Abstract
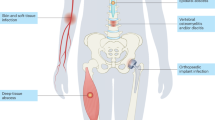
Community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) are the cause of a severe pandemic consisting primarily of skin and soft tissue infections. The underlying pathomechanisms have not been fully understood and we report here a mechanism that plays an important role for the elevated virulence of CA-MRSA. Surprisingly, skin abscess induction in an animal model was correlated with the amount of a major cell wall component of S. aureus, termed wall teichoic acid (WTA). CA-MRSA exhibited increased cell-wall-associated WTA content (WTAhigh) and thus were more active in inducing abscess formation via a WTA-dependent and T-cell-mediated mechanism than S. aureus strains with a WTAlow phenotype. We show here that WTA is directly involved in S. aureus strain-specific virulence and provide insight into the underlying molecular mechanisms that could guide the development of novel anti-infective strategies.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
DeLeo, F. R., Otto, M., Kreiswirth, B. N. & Chambers, H. F. Community-associated meticillin-resistant Staphylococcus aureus. Lancet 375, 1557–1568 (2010).
Stryjewski, M. E. & Chambers, H. F. Skin and soft-tissue infections caused by community-acquired methicillin-resistant Staphylococcus aureus. Clin. Infect. Dis. 46(Suppl. 5), S368–S377 (2008).
Fridkin, S. K. et al. Methicillin-resistant Staphylococcus aureus disease in three communities. N. Engl. J. Med. 352, 1436–1444 (2005).
Purcell, K. & Fergie, J. Epidemic of community-acquired methicillin-resistant Staphylococcus aureus infections: a 14-year study at Driscoll Children's Hospital. Arch. Pediatr. Adolesc. Med. 159, 980–985 (2005).
Hulten, K. G. et al. Three-year surveillance of community onset health care-associated Staphylococcus aureus infections in children. Pediatr. Infect. Dis. J. 25, 349–353 (2006).
Liu, C. et al. A population-based study of the incidence and molecular epidemiology of methicillin-resistant Staphylococcus aureus disease in San Francisco, 2004–2005. Clin. Infect. Dis. 46, 1637–1646 (2008).
Mediavilla, J. R., Chen, L., Mathema, B. & Kreiswirth, B. N. Global epidemiology of community-associated methicillin resistant Staphylococcus aureus (CA-MRSA). Curr. Opin. Microbiol. 15, 588–595 (2012).
Macal, C. M. et al. Modeling the transmission of community-associated methicillin-resistant Staphylococcus aureus: a dynamic agent-based simulation. J. Transl. Med. 12, 124 (2014).
Moran, G. J. et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N. Engl. J. Med. 355, 666–674 (2006).
Baker, P., Cohen, B., Liu, J. & Larson, E . Incidence and risk factors for community-associated methicillin-resistant Staphylococcus aureus in New York City, 2006–2012. Epidemiol. Infect. 144, 1014–1017 (2016).
Como-Sabetti, K. et al. Community-associated methicillin-resistant Staphylococcus aureus: trends in case and isolate characteristics from six years of prospective surveillance. Public Health Rep. 124, 427–435 (2009).
Foster, T. J. Immune evasion by staphylococci. Nat. Rev. Microbiol. 3, 948–958 (2005).
Rooijakkers, S. H., van Kessel, K. P. & van Strijp, J. A. Staphylococcal innate immune evasion. Trends Microbiol. 13, 596–601 (2005).
Otto, M. Basis of virulence in community-associated methicillin-resistant Staphylococcus aureus. Annu. Rev. Microbiol. 64, 143–162 (2010).
Voyich, J. M. et al. Insights into mechanisms used by Staphylococcus aureus to avoid destruction by human neutrophils. J. Immunol. 175, 3907–3919 (2005).
Moran, G. J., Amii, R. N., Abrahamian, F. M. & Talan, D. A. Methicillin-resistant Staphylococcus aureus in community-acquired skin infections. Emerg. Infect. Dis. 11, 928–930 (2005).
King, M. D. et al. Emergence of community-acquired methicillin-resistant Staphylococcus aureus USA 300 clone as the predominant cause of skin and soft-tissue infections. Ann. Intern. Med. 144, 309–317 (2006).
Melles, D. C. et al. Panton–Valentine leukocidin genes in Staphylococcus aureus. Emerg. Infect. Dis. 12, 1174–1175 (2006).
Voyich, J. M. et al. Is Panton–Valentine leukocidin the major virulence determinant in community-associated methicillin-resistant Staphylococcus aureus disease? J. Infect. Dis. 194, 1761–1770 (2006).
Bubeck Wardenburg, J., Bae, T., Otto, M., Deleo, F. R. & Schneewind, O. Poring over pores: α-hemolysin and Panton–Valentine leukocidin in Staphylococcus aureus pneumonia. Nat. Med. 13, 1405–1406 (2007).
Bubeck Wardenburg, J., Palazzolo-Ballance, A. M., Otto, M., Schneewind, O. & DeLeo, F. R. Panton–Valentine leukocidin is not a virulence determinant in murine models of community-associated methicillin-resistant Staphylococcus aureus disease. J. Infect. Dis. 198, 1166–1170 (2008).
Otto, M. Community-associated MRSA: what makes them special? Int. J. Med. Microbiol. 303, 324–330 (2013).
Wang, R. et al. Identification of novel cytolytic peptides as key virulence determinants for community-associated MRSA. Nat. Med. 13, 1510–1514 (2007).
Kobayashi, S. D. et al. Comparative analysis of USA300 virulence determinants in a rabbit model of skin and soft tissue infection. J. Infect. Dis. 204, 937–941 (2011).
Berube, B. J., Sampedro, G. R., Otto, M. & Bubeck Wardenburg, J. The psmα locus regulates production of Staphylococcus aureus alpha-toxin during infection. Infect Immun. 82, 3350–3358 (2014).
Hanberger, H. et al. Increased mortality associated with methicillin-resistant Staphylococcus aureus (MRSA) infection in the intensive care unit: results from the EPIC II study. Int. J. Antimicrob. Agents 38, 331–335 (2011).
Inoshima, I. et al. A Staphylococcus aureus pore-forming toxin subverts the activity of ADAM10 to cause lethal infection in mice. Nat. Med. 17, 1310–1314 (2011).
Cheung, G. Y., Wang, R., Khan, B. A., Sturdevant, D. E. & Otto, M. Role of the accessory gene regulator agr in community-associated methicillin-resistant Staphylococcus aureus pathogenesis. Infect. Immun. 79, 1927–1935 (2011).
Queck, S. Y. et al. RNAIII-independent target gene control by the agr quorum-sensing system: insight into the evolution of virulence regulation in Staphylococcus aureus. Mol. Cell 32, 150–158 (2008).
Li, M. et al. Evolution of virulence in epidemic community-associated methicillin-resistant Staphylococcus aureus. Proc. Natl Acad. Sci. USA 106, 5883–5888 (2009).
Novick, R. P. & Geisinger, E. Quorum sensing in staphylococci. Annu. Rev. Genet. 42, 541–564 (2008).
Novick, R. P. et al. Synthesis of staphylococcal virulence factors is controlled by a regulatory RNA molecule. EMBO J. 12, 3967–3975 (1993).
Bronesky, D. et al. Staphylococcus aureus RNAIII and its regulon link quorum sensing, stress responses, metabolic adaptation, and regulation of virulence gene expression. Annu. Rev. Microbiol. 70, 299–316 (2016).
Miller, L. G. et al. Clinical and epidemiologic characteristics cannot distinguish community-associated methicillin-resistant Staphylococcus aureus infection from methicillin-susceptible S. aureus infection: a prospective investigation. Clin. Infect. Dis. 44, 471–482 (2007).
Diep, B. A. et al. Complete genome sequence of USA300, an epidemic clone of community-acquired meticillin-resistant Staphylococcus aureus. Lancet 367, 731–739 (2006).
Thurlow, L. R. et al. Functional modularity of the arginine catabolic mobile element contributes to the success of USA300 methicillin-resistant Staphylococcus aureus. Cell Host Microbe 13, 100–107 (2013).
Weidenmaier, C. & Peschel, A. Teichoic acids and related cell-wall glycopolymers in Gram-positive physiology and host interactions. Nat. Rev. Microbiol. 6, 276–287 (2008).
Weidenmaier, C. et al. Role of teichoic acids in Staphylococcus aureus nasal colonization, a major risk factor in nosocomial infections. Nat. Med. 10, 243–245 (2004).
Baur, S. et al. A nasal epithelial receptor for Staphylococcus aureus WTA governs adhesion to epithelial cells and modulates nasal colonization. PLoS Pathog. 10, e1004089 (2014).
Weidenmaier, C. et al. DltABCD- and MprF-mediated cell envelope modifications of Staphylococcus aureus confer resistance to platelet microbicidal proteins and contribute to virulence in a rabbit endocarditis model. Infect. Immun. 73, 8033–8038 (2005).
Weidenmaier, C. et al. Lack of wall teichoic acids in Staphylococcus aureus leads to reduced interactions with endothelial cells and to attenuated virulence in a rabbit model of endocarditis. J. Infect. Dis. 191, 1771–1777 (2005).
Lehar, S. M. et al. Novel antibody–antibiotic conjugate eliminates intracellular S. aureus. Nature 527, 323–328 (2015).
Ling, L. L. et al. A new antibiotic kills pathogens without detectable resistance. Nature 517, 455–459 (2015).
Santa Maria, J. P. Jr et al. Compound–gene interaction mapping reveals distinct roles for Staphylococcus aureus teichoic acids. Proc. Natl Acad. Sci. USA 111, 12510–12515 (2014).
Wang, H. et al. Discovery of wall teichoic acid inhibitors as potential anti-MRSA β-lactam combination agents. Chem. Biol. 20, 272–284 (2013).
Pasquina, L. W., Santa Maria, J. P. & Walker, S. Teichoic acid biosynthesis as an antibiotic target. Curr. Opin. Microbiol. 16, 531–537 (2013).
Lee, S. H. et al. TarO-specific inhibitors of wall teichoic acid biosynthesis restore β-lactam efficacy against methicillin-resistant staphylococci. Sci. Transl. Med. 8, 329ra332 (2016).
Mann, P. A. et al. Chemical genetic analysis and functional characterization of staphylococcal wall teichoic acid 2-epimerases reveals unconventional antibiotic drug targets. PLoS Pathog. 12, e1005585 (2016).
Neuhaus, F. C. & Baddiley, J. A continuum of anionic charge: structures and functions of d-alanyl-teichoic acids in Gram-positive bacteria. Microbiol. Mol. Biol. Rev. 67, 686–723 (2003).
Brown, S., Santa Maria, J. P. Jr & Walker, S. Wall teichoic acids of Gram-positive bacteria. Annu. Rev. Microbiol. 67, 313–336 (2013).
Weidenmaier, C., McLoughlin, R. M. & Lee, J. C. The zwitterionic cell wall teichoic acid of Staphylococcus aureus provokes skin abscesses in mice by a novel CD4+ T-cell-dependent mechanism. PLoS One 5, e13227 (2010).
Lazarevic, V. & Karamata, D. The tagGH operon of Bacillus subtilis 168 encodes a two-component ABC transporter involved in the metabolism of two wall teichoic acids. Mol. Microbiol. 16, 345–355 (1995).
Schirner, K., Stone, L. K. & Walker, S. ABC transporters required for export of wall teichoic acids do not discriminate between different main chain polymers. ACS Chem. Biol. 6, 407–412 (2011).
Bunce, C., Wheeler, L., Reed, G., Musser, J. & Barg, N. Murine model of cutaneous infection with Gram-positive cocci. Infect. Immun. 60, 2636–2640 (1992).
Vuong, C., Gotz, F. & Otto, M. Construction and characterization of an agr deletion mutant of Staphylococcus epidermidis. Infect. Immun. 68, 1048–1053 (2000).
Novick, R. P. Autoinduction and signal transduction in the regulation of staphylococcal virulence. Mol. Microbiol. 48, 1429–1449 (2003).
Killikelly, A. et al. Structure-based functional characterization of repressor of toxin (Rot). A central regulator of Staphylococcus aureus virulence. J. Bacteriol. 197, 188–200 (2015).
Rajagopal, M. & Walker, S. Envelope structures of Gram-positive bacteria. Curr. Top. Microbiol. Immunol. http://dx.doi.org.10.1007/82_2015_5021 (2016).
Peschel, A. et al. Inactivation of the dlt operon in Staphylococcus aureus confers sensitivity to defensins, protegrins, and other antimicrobial peptides. J. Biol. Chem. 274, 8405–8410 (1999).
Winstel, V. et al. Wall teichoic acid glycosylation governs Staphylococcus aureus nasal colonization. mBio 6, e00632-15 (2015).
Montgomery, C. P., Boyle-Vavra, S. & Daum, R. S. Importance of the global regulators Agr and SaeRS in the pathogenesis of CA-MRSA USA300 infection. PLoS One 5, e15177 (2010).
Meredith, T. C., Swoboda, J. G. & Walker, S. Late-stage polyribitol phosphate wall teichoic acid biosynthesis in Staphylococcus aureus. J. Bacteriol. 190, 3046–3056 (2008).
Lee, K., Campbell, J., Swoboda, J. G., Cuny, G. D. & Walker, S. Development of improved inhibitors of wall teichoic acid biosynthesis with potent activity against Staphylococcus aureus. Bioorg. Med. Chem. Lett. 20, 1767–1770 (2010).
Swoboda, J. G. et al. Discovery of a small molecule that blocks wall teichoic acid biosynthesis in Staphylococcus aureus. ACS Chem. Biol. 4, 875–883 (2009).
Geisinger, E., Adhikari, R. P., Jin, R., Ross, H. F. & Novick, R. P. Inhibition of rot translation by RNAIII, a key feature of agr function. Mol. Microbiol. 61, 1038–1048 (2006).
Boisset, S. et al. Staphylococcus aureus RNAIII coordinately represses the synthesis of virulence factors and the transcription regulator Rot by an antisense mechanism. Genes Dev. 21, 1353–1366 (2007).
Zhu, Y. et al. Structure of Rot, a global regulator of virulence genes in Staphylococcus aureus. Acta Crystallogr. D 70, 2467–2476 (2014).
Kolata, J. et al. The fall of a dogma? Unexpected high T cell memory response to S. aureus in humans. J. Infect. Dis. 212, 830–838 (2015).
Cho, J. S. et al. IL-17 is essential for host defense against cutaneous Staphylococcus aureus infection in mice. J. Clin. Invest. 120, 1762–1773 (2010).
Malachowa, N., Kobayashi, S. D., Sturdevant, D. E., Scott, D. P. & DeLeo, F. R. Insights into the Staphylococcus aureus–host interface: global changes in host and pathogen gene expression in a rabbit skin infection model. PLoS One 10, e0117713 (2015).
Montgomery, C. P. et al. Protective immunity against recurrent Staphylococcus aureus skin infection requires antibody and interleukin-17A. Infect. Immun. 82, 2125–2134 (2014).
Gibson, D. G. et al. Enzymatic assembly of DNA molecules up to several hundred kilobases. Nat. Methods 6, 343–345 (2009).
Bertsche, U. et al. Increased cell wall teichoic acid production and d-alanylation are common phenotypes among daptomycin-resistant methicillin-resistant Staphylococcus aureus (MRSA) clinical isolates. PLoS One 8, e67398 (2013).
Smith, R. L. & Gilkerson, E. Quantitation of glycosaminoglycan hexosamine using 3-methyl-2-benzothiazolone hydrazone hydrochloride. Anal. Biochem. 98, 478–480 (1979).
Portoles, M., Kiser, K. B., Bhasin, N., Chan, K. H. & Lee, J. C. Staphylococcus aureus Cap5O has UDP-ManNAc dehydrogenase activity and is essential for capsule expression. Infect. Immun. 69, 917–923 (2001).
Mullane, K. M., Kraemer, R. & Smith, B. Myeloperoxidase activity as a quantitative assessment of neutrophil infiltration into ischemic myocardium. J. Pharmacol. Methods 14, 157–167 (1985).
van der Veen, B. S., de Winther, M. P. & Heeringa, P. Myeloperoxidase: molecular mechanisms of action and their relevance to human health and disease. Antioxid. Redox Signal. 11, 2899–2937 (2009).
Acknowledgements
The authors thank I. Autenrieth and A. Peschel for discussions and critical reading of the manuscript. This research was supported by grants from the German Research Foundation (SFB) to C.We. (SFB766 and TR34), C.Wo. (SFB766 and TR34) and B.M.B. (TR34). The funders had no role in the design of the experiments, in the collection, analysis and interpretation of the data, in writing the manuscript, or in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
S.W., C.Wo., J.K., B.M.B., J.S. and C.We. planned the experiments. S.W., J.S., N.W., D.Ke., L.K., J.B., T.G., V.W. and C.We. performed the experiments. C.Wo., J.K., B.M.B., V.W. and D.Kr. supplied materials and strains. S.W., J.S. and C.We. wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Information
Supplementary Table 1, Supplementary Figures 1–17, Supplementary References. (PDF 2207 kb)
Rights and permissions
About this article
Cite this article
Wanner, S., Schade, J., Keinhörster, D. et al. Wall teichoic acids mediate increased virulence in Staphylococcus aureus. Nat Microbiol 2, 16257 (2017). https://doi.org/10.1038/nmicrobiol.2016.257
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/nmicrobiol.2016.257
This article is cited by
-
Trans-kingdom conservation of mechanism between bacterial actifensin and eukaryotic defensins
npj Antimicrobials and Resistance (2025)
-
Design, synthesis and optimization of TarO inhibitors as multifunctional antibiotics against Methicillin-resistant Staphylococcus aureus
npj Antimicrobials and Resistance (2025)
-
Modulation of MRSA virulence gene expression by the wall teichoic acid enzyme TarO
Nature Communications (2023)
-
The effects of daptomycin on cell wall biosynthesis in Enterococcal faecalis
Scientific Reports (2023)
-
A type VII-secreted lipase toxin with reverse domain arrangement
Nature Communications (2023)