Abstract
Objective:
Post-mortem examination can provide important information about the cause of death and play a significant role in the bereavement process. Autopsies reveal previous unknown medical problems approximately 20 to 30% of the time. A non-invasive magnetic resonance imaging-based post-mortem examination (PM-MRI) may provide an alternative for families who do not consent to an autopsy.
Study Design:
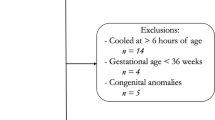
This study was a prospective observational study of recently expired neonates and infants. Subjects underwent a full body MRI scan (brain, chest, abdomen and pelvis) followed by conventional autopsy if the family desired to have one. MRI results were compared with autopsy findings and the ante-mortem clinical diagnosis. A follow-up survey was conducted to investigate family perceptions of the PM-MRI process.
Results:
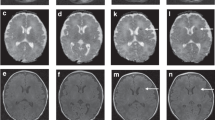
Thirty-one infants underwent full PM-MRI. Of 31 infants, 19 (61%) had complete agreement between the clinician’s impression and PM-MRI. Twenty-four infants also had conventional autopsy, with 14/24 (58%) infants having PM-MRI results consistent with autopsy findings. PM-MRI was superior at detection of free intraperitoneal/intrathoracic air and hepatic iron overload. Whole-body PM-MRI did not have the resolution to detect focal/microscopic injury, vascular remodeling and some forms of brain injury. Of those families who remembered the PM-MRI findings, the majority felt that the information was useful.
Conclusions:
PM-MRI studies may provide an important adjunct to conventional autopsy and a substitute when the latter is not possible for personal or religious reasons. Clinicians should be aware of, and communicate with the family, the resolution limits of the whole-body PM-MRI to detect certain types of injury.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Sailer DN . The clinical utility of the perinatal autopsy. JAMA 1995; 273: 663.
Craft H . Autopsy: high yield in neonatal population. Am J Dis Child 1986; 140: 1260.
Griffiths PD, Paley MNJ, Whitby EH . Post-mortem MRI as an adjunct to fetal or neonatal autopsy. Lancet Lond Engl 2005; 365: 1271–1273.
Combes A, Mokhtari M, Couvelard A, Trouillet J-L, Baudot J, Hénin D et al. Clinical and autopsy diagnoses in the intensive care unit: a prospective study. Arch Intern Med 2004; 164: 389–392.
Cardoso MP, Bourguignon DC, Gomes MM, Saldiva PHN, Pereira CR, Troster EJ . Comparison between clinical diagnoses and autopsy findings in a pediatric intensive care unit in São Paulo, Brazil. Pediatr Crit Care Med 2006; 7: 423–427.
Kabra NS, Udani RH . Correlation between clinical diagnoses at the time of death and autopsy findings in critically sick neonates at a regional neonatal intensive care unit in India. J Trop Pediatr 2001; 47: 295–300.
Brodlie M . Ten years of neonatal autopsies in tertiary referral centre: retrospective study. BMJ 2002; 324: 761–763.
Shojania KG, Burton EC, McDonald KM, Goldman L . Changes in rates of autopsy-detected diagnostic errors over time: a systematic review. JAMA 2003; 289: 2849–2856.
Tsitsikas DA, Brothwell M, Chin Aleong J-A, Lister AT . The attitudes of relatives to autopsy: a misconception. J Clin Pathol 2011; 64: 412–414.
O’Grady G . Death of the teaching autopsy. BMJ 2003; 327: 802–803.
Sherwood SJ, Start RD . Asking relatives for permission for a post mortem examination. Postgrad Med J 1995; 71: 269–272.
Burton JL, Underwood J . Clinical, educational, and epidemiological value of autopsy. Lancet Lond Engl 2007; 369: 1471–1480.
Sanner MA . In perspective of the declining autopsy rate. Attitudes of the public. Arch Pathol Lab Med 1994; 118: 878–883.
Bolliger SA, Thali MJ . Imaging and virtual autopsy: looking back and forward. Philos Trans R Soc B Biol Sci 2015; 370: 20140253.
Brookes JA, Hall-Craggs MA, Sams VR, Lees WR . Non-invasive perinatal necropsy by magnetic resonance imaging. Lancet 1996; 348: 1139–1141.
Woodward PJ, Sohaey R, Harris DP, Jackson GM, Klatt EC, Alexander AL et al. Postmortem fetal MR imaging: comparison with findings at autopsy. Am J Roentgenol 1997; 168: 41–46.
Alderliesten ME, Peringa J, Hulst VPM, Blaauwgeers HLG, Lith JMM . Perinatal mortality: clinical value of postmortem magnetic resonance imaging compared with autopsy in routine obstetric practice. BJOG Int J Obstet Gynaecol 2003; 110: 378–382.
Arthurs OJ, Thayyil S, Owens CM, Olsen OE, Wade A, Addison S et al. Diagnostic accuracy of post mortem MRI for abdominal abnormalities in foetuses and children. Eur J Radiol 2015; 84: 474–481.
Vaneckova M, Seidl Z, Goldova B, Vitkova I, Baxova A, Petrovicky P et al. Post-mortem magnetic resonance imaging and its irreplaceable role in determining CNS malformation (hydranencephaly)—case report. Brain Dev 2010; 32: 417–420.
Vaneckova M, Seidl Z, Goldova B, Vitkova I, Calda P . Benefits of examination by post mortem performed magnetic resonance imaging of foetus: haemorrhage in germinal matrix. Neuro Endocrinol Lett 2010; 31: 40–42.
Bouchireb K, Teychene A-M, Rigal O, de Lonlay P, Valayannopoulos V, Gaudelus J et al. Post-mortem MRI reveals CPT2 deficiency after sudden infant death. Eur J Pediatr 2010; 169: 1561–1563.
Ben-Sasi K, Chitty LS, Franck LS, Thayyil S, Judge-Kronis L, Taylor AM et al. Acceptability of a minimally invasive perinatal/paediatric autopsy: healthcare professionals’ views and implications for practice. Prenat Diagn 2013; 33: 307–312.
Kang X, Cos T, Guizani M, Cannie MM, Segers V, Jani JC . Parental acceptance of minimally invasive fetal and neonatal autopsy compared with conventional autopsy. Prenat Diagn 2014; 34: 1106–1110.
Cannie M, Votino C, Moerman P, Vanheste R, Segers V, Van Berkel K et al. Acceptance, reliability and confidence of diagnosis of fetal and neonatal virtuopsy compared with conventional autopsy: a prospective study. Ultrasound Obstet Gynecol 2012; 39: 659–665.
Thayyil S, Sebire NJ, Chitty LS, Wade A, Chong W, Olsen O et al. Post-mortem MRI versus conventional autopsy in fetuses and children: a prospective validation study. Lancet Lond Engl 2013; 382: 223–233.
Taylor AM, Sebire NJ, Ashworth MT, Schievano S, Scott RJ, Wade A et al. Postmortem cardiovascular magnetic resonance imaging in fetuses and children: a masked comparison study with conventional autopsy. Circulation 2014; 129: 1937–1944.
Norman W, Jawad N, Jones R, Taylor AM, Arthurs OJ . Perinatal and paediatric post-mortem magnetic resonance imaging (PMMR): sequences and technique. Br J Radiol 2016; 89: 20151028.
Acknowledgements
This work was supported by the Washington University Institute of Clinical and Translational Sciences KL2 Training Program (NIH/NCATS KL2 TR000450).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Leadbetter, K., Vesoulis, Z., White, F. et al. The role of post-mortem MRI in the neonatal intensive care unit. J Perinatol 37, 98–103 (2017). https://doi.org/10.1038/jp.2016.156
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/jp.2016.156
This article is cited by
-
The Role and Place of Thanatoradiological Studies in the Pathological Examination of Fetuses and Newborns
Bulletin of Experimental Biology and Medicine (2022)
-
A pragmatic evidence-based approach to post-mortem perinatal imaging
Insights into Imaging (2021)
-
Inter-center variation in autopsy practices among regional neonatal intensive care units (NICUs)
Journal of Perinatology (2021)
-
Peri-mortem evaluation of infants who die without a diagnosis: focus on advances in genomic technology
Journal of Perinatology (2018)