Abstract
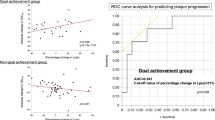
Although many clinical studies have evaluated plaque growth in response to positive or negative remodeling in coronary arteries using intravascular ultrasound (IVUS), little is known about the associations between metabolic factors and coronary plaque growth or remodeling. In this cross-sectional study, we analyzed 100 consecutive patients with stable angina who had undergone preinterventional IVUS. The characteristics of coronary plaque (plaque area [PA] and volume [PV]) and remodeling patterns were analyzed by IVUS. Patients were divided into two groups: a positive remodeling (P) group (remodeling index [RI]>1.0, n=37) and a non–positive remodeling (NP) group (RI≤1.0, n=63). Patient characteristics, including age, gender, body mass index and angiographic variables, were similar between the two groups. Interestingly, plasma adiponectin levels in the P group were significantly lower than those in the NP group. The remodeling classification was most closely associated with plasma adiponectin levels (p=0.006) among the metabolic factors. Although there were no significant correlations between RI and %PA or %PV, and although %PA but not %PV in the P group was significantly higher than that in the NP group, %PV was significantly associated with plasma low-density lipoprotein cholesterol (LDL-C) and diastolic blood pressure, but not adiponectin, in all patients. In addition, higher %PV was most closely correlated with higher plasma LDL-C (p=0.009) among metabolic factors. In conclusion, among the metabolic factors examined, plasma adiponectin levels may be critical for arterial remodeling, while higher levels of LDL-C may be most useful for predicting PV.
Similar content being viewed by others
Article PDF
References
Glagov S, Weisenberg E, Zarins CK, et al: Compensatory enlargement of human atherosclerotic coronary arteries. N Engl J Med 1987; 316: 1371–1375.
Hermiller JB, Tenaglia AN, Kisslo KB, et al: In vivo validation of compensatory enlargement of atherosclerotic coronary arteries. Am J Cardiol 1993; 71: 665–668.
Losordo DW, Rosenfield K, Kaufman J, et al: Focal compensatory enlargement of human arteries in response to progressive atherosclerosis. In vivo documentation using intravascular ultrasound. Circulation 1994; 89: 2570–2577.
Katayama T, Kubo N, Takagi Y, et al: Relation of atherothrombosis burden and volume detected by intravascular ultrasound to angiographic no-reflow phenomenon during stent implantation in patients with acute myocardial infarction. Am J Cardiol 2006; 97: 301–304.
Pasterkamp G, Wensing PJ, Post MJ, et al: Paradoxical arterial wall shrinkage may contribute to luminal narrowing of human atherosclerotic femoral arteries. Circulation 1995; 91: 1444–1449.
Mintz GS, Kent KM, Pichard AD, et al: Contribution inadequate arterial remodeling to the development of focal coronary artery stenoses. An intravascular ultrasound study. Circulation 1997; 95: 1791–1798.
Kimura T, Kaburagi S, Tamura T, et al: Remodeling human coronary arteries undergoing coronary angioplasty or atherectomy. Circulation 1997; 96: 475–483.
Schoenhagen P, Ziada KM, Kapadia SR, et al: Extent and direction of arterial remodeling in stable versus unstable coronary syndromes: an intravascular ultrasound study. Circulation 2000; 101: 598–603.
Koji Y, Tomiyama H, Yamada J, et al: Relationship between arterial stiffness and the risk of coronary artery disease in subjects with and without metabolic syndrome. Hypertens Res 2007; 30: 243–247.
Lakka HM, Laaksonen DE, Lakka TA, et al: The metabolic syndrome and total and cardiovascular disease mortality middle-aged men. JAMA 2002; 288: 2709–2716.
Nakamura Y, Shimada K, Fukuda D, et al: Implications plasma concentrations of adiponectin in patients with coronary artery disease. Heart 2004; 90: 528–533.
Otsuka F, Sugiyama S, Kojima S, et al: Plasma adiponectin levels are associated with coronary lesion complexity men with coronary artery disease. J Am Coll Cardiol 2006; 48: 1155–1162.
Gronenschild E, Janssen J, Tijdens F : CAAS. II: A second generation system for off-line and on-line quantitative coronary angiography. Cathet Cardiovasc Diagn 1994; 33: 61–75.
Arita Y, Kihara S, Ouchi N, et al: Paradoxical decrease an adipose-specific protein, adiponectin, in obesity. Biochem Biophys Res Commun 1999; 257: 79–83.
Kojima S, Funahashi T, Maruyoshi H, et al: Levels of the adipocyte-derived plasma protein, adiponectin, have a close relationship with atheroma. Thromb Res 2005; 115: 483–490.
Ouchi N, Kihara S, Arita Y, et al: Novel modulator for endothelial adhesion molecules: adipocyte-derived plasma protein adiponectin. Circulation 1999; 100: 2473–2476.
Nakamura M, Nishikawa H, Mukai S, et al: Impact of coronary artery remodeling on clinical presentation of coronary artery disease: an intravascular ultrasound study. J Am Coll Cardiol 2001; 37: 63–69.
Ehara S, Kobayashi Y, Yoshiyama M, et al: Spotty calcification typifies the culprit plaque in patients with acute myocardial infarction: an intravascular ultrasound study. Circulation 2004; 110: 3424–3429.
Maehara A, Mintz GS, Bui AB, et al: Morphologic and angiographic features of coronary plaque rupture detected by intravascular ultrasound. J Am Coll Cardiol 2002; 40: 904–910.
Kotani J, Mintz GS, Castagna MT, et al: Intravascular ultra-sound analysis of infarct-related and non-infarct-related arteries in patients who presented with an acute myocardial infarction. Circulation 2003; 107: 2889–2893.
Ouchi N, Kihara S, Arita Y, et al: Adipocyte-derived plasma protein, adiponectin, suppresses lipid accumulation and class A scavenger receptor expression in human monocyte- derived macrophages. Circulation 2001; 103: 1057–1063.
Okamoto Y, Kihara S, Ouchi N, et al: Adiponectin reduces atherosclerosis in apolipoprotein E–deficient mice. Circulation 2002; 106: 2767–2770.
Kumada M, Kihara S, Ouchi N, et al: Adiponectin specifically increased tissue inhibitor of metalloproteinase-1 through interleukin-10 expression in human macrophages. Circulation 2004; 109: 2046–2049.
Kojima S, Funahashi T, Sakamoto T, et al: The variation of plasma concentrations of a novel, adipocyte derived protein, adiponectin, in patients with acute myocardial infarction. Heart 2003; 89: 667–668.
Folsom AR, Wu KK, Rosamond WD, et al: Prospective study of hemostatic factors and incidence of coronary heart disease: the Atherosclerosis Risk in Communities (ARIC) Study. Circulation 1997; 96: 1102–1108.
Nakano Y, Tajima S, Yoshimi A, et al: A novel enzymelinked immunosorbent assay specific for high-molecular-weight adiponectin. J Lipid Res 2006; 47: 1572–1582.
Furuya R, Odamaki M, Kumagai H, et al: Impact of angiotensin II receptor blocker on plasma levels of adiponectin and advanced oxidation protein products in peritoneal dialysis patients. Blood Purif 2006; 24: 445–450.
Chujo D, Yagi K, Asano A, et al: Telmisartan treatmentdecreases visceral fat accumulation and improves serum levels of adiponectin and vascular inflammation markers in Japanese hypertensive ptients. Hypertens Res 2007; 30: 1205–1210.
Sacks FM, Pfeffer MA, Moye LA, et al: The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N Engl J Med 1996; 335: 1001–1009.
Serruys PW, de Feyter P Macaya C, et al: Fluvastatin for prevention of cardiac events following successful first percutaneous coronary intervention: a randomized controlled trial. JAMA 2002; 287: 3215–3222.
Jensen LO, Thayssen P, Pedersen KE, et al: Regression of coronary atherosclerosis by simvastatin: a serial intravascular ultrasound study. Circulation 2004; 110: 265–270.
Nicholls SJ, Tuzcu EM, Schoenhagen P, et al: Effect of atorvastatin (80 mg/day) versus pravastatin (40 mg/day) on arterial remodeling at coronary branch points (from the REVERSAL study). Am J Cardiol 2005; 96: 1636–1639.
von Birgelen C, Hartmann M, Mintz GS, et al: Relation between progression and regression of atherosclerotic left main coronary artery disease and serum cholesterol levels as assessed with serial long-term (≥12 months) follow-up intravascular ultrasound. Circulation 2003; 108: 2757–2762.
Iwata A, Miura S, Shirai K, et al: Lower level of low-density lipoprotein cholesterol by statin prevents progression of coronary restenosis after successful stenting in acute myocardial infarction. Intern Med 2006; 45: 885–890.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Iwata, A., Miura, Si., Mori, K. et al. Associations between Metabolic Factors and Coronary Plaque Growth or Arterial Remodeling as Assessed by Intravascular Ultrasound in Patients with Stable Angina. Hypertens Res 31, 1879–1886 (2008). https://doi.org/10.1291/hypres.31.1879
Received:
Accepted:
Issue date:
DOI: https://doi.org/10.1291/hypres.31.1879