Abstract
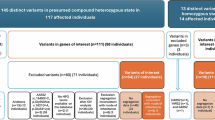
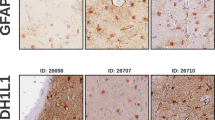
To delineate the phenotype and genotype in Chinese children with type I Alexander disease (AxD) and the parental origin of de novo glial fibrillary acidic protein (GFAP) mutations. Twenty-two children with clinically diagnosed type I AxD were followed up for 1.66–6.62 years. Allele-specific PCR was used for the analysis of parental origin of the allele harboring the de novo mutation. Phenotype of these patients were consistent with type I AxD described in other population, with developmental delay (motor delay in 81.82%, cognitive delay in 63.64%), macrocephaly (100%), seizures (95.45%), paroxysmal deterioration (27.27%) and typical brain magnetic resonance imaging (100%). Progression was slower than reported. At 8.55 years of age (5.29–13.25), all patients who underwent the second follow-up were alive. Eleven heterozygous missense mutations of GFAP were identified in 21 patients, with three novel mutations. Reported hot spot mutations, p.R79, p.R239 and p.R88, were also identified in Chinese patients. Mutations were de novo in all but one case. The mother of a proband was demonstrated to be a presymptomatic patient with type II AxD with a p.R79H mutation. Ninety percent of de novo mutations were on the paternal allele demonstrated by allele-specific PCR. This is the largest follow-up study on Chinese children with AxD. The phenotypes of these patients are consistent with reports in other populations. GFAP mutations were identified in 95.46% of Chinese children with clinically diagnosed type I AxD. Our data suggested a male germ-line transmission.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Li, R., Jonhson, A. B., Salomons, G., Goldman, J. E., Naidu, S., Quinlan, R. & Wu, Y. Glial fibrillary acidic protein mutations in infantile, juvenile, and adult forms of Alexander disease. Ann. Neurol. 57, 310–326 (2005).
Johnson, A. B. & Brenner, M. Alexander disease: a review and the gene. Int. J. Dev. Neurosci. 20, 391–394 (2002).
Prust, M., Wang, J., Morizono, H., Messing, A., Brenner, M., Gordon, E. et al. GFAP mutations, age at onset, and clinical subtypes in Alexander disease. Neurology 77, 1287–1294 (2011).
Johnson, A. B. & Bettica, A. On-grid immunogold labeling of glial intermediate filaments in epoxy-embedded tissue. Am. J. Anat. 185, 335–341 (1989).
Head, M. W., Corbin, E. & Goldman, J. E. Overexpression and abnormal modification of the stress proteins alpha B-crystallin and HSP27 in Alexander disease. Am. J. Pathol. 143, 1743–1753 (1993).
Brenner, M., Johnson, A. B., Boespflug-Tanguy, O., Rodriquez, D., Goldman, J. E. & Messing, A. Mutations in GFAP, encoding glial fibrillary acidic protein, are associated with Alexander disease. Nat. Genet. 27, 117–120 (2001).
Brenner, M., Goldman, J. E., Quinlan, R. A. & Messing, A. Alexander disease: a genetic disorder of astrocytes In: Astrocytes in (Patho) Physiology of the Nervous System (eds Parpura V., Haydon P. G.), pp 591–648 Springer: New York, (2009).
Messing, A., Daniels, C. M. & Hagemann, T. L. Strategies for treatment in Alexander disease. Neurotherapeutics 7, 507–515 (2010).
van der Knaap, M. S., Naidu, S., Breiter, S. N., Blaser, S., Stroink, H., Springer, S. et al. Alexander disease: diagnosis with MR imaging. Am. J. Neuroradiol. 22, 541–552 (2001).
Shi, W., Wang, S. J., Yang, H., Zhu, M. & Wang, L. Study on reliability and validity of the Chinese version of the gross motor function classification system for cerebral palsy. Chin. J. Evld. Based Pediatr. 1, 122–129 (2006).
Yoshida, T. & Nakagawa, M. Clinical aspects and pathology of Alexander disease, and morphological and functional alterationof astrocytes induced by GFAP mutation. Neuropathlogogy doi:10.1111/j.1440-1789 (2011).
Balbi, P., Salvini, S., Fundarò, C., Frazzitta, G., Maestri, R., Mosah, D. et al. The clinical spectrum of late-onset Alexander disease: a systematic literature review. J. Neurol. 257, 1955–1962 (2010).
van der Knaap, M. S., Pronk, J. C. & Scheper, G. C. Vanishingwhite matter disease. Lancet Neurol. 5, 413–423 (2006).
D'Antonio, M., Feltri, M. L. & Wrabetz, L. Myelin under stress. J. Neurosci. Res. 87, 3241–3249 (2009).
Probst, E. N., Hagel, C., Weisz, V., Nagel, S., Wittkugel, O., Zeumer, H. et al. Atypical focal MRI lesions in a case of juvenile Alexander’s disease. Ann. Neurol. 53, 118–120 (2003).
van der Knaap, M. S., Salomons, G. S., Li, R., Franzoni, E., Gutiérrez-Solana, L. G., Smit, L. M. et al. Unusual variants of Alexander’s disease. Ann. Neurol. 57, 327–338 (2005).
Barreau, P., Prust, M. J., Crane, J., Loewenstein, J., Kadom, N. & Vanderver, A. Focal central white matter lesions in Alexander disease. J. Child. Neurol. 26, 1422–1424 (2011).
Schmidt, S., Wattjes, M. P., Gerding, W. M. & van der Knaap, M. Late onset Alexander’s disease presenting as cerebellar ataxia associated with a novel mutation in the GFAP gene. J. Neurol. 258, 938–940 (2011).
Jefferson, R. J., Absoud, M., Jain, R., Livingston, J. H., Van der Knaap, M. S. & Jayawant, S. Alexander disease with perivent ricular calcification: a novel mutation of the GFAP gene. Dev. Med. Child. Neurol. 52, 1160–1163 (2010).
Namekawa, M., Takiyama, Y., Honda, J., Shimazaki, H., Sakoe, K. & Nakano, I. Adult-onset Alexander disease with typical“ tadpole” brainstem atrophy and unusual bilateral basal ganglia involvement: a case report and review of the literature. BMC Neurol. 10, 21 (2010).
Johnson, A. B. & Brenner, M. Alexander’s disease: clinical, pathologic, and genetic features. J. Child. Neurol. 18, 625–632 (2003).
Eng, L. F., Ghirnikar, R. S. & Lee, Y. L. Glial fibrillary acidic protein: GFAP-Thirty-One Years (1969–2000). Neurochem. Res. 25, 1439–1451 (2000).
Sawaishi, Y. Review of Alexander disease: beyond the classical concept of leukodystrophy. Brain Dev. 31, 493–498 (2009).
Wang, L., Colodner, K. J. & Feany, M. B. Protein misfolding and oxidative stress promote glial-mediated neurodegeneration in an Alexander disease model. J. Neurosci. 31, 2868–2877 (2011).
Meisingset, T. W., Risa, Ø., Brenner, M., Messing, A. & Sonnewald, U. Alteration of glial-neuronal metabolic interactions in a mouse model of Alexander disease. Glia 58, 1228–1234 (2010).
Messing, A., Brenner, M., Feany, M. B., Feany, M. B., Nedergaard, M. & Goldman, J. E. Alexander disease. J. Neurosci. 32, 5017–5023 (2012).
Rodriguez, D., Gauthier, F., Bertini, E., Bugiani, M., Brenner, M., N’guyen, S. et al. Infantile Alexander disease: spectrum of GFAP mutations and genotype-phenotype correlation. Am. J. Hum. Genet. 69, 1134–1140 (2001).
Brenner, M., Johnson, A. B., Boespflug-Tanguy, O., Rodriguez, D., Glodman, J. E. & Messing, A. Mutations in GFAP, encoding glial fibrillary acidic protein, are associated with Alexander disease. Nature Genet. 27, 117–120 (2001).
Li, R., Jonhson, A. B., Salomons, G. S., van der Knaap, M. S., Rodriguez, D., Boespflug-Tanguy, O. et al. Propensity for paternal inheritance of de novo mutations in Alexander disease. Hum. Genet. 119, 137–144 (2006).
Girard, M., Couvert, P., Carrié, A., Tardieu, M., Chelly, J., Beldjord, C. et al. Parental origin of de novo MECP2 mutations in Rett syndrome. Eur. J. Hum. Genet. 9, 231–236 (2001).
Heron, S. E., Scheffer, I. E., Iona, X., Zuberi, S. M., Birch, R., McMahon, J. M. et al. De novo SCN1A mutations in Dravet syndrome and related epileptic encephalopathies are largely of paternal origin. J. Med. Genet. 47, 137–141 (2010).
Robertson, K. D. & Wolffe, A. P. DNA methylation in health and disease. Nat. Rev. Genet. 1, 11–19 (2000).
Monk, M. Epigenetic programming of differential gene expression in development and evolution. Dev. Genet. 17, 188–197 (1995).
Taylor, J., Tyekucheva, S., Zody, M., Chiaromonte, F. & Makove, K. D. Strong and weak male mutation bias at different sites in the primate genomes: insights from the human-chimpanzee comparison. Mol. Biol. Evol. 23, 565–573 (2006).
Acknowledgements
The study was supported by the program for new century excellent talents in university from the Chinese Ministry of Education and Natural Science Foundation of China (81171065).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zang, L., Wang, J., Jiang, Y. et al. Follow-up study of 22 Chinese children with Alexander disease and analysis of parental origin of de novo GFAP mutations. J Hum Genet 58, 183–188 (2013). https://doi.org/10.1038/jhg.2012.152
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/jhg.2012.152
Keywords
This article is cited by
-
Symptomatic care of late-onset Alexander disease presenting with area postrema-like syndrome with prednisolone; a case report
BMC Pediatrics (2022)
-
Identification of a novel de novo pathogenic variant in GFAP in an Iranian family with Alexander disease by whole-exome sequencing
European Journal of Medical Research (2022)
-
Does genetic anticipation occur in familial Alexander disease?
neurogenetics (2021)