Abstract
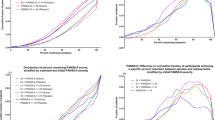
Our objective was to prospectively assess whether early (ie, 2 weeks) response to an antipsychotic predicts later (12-week) response and whether ‘switching’ early non-responders to another antipsychotic is a better strategy than ‘staying’. This randomized, double-blind, flexible-dosed, 12-week study enrolled 628 patients diagnosed with schizophrenia or schizoaffective disorder. All initiated treatment with risperidone. Early response was defined as ⩾20% improvement on the Positive and Negative Syndrome Scale (PANSS) total score following 2 weeks of treatment. Early responders (ERs) continued on risperidone, whereas early non-responders (ENRs) were randomized (1 : 1) to continue on risperidone 2–6 mg/day or switch to olanzapine 10–20 mg/day for 10 additional weeks. Compared with ENRs, risperidone ERs showed significantly greater reduction in PANSS total score (end point; p<001). Early response/non-response was highly predictive of subsequent clinical outcomes. Switching risperidone ENRs to olanzapine at week 2 resulted in a small but significantly greater reduction in PANSS total score (end point; p=0.020) and in depressive symptoms (end point; p=0.004); the reduction in PANSS was greater among those who were still moderately ill at 2 weeks. Switching risperidone ENRs to olanzapine also resulted in significantly greater increases in triglycerides, a significantly greater decrease in prolactin, and significantly less treatment-emergent dyskinesia. This is the first study to prospectively show that early response/non-response to an antipsychotic (risperidone) is a reliable clinical marker of subsequent clinical outcomes and that a ‘switching’ strategy based on this information may lead to greater clinical improvement than staying on a drug for a longer period in some patients.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Agid O, Kapur S, Arenovich T, Zipursky RB (2003). Delayed-onset hypothesis of antipsychotic action: a hypothesis tested and rejected. Arch Gen Psychiatry 60: 1228–1235.
Alvarez E, Ciudad A, Olivares JM, Bousoño M, Gómez JC (2006). A randomized, 1-year follow-up study of olanzapine and risperidone in the treatment of negative symptoms in outpatients with schizophrenia. J Clin Psychopharmacol 26: 238–249.
Ascher-Svanum H, Nyhuis AW, Faries DE, Kinon BJ, Baker RW, Shekhar A (2008). Clinical, functional, and economic ramifications of early nonresponse to antipsychotics in the naturalistic treatment of schizophrenia. Schizophr Bull 34: 1163–1171.
Barnes TR (1989). A rating scale for drug-induced akathisia. Br J Psychiatry 154: 672–676.
Canive JM, Miller GA, Irwin JG, Moses SN, Thoma RJ, Edgar JC et al (2006). Efficacy of olanzapine and risperidone in schizophrenia: a randomized double-blind crossover design. Psychopharmacol Bull 39: 105–116.
Conley RR, Mahmoud R (2001). A randomized double-blind study of risperidone and olanzapine in the treatment of schizophrenia or schizoaffective disorder. Am J Psychiatry 158: 765–774.
Correll CU, Malhotra AK, Kaushik S, McMeniman M, Kane JM (2003). Early prediction of antipsychotic response in schizophrenia. Am J Psychiatry 160: 2063–2065.
Davis JM, Chen N, Glick ID (2003). A meta-analysis of the efficacy of second-generation antipsychotics. Arch Gen Psychiatry 60: 553–564.
Dossenbach M, Erol A, el Mahfoud Kessaci M, Shaheen MO, Sunbol MM, Boland J et al (2004). Effectiveness of antipsychotic treatments for schizophrenia: interim 6-month analysis from a prospective observational study (IC-SOHO) comparing olanzapine, quetiapine, risperidone, and haloperidol. J Clin Psychiatry 65: 312–321.
Essock SM, Covell NH, Davis SM, Stroup TS, Rosenheck RA, Lieberman JA (2006). Effectiveness of switching antipsychotic medications. Am J Psychiatry 163: 2090–2095.
Falkai P (2008). Limitations of current therapies: why do patients switch therapies? Eur Neuropsychopharmacol 18: S135–S139.
Faries DE, Ascher-Svanum H, Nyhuis AW, Kinon BJ (2008). Switching from risperidone to olanzapine in a one-year, randomized, open-label effectiveness study of schizophrenia. Curr Med Res Opin 24: 1399–1405.
Fleischhacker WW, McQuade RD, Marcus RN, Archibald D, Swanink R, Carson WH (2009). A double-blind, randomized comparative study of aripiprazole and olanzapine in patients with schizophrenia. Biol Psychiatry 65: 510–517.
Ganguli R, Brar JS, Mahmoud R, Berry SA, Pandina GJ (2008). Assessment of strategies for switching patients from olanzapine to risperidone: a randomized, open-label, rater-blinded study. BMC Med 6: 17.
Guy W (1976). ECDEU Assessment Manual for Psychopharmacology Revised (Publication ADM 76-338) US Departmnet of Health, Education, and Welfare: Rockville, MD. pp 218–222.
Hardy TA, Marquez E, Kryzhanovskaya L, Taylor CC, Cavazzoni P (2006). Cross-sectional comparison of fasting lipids in normoglycemic patients with schizophrenia during chronic treatment with olanzapine, risperidone, or typical antipsychotics. J Clin Psychopharmacol 26: 405–408.
Haro JM, Suarez D, Novick D, Brown J, Usall J, Naber D et al (2007). Three-year antipsychotic effectiveness in the outpatient care of schizophrenia: observational versus randomized studies results. Eur Neuropsychopharmacol 17: 235–244.
Kay SR, Fiszbein A, Opler LA (1987). The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 13: 261–276.
Kelly DL, Conley RR, Love RC, Morrison JA, McMahon RP (2008). Metabolic risk with second-generation antipsychotic treatment: a double-blind randomized 8-week trial of risperidone and olanzapine. Ann Clin Psychiatry 20: 71–78.
Kinon BJ, Ahl J, Liu-Seifert H, Maguire GA (2006). Improvement in hyperprolactinemia and reproductive comorbidities in patients with schizophrenia switched from conventional antipsychotics or risperidone to olanzapine. Psychoneuroendocrinology 31: 577–588.
Kinon BJ, Chen L, Ascher-Svanum H, Stauffer VL, Kollack-Walker S, Sniadecki JL et al (2008). Predicting response to atypical antipsychotics based on early response in the treatment of schizophrenia. Schizophr Res 102: 230–240.
Kinon BJ, Kane JM, Johns C, Perovich R, Ismi M, Koreen A et al (1993). Treatment of neuroleptic-resistant schizophrenic relapse. Psychopharmacol Bull 29: 309–314.
Konarzewska B, Wolczynski S, Szulc A, Galinska B, Poplawska R, Waszkiewicz N (2009). Effect of risperidone and olanzapine on reproductive hormones, psychopathology and sexual functioning in male patients with schizophrenia. Psychoneuroendocrinology 34: 129–139.
Leucht S, Busch R, Hamann J, Kissling W, Kane JM (2005a). Early-onset hypothesis of antipsychotic drug action: a hypothesis tested, confirmed and extended. Biol Psychiatry 57: 1543–1549.
Leucht S, Busch R, Kissling W, Kane JM (2007). Early prediction of antipsychotic nonresponse among patients with schizophrenia. J Clin Psychiatry 68: 352–360.
Leucht S, Kane JM, Kissling W, Hamann J, Etschel E, Engel RR (2005b). What does the PANSS mean? Schizophr Res 79: 231–238.
Leucht S, Shamsi SA, Busch R, Kissling W, Kane JM (2008). Predicting antipsychotic drug response. Replication and extension to six weeks in an international olanzapine study. Schizophr Res 101: 312–319.
Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO et al (2005). Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 353: 1209–1223.
Meyer JM, Davis VG, McEvoy JP, Goff DC, Nasrallah HA, Davis SM et al (2008). Impact of antipsychotic treatment on nonfasting triglycerides in the CATIE Schizophrenia Trial phase 1. Schizophr Res 103: 104–109.
Montgomery SA, Asberg M (1979). A new depression scale designed to be sensitive to change. Br J Psychiatry 134: 382–389.
Overall JE, Gorham DR (1962). The brief psychiatric rating scale. Psychol Rep 10: 799–812.
Rosenheck RA, Davis S, Covell N, Essock S, Swartz M, Stroup S et al (2009). Does switching to a new antipsychotic improve outcomes? Data from the CATIE Trial. Schizophr Res 107: 22–29.
Simpson GM, Angus JW (1970). A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl 212: 11–19.
Simpson GM, O'Gorman CJ, Loebel A, Yang R (2008). Long-term improvement in efficacy and safety after switching to ziprasidone in stable outpatients with schizophrenia. CNS Spectr 13: 898–905.
Takahashi H, Kamata M, Yoshida K, Ishigooka J, Higuchi H (2006a). Switching to olanzapine after unsuccessful treatment with risperidone during the first episode of schizophrenia: an open-label trial. J Clin Psychiatry 67: 1577–1582.
Takahashi H, Yoshida K, Ishigooka J, Higuchi H (2006b). Switching to risperidone after unsuccessful treatment of olanzapine in the first-episode schizophrenia: an open trial. Prog Neuropsychopharmacol Biol Psychiatry 30: 1067–1072.
Tran PV, Hamilton SH, Kuntz AJ, Potvin JH, Andersen SW, Beasley Jr C et al (1997). Double-blind comparison of olanzapine versus risperidone in the treatment of schizophrenia and other psychotic disorders. J Clin Psychopharmacol 17: 407–418.
Wang X, Savage R, Borisov A, Rosenberg J, Woolwine B, Tucker M et al (2006). Efficacy of risperidone versus olanzapine in patients with schizophrenia previously on chronic conventional antipsychotic therapy: a switch study. J Psychiatr Res 40: 669–676.
Acknowledgements
Appreciation is expressed to Heather Fox, Medical Information Specialist with Lilly USA, LLC, for administrative oversight of the editing for this article. We acknowledge Teri Tucker and Caron Modeas for editorial contributions. Ms Tucker and Modeas are medical editors employed full-time by i3 Statprobe, a division of Ingenix, which is a subsidiary of United Health Group. Eli Lilly contracted the editing and formatting of this article with i3 Statprobe.
Author information
Authors and Affiliations
Corresponding author
Additional information
Previous Presentation: These data debuted at the annual American Psychiatric Association (APA) congress in Washington, DC, May 3–8, 2008.
Clinical Trials Registration: ClinicalTrials.gov identifier: NCT00337662; http://www.clinicaltrials.gov/
DISCLOSURE
Drs Kinon, Chen, Ascher-Svanum, Stauffer, and Kollack-Walker and Wei Zhou are all employees of Eli Lilly and Company. Dr John Kane serves as a Consultant and/or Advisory Board member for Bristol Meyer Squibb; Otsuka America Pharmaceutical Inc.; Eli Lilly and Company; Janssen; Pfizer; Wyeth; Vanda Pharmaceuticals Inc.; GlaxoSmithKline; Lundbeck; Johnson & Johnson; PGxHealth; and Proteus; is a shareholder of MedAvante; and serves on Speakers Bureaus for Bristol Meyer Squibb, Janssen, AstraZeneca, and Eli Lilly and Company. Dr Shitij Kapur has had affiliations with the following commercial organizations over the last 5 years: AstraZeneca; Bristol Meyers Squibb; Eli Lilly and Company; EMD Pharmaceuticals Inc.; Darmstadt; GlaxoSmithKline; Janssen; Neuromolecular Pharmaceuticals; Otsuka America Pharmaceutical Inc.; Organon Pharmaceuticals USA; Pfizer; Sanofi-Synthelabo; Servier; and Solvay Wyeth. Funding of this study was provided by Eli Lilly and Company.
Rights and permissions
About this article
Cite this article
Kinon, B., Chen, L., Ascher-Svanum, H. et al. Early Response to Antipsychotic Drug Therapy as a Clinical Marker of Subsequent Response in the Treatment of Schizophrenia. Neuropsychopharmacol 35, 581–590 (2010). https://doi.org/10.1038/npp.2009.164
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/npp.2009.164
Keywords
This article is cited by
-
Early Non-Response to Antipsychotic Treatment in Schizophrenia: A Systematic Review and Meta-Analysis of Evidence-Based Management Options
CNS Drugs (2023)
-
Antipsychotic-placebo separation on the PANSS-6 subscale as compared to the PANSS-30: a pooled participant-level analysis
npj Schizophrenia (2021)
-
A dopaminergic mechanism of antipsychotic drug efficacy, failure, and failure reversal: the role of the dopamine transporter
Molecular Psychiatry (2020)
-
Switching strategies for antipsychotic monotherapy in schizophrenia: a multi-center cohort study of aripiprazole
Psychopharmacology (2020)
-
Determinants of treatment response in first-episode psychosis: an 18F-DOPA PET study
Molecular Psychiatry (2019)