Abstract
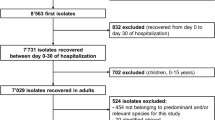
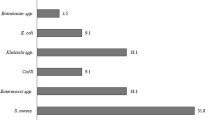
The hospital infection control team (ICT) has a major role in suppressing or preventing infectious diseases. The purpose of this study was to investigate whether the work of the ICT had affected the antibiograms at the Kobe University Hospital in the past 3 years. The ICT’s works are as follows: (1) to monitor whether physicians are instructed in the use of broad-spectrum antibiotics; (2) to check whether measures for preventing the occurrence or spread of infectious disease are performed along with appropriate standard precautions; (3) to provide rapid communication with physicians in bacteremia cases and (4) reporting the antibiograms in the hospital. In addition, we investigated changes in the antibiograms every 6 months based on all materials. There were 193 physician interventions in 2010 and 491 in 2011. The representative isolated bacteria included no additional bacteria with lower susceptibilities found over the past 1.5 years compared with the initial 1.5 years in the 3-year investigation period. The ratio for performing two sets of blood culture tests in all blood culture tests showed an upward tendency from 58.1% in 2009 to 71.1% in 2010 and 80.3% in 2011 (r=0.995, P=0.063, b=0.089). In conclusion, since the introduction of an expanded ICT role, our data showed an increased antibiotic susceptibilities in bacteria such as Enteroccus faecalis and the total amount of hand disinfectant agents tended to increase year by year, even though direct statistical analyses could not easily be performed. Further observation may be necessary for a definitive evaluation of ICT activities.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Carlet, J. et al. Society’s failure to protect a precious resource: antibiotics. Lancet 378, 369–371 (2011).
Gordts, B. Models for the organisation of hospital infection control and prevention programmes. Clin. Microbiol. Infect. 11, S19–S23 (2005).
Neuhauser, M. M. et al. Antibiotic resistance among gram-negative bacilli in US intensive care units: implications for fluoroquinolone use. JAMA 289, 885–888 (2003).
Venberghe, A. et al. Surveillance of hospital-acquired infections in an intensive care department-the benefit of the full-time presence of an infection control nurse. J. Hosp. Infect. 52, 56–59 (2002).
Niwa, T. et al. Outcome measurement of extensive implementation of antimicrobial stewardship in patients receiving intravenous antibiotics in a Japanese university hospital. Int. J. Clin. Pract. 66, 999–1008 (2012).
Yassi, A., Bryce, E. A., Maultsaid, D., Lauscher, H. N. & Zhao, K. The impact of requiring completion of an online infection control course on health professionals' intentions to comply with infection control guidelines: a comparative study. Can. J. Infect. Dis. Med. Microbiol. 20, 15–19 (2009).
Sekimoto, M. et al. Impact of hospital accreditation on infection control programs in teaching hospitals in Japan. Am. J. Infect. Control 36, 212–219 (2008).
Gould, I. M. Antibiotic policies and control of resistance. Curr. Opin. Infect. Dis. 15, 395–400 (2002).
Joung, M. K. et al. Impact of de-escalation therapy on clinical outcomes for intensive care unit-acquired pneumonia. Crit. Care 15, R79 (2011).
Shime, N., Satake, S. & Fujita, N. De-escalation of antimicrobials in the treatment of bacteraemia due to antibiotic-sensitive pathogens in immunocompetent patients. Infection 39, 319–325 (2011).
Masterton, R. G. Antibiotic de-escalation. Crit. Care. Clin. 27, 149–162 (2011).
Chihara, S., Okuzumi, K., Yamamoto, Y., Oikawa, S. & Hishinuma, A. First case of New Delhi metallo-beta-lactamase 1-producing Escherichia coli infection in Japan. Clin. Infect. Dis. 52, 153–154 (2011).
Yamamoto, T., Takano, T., Iwao, Y. & Hishinuma, A. Emergence of NDM-1-positive capsulated Escherichia coli with high resistance to serum killing in Japan. J. Infect. Chemother. 17, 435–439 (2011).
Yamamoto, M. et al. Interspecies dissemination of a novel class 1 integron carrying blaIMP-19 among Acinetobacter species in Japan. J. Antimicrob. Chemother. 66, 2480–2483 (2011).
Lee, S. O. et al. Reduced use of third-generation cephalosporins decreases the acquisition of extended-spectrum beta-lactamase-producing Klebsiella pneumoniae. Infect. Control Hosp. Epidemiol. 25, 832–837 (2004).
Goddard, S. & Muller, M. P. The efficacy of infection control interventions in reducing the incidence of extended-spectrum β-lactamase-producing Enterobacteriaceae in the nonoutbreak setting: a systematic review. Am. J. Infect. Control 39, 599–601 (2011).
D'Agata, E. M., Horn, M. A., Ruan, S., Webb, G. F. & Wares, J. R. Efficacy of infection control interventions in reducing the spread of multidrug-resistant organisms in the hospital setting. PLoS. One 7, e30170 (2012).
Hawser, S. P. et al. Susceptibility of European Escherichia coli clinical isolates from intra-abdominal infections, extended-spectrum β-lactamase occurrence, resistance distribution, and molecular characterization of ertapenem-resistant isolates (SMART 2008-2009). Clin. Microbiol. Infect. 18, 253–259 (2012).
Yamamoto, A. Extended-spectrum β-lactamase (ESBL)-producing Escherichia coli is frequently detected as a pathogen of urinary tract infection in nursing home residents. Nihon Ronen Igakkai Zasshi 48, 530–538 (2011).
Perz, J. F. et al. Changes in antibiotic prescribing for children after a community-wide campaign. JAMA 287, 3103–3109 (2002).
Earnshaw, S. et al. European Antibiotic Awareness Day, 2008–the first Europe-wide public information campaign on prudent antibiotic use: methods and survey of activities in participating countries. Euro. Surveill. 14, 19280 (2009).
Levy, S. B. Antibiotic resistance: an ecological imbalance. Ciba. Found. Symp. 207, 1–9 (1997).
Wenzel, R. P. & Edmond, M. B. Managing antibiotic resistance. N. Engl. J. Med. 343, 1961–1963 (2000).
Towns, M. L., Jarvis, W. R. & Hsueh, P. R. Guidelines on blood cultures. J. Microbiol. Imuunol. Infect. 43, 347–349 (2010).
Abe, T., Tokuda, Y., Ishimatsu, S. & Birrer, R. B. Usefulness of initial blood cultures in patients admitted with pneumonia from anemergency department in Japan. J. Infect. Chemother. 15, 180–186 (2009).
Acknowledgements
We thank Gary Mawyer for English editing.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shigemura, K., Osawa, K., Mukai, A. et al. Infection control team activity and recent antibiograms in the Kobe University Hospital. J Antibiot 66, 511–516 (2013). https://doi.org/10.1038/ja.2013.36
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/ja.2013.36