Abstract
Objective:
There is limited data characterizing the risk and impact of surgical site infection (SSI) in neonates; this makes it difficult to identify factors that increase neonatal SSI risk and to determine how SSI affects outcomes in this special population.
Study Design:
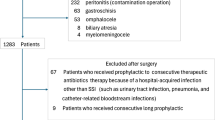
The American College of Surgeons National Surgical Improvement Program Pediatric (NSQIP-P) collected data on children undergoing surgery at children’s hospitals from 2012 to 2014. Neonates undergoing general surgical procedures were characterized with regard to demographic characteristics and comorbidities. Perioperative variables such as wound class, type of surgery and length of operation were also evaluated.
Results:
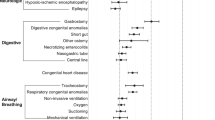
Seven thousand three hundred and seventy-nine neonates were identified in the NSQIP-P participant user file. The overall SSI rate was 2.6%. Only wound class and length of surgery were significantly associated with SSI. Furthermore, SSI was independently associated with longer length of stay, even after adjusting for covariates.
Conclusions:
This is the largest study to date analyzing SSI in neonates. We found that perioperative variables have a more significant impact on SSI than patient factors, suggesting that operation-related characteristics are influencing SSI. Furthermore, neonates with SSI are more likely to have prolonged hospitalizations even after adjusting for patient comorbidities.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Kirkland KB, Briggs JP, Trivette SL, Wilkinson WE, Sexton DJ . The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol 1999; 20: 725–730.
Wilson J . How to reduce the risk of surgical site infection. Nurs Times 2015; 111: 12–16.
Leaper D, Ousey K . Evidence update on prevention of surgical site infection. Curr Opin Infect Dis 2015; 28: 158–163.
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR . Guideline for Prevention of Surgical Site Infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control 1999; 27: 97–132.
Kovarik J, Siegrist CA . Immunity in early life. Immunol Today 1998; 19: 150–152.
Chiswick ML Infection and defences in neonates.Br Med J (Clin Res Ed) 1983; 286: 1377–1378.
Velilla PA, Rugeles MT, Chougnet CA . Defective antigen-presenting cell function in human neonates. Clin Immunol 2006; 121: 251–259.
Miller ME . Phagocytosis in the newborn infant: humoral and cellular factors. J Pediatr 1969; 74: 255–259.
Klein Klouwenberg P, Bont L . Neonatal and infantile immune responses to encapsulated bacteria and conjugate vaccines. Clin Dev Immunol 2008; 2008: 628963.
Bojdo A, Sawicka E, Zak K, Offert B, Szamotulska K . Risk factors of surgical site infection in newborn infants. Med Wieku Rozwoj 2008; 12: 771–777.
Garcia HJ, Rodriguez-Medina X, Franco-Gutierrez M, Miranda-Novales G, Villegas-Silva R . Risk factors for surgical site infections in newborns in a neonatal intensive care unit. Rev Invest Clin 2005; 57: 425–433.
Horwitz JR, Chwals WJ, Doski JJ, Suescun EA, Cheau HW, Lally KP . Pediatric wound infections: a prospective multicenter study. Ann Surg 1998; 227: 553–558.
Lejus C, Dumont R, Gall CL, Guillaud C, Guen CG, Leclair MD et al. A preoperative stay in an intensive care unit is associated with an increased risk of surgical site infection in neonates. J Pediatr Surg 2013; 48: 1503–1508.
Rojo R, Fanjul M, Garcia-Casillas MA, Corona C, Tardaguila AR, Zornoza M et al. Surgical wound infections in newborns: analysis of risk factors. Cir Pediatr 2012; 25: 129–134.
Segal I, Kang C, Albersheim SG, Skarsgard ED, Lavoie PM . Surgical site infections in infants admitted to the neonatal intensive care unit. J Pediatr Surg 2014; 49: 381–384.
Vu LT, Vittinghoff E, Nobuhara KK, Farmer DL, Lee H . Surgical site infections in neonates and infants: is antibiotic prophylaxis needed for longer than 24 h? Pediatr Surg Int 2014; 30: 587–592.
Harrison W, Goodman D . Epidemiologic trends in neonatal intensive care, 2007-2012. JAMA Pediatr 2015; 169: 855–862.
Grover TR, Brozanski BS, Barry J, Zaniletti I, Asselin JM, Durand DJ et al. High surgical burden for infants with severe chronic lung disease (sCLD). J Pediatr Surg 2014; 49: 1202–1205.
Davenport M, Doig CM . Wound infection in pediatric surgery: a study in 1,094 neonates. J Pediatr Surg 1993; 28: 26–30.
ACS NSQIP Pediatric DATA USER GUIDE. American College of Surgeons 2015. Available at https://www.facs.org/quality-programs/pediatric/program-specifics/quality-support-tools/puf (accessed 12 December 2016).
Davis SD, Sobocinski K, Hoffmann RG, Mohr B, Nelson DB . Postoperative wound infections in a children’s hospital. Pediatr Infect Dis 1984; 3: 114–116.
Duque-Estrada EO, Duarte MR, Rodrigues DM, Raphael MD . Wound infections in pediatric surgery: a study of 575 patients in a university hospital. Pediatr Surg Int 2003; 19: 436–438.
Steinberg JP, Braun BI, Hellinger WC, Kusek L, Bozikis MR, Bush AJ et al. Timing of antimicrobial prophylaxis and the risk of surgical site infections: results from the Trial to Reduce Antimicrobial Prophylaxis Errors. Ann Surg 2009; 250: 10–16.
Tsuchida T, Takesue Y, Ichiki K, Uede T, Nakajima K, Ikeuchi H et al. Influence of peri-operative hypothermia on surgical site infection in prolonged gastroenterological surgery. Surg Infect (Larchmt) 2016; 17: 570–576.
Poulin P, Chapman K, McGahan L, Austen L, Schuler T . Preoperative skin antiseptics for preventing surgical site infections: what to do? ORNAC J 2014; 32 (12–15): 24–29.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors. The American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in the ACS NSQIP Pediatric are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Gilje, E., Hossain, M., Vinocur, C. et al. Surgical site infections in neonates are independently associated with longer hospitalizations. J Perinatol 37, 1130–1134 (2017). https://doi.org/10.1038/jp.2017.107
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/jp.2017.107
This article is cited by
-
Early postnatal neonatal surgery is associated with a low risk of surgical site infections
Surgery Today (2025)
-
Factors associated with neonatal surgical site infection after abdominal surgery
Pediatric Surgery International (2022)