Abstract
Objective:
Unplanned extubation events (UPEs) in neonates are hazardous to patient safety. Our goal was to reduce UPE rate (#UPEs per 100 ventilator days) by 50% in 12 months at our 25-bed level III inborn unit.
Study Design:
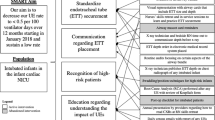
Baseline data were gathered prospectively for 7 months. Three Plan-Do-Study-Act (PDSA) cycles targeting main causes of UPEs were developed over the next 20 months. Causes of UPEs were analyzed using Pareto charts; and a U control chart was created with QI Charts©. Standard rules for detecting special cause variation were applied.
Result:
Mean UPE rate decreased from 16.1 to 4.5 per 100 ventilator days, a 72% decrease, exceeding our goal. Analysis of U-chart demonstrated special cause variation, with eight consecutive points below the mean. Improvement was sustained throughout the study period.
Conclusion:
UPEs in neonates can be reduced with process standardization and frontline staff education, emphasizing vigilant endotracheal tube (ETT) maintenance.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Loughead JL, Brennan RA, DeJulio P, Camposeo V, Wengert J, Cooke D . Reducing accidental extubation in neonoates. Jt Comm J Qual Patient Saf 2008; 34 (3): 164–170 125.
Veldman A, Trautschold T, Weib K, Fischer D, Bauer K . Characteristics and outcomes of unplanned extubation in ventilated preterm and term newborns on a neonatal intensive care unit. Paediatr Anaesth 2006; 16 (9): 968–973.
Carvalho FL, Mezzacappa MA, Calil R, Machado Hda C . Incidence and risk factors of accidental extubation in a neonatal intensive care unit. J Pediatr (Rio J) 2010; 86 (3): 189–195.
Lucas da Silva PS, Reis ME, Aguiar VE, Fonseca MC . Unplanned extubation in the neonatal ICU: A systematic review, critical appraisal, and evidence-based recommendations. Respir Care 2013; 58 (7): 1237–1245.
Lucas da Silva PS, de Carvalho WB . Unplanned extubation in pediatric critically ill patients: A systematic review and best practice recommendations. Pediatr Crit Care Med 2010; 11 (2): 287–294.
Barber JA . Unplanned extubation in the NICU. J Obstet Gynecol Neonatal Nurs 2013; 42: 233–238.
Merkel L, Beers K, Lewis MM, Stauffer J, Mujsce DJ, Kresch MJ . Reducing unplanned extubations in the NICU. Pediatrics 2014; 133 (5): e1367–e1372.
Provost LP, Murray S . The Health Care Data Guide: Learning from Data for Improvement. Jossey-Bass Publishers: San Francisco, CA, USA, 2011; 107–136.
Sharek PJ, Horbar JD, Mason W, Bisarya H, Thurm CW, Suresh G et al. Adverse events in the Neonatal Intensive Care Unit: Development, testing, and findings of a NICU-focused trigger tool to identify harm in North American NICUs. Pediatrics 2006; 118 (4): 1332–1340.
Gardner A, Hughes D, Cook R, Henson R, Osborne S, Gardner G . Best practice in stabilization of oral endotracheal tubes: a systematic review. Aust Crit Care 2005; 18 (4)158 160–165.
Lai M, Inglis GDT, Hose K, Jardine LA, Davies MW . Methods for securing endotracheal tubes in newborn infants. Cochrane Database Syst Rev 2014; 7: CD007805.
Meyers JM, Pinheiro J, Nelson MU . Unplanned extubation in NICU patients: are we speaking the same language? J Perinatol 2015; 35: 676–677.
Acknowledgements
We acknowledge all the nursing staff, neonatal fellows and neonatal nurse practitioners at Hahnemann University Hospital who contributed to the development and implementation of this quality improvement project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Fontánez-Nieves, T., Frost, M., Anday, E. et al. Prevention of unplanned extubations in neonates through process standardization. J Perinatol 36, 469–473 (2016). https://doi.org/10.1038/jp.2015.219
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/jp.2015.219
This article is cited by
-
Use of an airway bundle to reduce unplanned extubations in a neonatal intensive care unit
Journal of Perinatology (2024)
-
Short-term complications and long-term morbidities associated with repeated unplanned extubations
Journal of Perinatology (2021)
-
Enhanced recovery after surgery (ERAS) protocols in neonates should focus on the respiratory tract
Pediatric Surgery International (2019)
-
Counting unplanned extubations: marked variation among neonatologists
Journal of Perinatology (2017)