Abstract
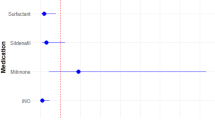
While diagnoses of hypoxemic respiratory failure (HRF) and pulmonary hypertension (PH) in preterm infants may be based on criteria similar to those in term infants, management approaches often differ. In preterm infants, HRF can be classified as ‘early’ or ‘late’ based on an arbitrary threshold of 28 postnatal days. Among preterm infants with late HRF, the pulmonary vascular abnormalities associated with bronchopulmonary dysplasia (BPD) represent a therapeutic challenge for clinicians. Surfactant, inhaled nitric oxide (iNO), sildenafil, prostacyclin and endothelin receptor blockers have been used to manage infants with both early and late HRF. However, evidence is lacking for most therapies currently in use. Chronic oral sildenafil therapy for BPD-associated PH has demonstrated some preliminary efficacy. A favorable response to iNO has been documented in some preterm infants with early PH following premature prolonged rupture of membranes and oligohydramnios. Management is complicated by a lack of clear demarcation between interventions designed to manage respiratory distress syndrome, prevent BPD and treat HRF. Heterogeneity in clinical phenotype, pathobiology and genomic underpinnings of BPD pose challenges for evidence-based management recommendations. Greater insight into the spectrum of disease phenotypes represented by BPD can optimize existing therapies and promote development of new treatments. In addition, better understanding of an individual’s phenotype, genotype and biomarkers may suggest targeted personalized interventions. Initiatives such as the Prematurity and Respiratory Outcomes Program provide a framework to address these challenges using genetic, environmental, physiological and clinical data as well as large repositories of patient samples.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Clark RH, Ursprung RL, Walker MW, Ellsbury DL, Spitzer AR . The changing pattern of inhaled nitric oxide use in the neonatal intensive care unit. J Perinatol 2010; 30: 800–804.
Rawat M, Chandrasekharan PK, Williams A, Gugino S, Koenigsknecht C, Swartz D et al. Oxygen saturation index and severity of hypoxic respiratory failure. Neonatology 2015; 107: 161–166.
Rowe L, Jones JG, Quine D, Bhushan SS, Stenson BJ . A simplified method for deriving shunt and reduced VA/Q in infants. Arch Dis Child Fetal Neonatal Ed 2010; 95: F47–F52.
Skinner JR, Boys RJ, Hunter S, Hey EN . Pulmonary and systemic arterial pressure in hyaline membrane disease. Arch Dis Child 1992; 67: 366–373.
Randala M, Eronen M, Andersson S, Pohjavuori M, Pesonen E . Pulmonary artery pressure in term and preterm neonates. Acta Paediatr 1996; 85: 1344–1347.
Bhat R, Salas AA, Foster C, Carlo WA, Ambalavanan N . Prospective analysis of pulmonary hypertension in extremely low birth weight infants. Pediatrics 2012; 129: e682–e689.
Mourani PM, Sontag MK, Younoszai A, Miller JI, Kinsella JP, Baker CD et al. Early pulmonary vascular disease in preterm infants at risk for bronchopulmonary dysplasia. Am J Respir Crit Care Med 2015; 191: 87–95.
Mirza H, Ziegler J, Ford S, Padbury J, Tucker R, Laptook A . Pulmonary hypertension in preterm infants: prevalence and association with bronchopulmonary dysplasia. J Pediatr 2014; 165: 909–914.
Geary C, Whitsett J . Inhaled nitric oxide for oligohydramnios-induced pulmonary hypoplasia: a report of two cases and review of the literature. J Perinatol 2002; 22: 82–85.
Kilbride HW, Thibeault DW . Strategies of cardiovascular and ventilatory management in preterm infants with prolonged rupture of fetal membranes and oligohydramnios. J Perinatol 2002; 22: 510.
Kilbride HW, Thibeault DW . Neonatal complications of preterm premature rupture of membranes. Pathophysiology and management. Clin Perinatol 2001; 28: 761–785.
Aikio O, Metsola J, Vuolteenaho R, Perhomaa M, Hallman M . Transient defect in nitric oxide generation after rupture of fetal membranes and responsiveness to inhaled nitric oxide in very preterm infants with hypoxic respiratory failure. J Pediatr 2012; 161: 397–403.
Wheeler K, Klingenberg C, McCallion N, Morley CJ, Davis PG . Volume-targeted versus pressure-limited ventilation in the neonate. Cochrane Database Syst Rev 2010; 11: CD003666.
Peng W, Zhu H, Shi H, Liu E . Volume-targeted ventilation is more suitable than pressure-limited ventilation for preterm infants: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed 2014; 99: F158–F165.
Cools F, Offringa M, Askie LM . Elective high frequency oscillatory ventilation versus conventional ventilation for acute pulmonary dysfunction in preterm infants. Cochrane Database Syst Rev 2015; 3, CD000104.
Soll RF . Synthetic surfactant for respiratory distress syndrome in preterm infants. Cochrane Database Syst Rev 2000; 2, CD001149.
Soll RF . Current trials in the treatment of respiratory failure in preterm infants. Neonatology 2009; 95: 368–372.
Pfister RH, Soll RF . Initial respiratory support of preterm infants: the role of CPAP, the INSURE method, and noninvasive ventilation. Clin Perinatol 2012; 39: 459–481.
Polin RA, Carlo WA . Surfactant replacement therapy for preterm and term neonates with respiratory distress. Pediatrics 2014; 133: 156–163.
Rojas-Reyes MX, Morley CJ, Soll R . Prophylactic versus selective use of surfactant in preventing morbidity and mortality in preterm infants. Cochrane Database Syst Rev 2012; 3: CD000510.
Dunn MS, Kaempf J, de Klerk A, de Klerk R, Reilly M, Howard D et al. Randomized trial comparing 3 approaches to the initial respiratory management of preterm neonates. Pediatrics 2011; 128: e1069–e1076.
Carlo WA, Stark AR, Wright LL, Tyson JE, Papile LA, Shankaran S et al. Minimal ventilation to prevent bronchopulmonary dysplasia in extremely-low-birth-weight infants. J Pediatr 2002; 141: 370–374.
Manja V, Lakshminrusimha S, Cook DJ . Oxygen saturation target range for extremely preterm infants: a systematic review and meta-analysis. JAMA Pediatr 2015; 169: 332–340.
Kumar P . Use of inhaled nitric oxide in preterm infants. Pediatrics 2014; 133: 164–170.
Askie LM, Ballard RA, Cutter GR, Dani C, Elbourne D, Field D et al. Inhaled nitric oxide in preterm infants: an individual-patient data meta-analysis of randomized trials. Pediatrics 2011; 128: 729–739.
Gadhia MM, Cutter GR, Abman SH, Kinsella JP . Effects of early inhaled nitric oxide therapy and vitamin A supplementation on the risk for bronchopulmonary dysplasia in premature newborns with respiratory failure. J Pediatr 2014; 164: 744–748.
de Waal K, Kluckow M . Prolonged rupture of membranes and pulmonary hypoplasia in very preterm infants: pathophysiology and guided treatment. J Pediatr 2015; 166: 1113–1120.
Shah DM, Kluckow M . Early functional echocardiogram and inhaled nitric oxide: usefulness in managing neonates born following extreme preterm premature rupture of membranes (PPROM). J Paediatr Child Health 2011; 47: 340–345.
Gournay V, Savagner C, Thiriez G, Kuster A, Roze JC . Pulmonary hypertension after ibuprofen prophylaxis in very preterm infants. Lancet 2002; 359: 1486–1488.
Bellini C, Campone F, Serra G . Pulmonary hypertension following L-lysine ibuprofen therapy in a preterm infant with patent ductus arteriosus. CMAJ 2006; 174: 1843–1844.
Kumar VH, Hutchison AA, Lakshminrusimha S, Morin FC III, Wynn RJ, Ryan RM . Characteristics of pulmonary hypertension in preterm neonates. J Perinatol 2007; 27: 214–219.
Abman SH, Hansmann G, Archer S, Ivy D, Adatia I, Chung WK et al. Pediatric pulmonary hypertension guidelines from the American Heart Association and American Thoracic Society. Circulation 2015; 132: 2037–2099.
James AT, Bee C, Corcoran JD, McNamara PJ, Franklin O, El-Khuffash AF . Treatment of premature infants with pulmonary hypertension and right ventricular dysfunction with milrinone: a case series. J Perinatol 2015; 35: 268–273.
Radicioni M, Bruni A, Camerini P . Combination therapy for life-threatening pulmonary hypertension in a premature infant: first report on bosentan use. Eur J Pediatr 2011; 170: 1075–1078.
Reynolds EW, Conely ET, Vranicar M . Nesiritide for the treatment of pulmonary hypertension and cor pulmonale in an infant. Pediatr Cardiol 2007; 28: 229–233.
Motti A, Tissot C, Rimensberger PC, Prina-Rousso A, Aggoun Y, Berner M et al. Intravenous adenosine for refractory pulmonary hypertension in a low-weight premature newborn: a potential new drug for rescue therapy. Pediatr Crit Care Med 2006; 7: 380–382.
Claure N, Bancalari E . Automation of respiratory support in premature infants. Early Hum Dev 2013; 89 (Suppl 1): S28–S30.
Rochow N, Manan A, Wu WI, Fusch G, Monkman S, Leung J et al. An integrated array of microfluidic oxygenators as a neonatal lung assist device: in vitro characterization and in vivo demonstration. Artif Organs 2014; 38: 856–866.
Schmidt B, Roberts RS, Davis P, Doyle LW, Barrington KJ, Ohlsson A et al. Caffeine therapy for apnea of prematurity. N Engl J Med 2006; 354: 2112–2121.
Tyson JE, Wright LL, Oh W, Kennedy KA, Mele L, Ehrenkranz RA et al. Vitamin A supplementation for extremely-low-birth-weight infants. National Institute of Child Health and Human Development Neonatal Research Network. N Engl J Med 1999; 340: 1962–1968.
Check J, Gotteiner N, Liu X, Su E, Porta N, Steinhorn R et al. Fetal growth restriction and pulmonary hypertension in premature infants with bronchopulmonary dysplasia. J Perinatol 2013; 33: 553–557.
Collaco JM, Romer LH, Stuart BD, Coulson JD, Everett AD, Lawson EE et al. Frontiers in pulmonary hypertension in infants and children with bronchopulmonary dysplasia. Pediatr Pulmonol 2012; 47: 1042–1053.
Mourani PM, Sontag MK, Younoszai A, Ivy DD, Abman SH . Clinical utility of echocardiography for the diagnosis and management of pulmonary vascular disease in young children with chronic lung disease. Pediatrics 2008; 121: 317–325.
del Cerro MJ, Sabate RA, Carton A, Deiros L, Bret M, Cordeiro M et al. Pulmonary hypertension in bronchopulmonary dysplasia: clinical findings, cardiovascular anomalies and outcomes. Pediatr Pulmonol 2014; 49: 49–59.
Trittmann JK, Peterson E, Rogers LK, Chen B, Backes CH, Klebanoff MA et al. Plasma asymmetric dimethylarginine levels are increased in neonates with bronchopulmonary dysplasia-associated pulmonary hypertension. J Pediatr 2015; 166: 230–233.
Kim DH, Kim HS . Serial changes of serum endostatin and angiopoietin-1 levels in preterm infants with severe bronchopulmonary dysplasia and subsequent pulmonary artery hypertension. Neonatology 2014; 106: 55–61.
Cuna A, Kandasamy J, Sims B . B-type natriuretic peptide and mortality in extremely low birth weight infants with pulmonary hypertension: a retrospective cohort analysis. BMC Pediatr 2014; 14: 68.
Mourani PM, Sontag MK, Ivy DD, Abman SH . Effects of long-term sildenafil treatment for pulmonary hypertension in infants with chronic lung disease. J Pediatr 2009; 154: 379–84, 384.
Nyp M, Sandritter T, Poppinga N, Simon C, Truog WE . Sildenafil citrate, bronchopulmonary dysplasia and disordered pulmonary gas exchange: any benefits? J Perinatol 2012; 32: 64–69.
Tan K, Krishnamurthy MB, O'Heney JL, Paul E, Sehgal A . Sildenafil therapy in bronchopulmonary dysplasia-associated pulmonary hypertension: a retrospective study of efficacy and safety. Eur J Pediatr 2015; 174: 1109–1115.
Trottier-Boucher MN, Lapointe A, Malo J, Fournier A, Raboisson MJ, Martin B et al. Sildenafil for the treatment of pulmonary arterial hypertension in infants with bronchopulmonary dysplasia. Pediatr Cardiol 2015; 36: 1255–1260.
Steiner M, Salzer U, Baumgartner S, Waldhoer T, Klebermass-Schrehof K, Wald M et al. Intravenous sildenafil i.v. as rescue treatment for refractory pulmonary hypertension in extremely preterm infants. Klin Padiatr 2014; 226: 211–215.
Stultz JS, Puthoff T, Backes C Jr, Nahata MC . Intermittent intravenous sildenafil for pulmonary hypertension management in neonates and infants. Am J Health Syst Pharm 2013; 70: 407–413.
Yilmaz O, Kahveci H, Zeybek C, Ciftel M, Kilic O . Inhaled iloprost in preterm infants with severe respiratory distress syndrome and pulmonary hypertension. Am J Perinatol 2014; 31: 321–326.
Piastra M, De LD, De Carolis MP, Tempera A, Stival E, Caliandro F et al. Nebulized iloprost and noninvasive respiratory support for impending hypoxaemic respiratory failure in formerly preterm infants: a case series. Pediatr Pulmonol 2012; 47: 757–762.
Eifinger F, Sreeram N, Mehler K, Huenseler C, Kribs A, Roth B . Aerosolized iloprost in the treatment of pulmonary hypertension in extremely preterm infants: a pilot study. Klin Padiatr 2008; 220: 66–69.
Ferdman DJ, Rosenzweig EB, Zuckerman WA, Krishnan U . Subcutaneous treprostinil for pulmonary hypertension in chronic lung disease of infancy. Pediatrics 2014; 134: e274–e278.
Baraldi E, Filippone M . Chronic lung disease after premature birth. N Engl J Med 2007; 357: 1946–1955.
Shennan AT, Dunn MS, Ohlsson A, Lennox K, Hoskins EM . Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics 1988; 82: 527–532.
Jobe AH, Bancalari E . Bronchopulmonary dysplasia. Am J Respir Crit Care Med 2001; 163: 1723–1729.
Walsh MC, Yao Q, Gettner P, Hale E, Collins M, Hensman A et al. Impact of a physiologic definition on bronchopulmonary dysplasia rates. Pediatrics 2004; 114: 1305–1311.
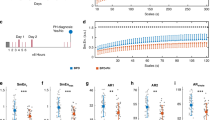
Ambalavanan N, Cotten CM, Page GP, Carlo WA, Murray JC, Bhattacharya S et al. Integrated genomic analyses in bronchopulmonary dysplasia. J Pediatr 2015; 166: 531–537.
Pryhuber GS, Maitre NL, Ballard RA, Cifelli D, Davis SD, Ellenberg JH et al. Prematurity and respiratory outcomes program (PROP): study protocol of a prospective multicenter study of respiratory outcomes of preterm infants in the United States. BMC Pediatr 2015; 15: 37.
Poindexter BB, Feng R, Schmidt B, Aschner JL, Ballard RA, Hamvas A et al. Comparisons and limitations of current definitions of bronchopulmonary dysplasia for the prematurity and respiratory outcomes program. Ann Am Thorac Soc 2015; 12: 1822–1830 (Epub ahead of print).
Acknowledgements
This article is based on discussions at a roundtable meeting supported by a grant from Mallinckrodt Pharmaceuticals, formerly Ikaria. Presentations and discussions were developed solely by the participants, without grantor input. The meeting chair Robin Steinhorn, MD, determined the agenda and attendees. NA and JLA developed the presentations and led the discussions upon which this article is based, provided critical review and revisions to the outline and manuscript drafts, provided final approval of the version to be published and are accountable for the integrity of the content and for addressing questions. We gratefully acknowledge the contributions of the following individuals who participated in discussion that shaped the content of this article: Jason Gien, MD; John Kinsella, MD; G Ganesh Konduri, MD; Satyan Lakshminrusimha, MD; Ola Didrik Saugstad, MD, PhD, FRCPE; and Robin Steinhorn, MD. Writing and editorial assistance was provided by John Kross, Sharon Suntag and Julie Gerke of Quintiles.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
JLA and NA received honoraria for their participation in a roundtable meeting supported by a grant from Mallinckrodt Pharmaceuticals, formerly Ikaria. JLA owns stock in Gilead, and is named on an intellectual property rights patent for the use of intravenous citrulline for neonatal lung diseases. NA has received research support from Pfizer, and has received research support as a mentor from Ikaria. NIH Grants: 1U01HL101456 (JLA); U01 HL122626 and R01 HD067126 (NA).
Rights and permissions
About this article
Cite this article
Ambalavanan, N., Aschner, J. Management of hypoxemic respiratory failure and pulmonary hypertension in preterm infants. J Perinatol 36 (Suppl 2), S20–S27 (2016). https://doi.org/10.1038/jp.2016.45
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/jp.2016.45
This article is cited by
-
Screening for pulmonary hypertension in preterm infants—not ready for prime time
Journal of Perinatology (2018)
-
The gentle art of saying NO: how nitric oxide gets things done in the hypothalamus
Nature Reviews Endocrinology (2017)