 2006; 12: 642–649.
Levine RJ, Lam C, Qian C, et al: CPEP Study Group: Soluble endoglin and other circulating antiangiogenic factors in preeclampsia. N Engl J Med 2006; 355: 992–1005.
Lebrin F, Deckers M, Bertolino P, Ten Dijke P : TGF-beta receptor function in the endothelium. Cardiovasc Res 2005; 65: 599–608.
Masuyama H, Nakatsukasa H, Takamoto N, Hiramatsu Y : Correlation between soluble endoglin, vascular endothelial growth factor receptor-1, and adipocytokines in preeclampsia. J Clin Endocrinol Metab 2007; 92: 2672–2679.
Salahuddin S, Lee Y, Vadnais M, Sachs BP, Karumanchi SA, Lim KH : Diagnostic utility of soluble fms-like tyrosine kinase 1 and soluble endoglin in hypertensive diseases of pregnancy. Am J Obstet Gynecol 2007; 197: 28.e 1–28.e6.
Staff AC, Braekke K, Johnsen GM, Karumanchi SA, Harsem NK : Circulating concentrations of soluble endoglin (CD105) in fetal and maternal serum and in amniotic fluid in preeclampsia. Am J Obstet Gynecol 2007; 197: 176.e1–176.e6.
Sato K : A proposal for a new definition and classification of “Pregnancy Induced Hypertension (PIH)” (2004), in Japan Society for the Study of Toxemia of Pregnancy (ed): Historical Perspective of Study of Pregnancy-Induced Hypertension in Japan. Tokyo, Medical View Co, 2005, 54–87.
Ogawa Y, Iwamura T, Kuriya N, et al: Birth size standards by gestational age for Japanese neonates. Acta Neonatologica Japonica 1998; 34: 624–632.
Rana S, Karumanchi SA, Levine RJ, et al: Sequential changes in antiangiogenic factors in early pregnancy and risk of developing preeclampsia. Hypertension 2007; 50: 137–142.
Robinson CJ, Johnson DD : Soluble endoglin as a second-trimester marker for preeclampsia. Am J Obstet Gynecol 2007; 197: 174.e1–174.e5.
Lopez-Novoa JM : Soluble endoglin is an accurate predictor and a pathogenic molecule in pre-eclampsia. Nephrol Dial Transplant 2007; 22: 712–714.
Lowe DT : Nitric oxide dysfunction in the pathophysiology of preeclampsia. Nitric Oxide 2000; 4: 441–458.
Cudmore M, Ahmad S, Al-Ani B, et al: Negative regulation of soluble Flt-1 and soluble endoglin release by heme oxygenase-1. Circulation 2007; 115: 1789–1797.
Ahmed A, Rahman M, Zhang X, et al: Induction of placental heme oxygenase-1 is protective against TNFalpha-induced cytotoxicity and promotes vessel relaxation. Mol Med 2000; 6: 391–409.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hirashima, C., Ohkuchi, A., Matsubara, S. et al. Alteration of Serum Soluble Endoglin Levels after the Onset of Preeclampsia Is More Pronounced in Women with Early-Onset. Hypertens Res 31, 1541–1548 (2008). https://doi.org/10.1291/hypres.31.1541
Received:
Accepted:
Issue date:
DOI: https://doi.org/10.1291/hypres.31.1541
Keywords
This article is cited by
-
The role of endoglin and its soluble form in pathogenesis of preeclampsia
Molecular and Cellular Biochemistry (2022)
-
Cerebrospinal beta-amyloid peptides(1-40) and (1-42) in severe preeclampsia and HELLP syndrome – a pilot study
Scientific Reports (2020)
-
An Insight into the Angiogenic and Lymphatic Interplay in Pre-eclampsia Comorbid with HIV Infection
Current Hypertension Reports (2020)
-
Galectin-1 as a novel risk factor for both gestational hypertension and preeclampsia, specifially its expression at a low level in the second trimester and a high level after onset
Hypertension Research (2018)
-
Prediction and prevention of hypertensive disorders of pregnancy
Hypertension Research (2017)