Abstract
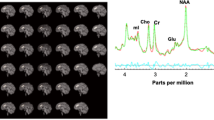
While bupropion HCl and practical group counseling (PGC) are commonly used treatments for tobacco dependence, the effects of these treatments on brain function are not well established. For this study, 54 tobacco-dependent cigarette smokers underwent resting 18F-fluorodeoxyglucose–positron emission tomography (FDG–PET) scanning before and after 8 weeks of treatment with bupropion HCl, PGC, or pill placebo. Using Statistical Parametric Mapping (SPM 2), changes in cerebral glucose metabolism from before to after treatment were compared between treatment groups and correlations were determined between amount of daily cigarette usage and cerebral glucose metabolism. Compared with placebo, the two active treatments (bupropion HCl and PGC) had reductions in glucose metabolism in the posterior cingulate gyrus. Further analysis suggested that PGC had a greater effect than bupropion HCl on glucose metabolism in this region. We also found positive correlations between daily cigarette use and glucose metabolism in the left occipital gyrus and parietal–temporal junction. There were no significant negative correlations between daily cigarette use and glucose metabolism. Our findings suggest that bupropion HCl and PGC reduce neural activity much as the performance of a goal-oriented task does in the default mode network of the brain, including the posterior cingulate gyrus. Thus, this study supports the theory that active treatments for tobacco dependence move the brain into a more goal-oriented state.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Argyelan M, Szabo Z, Kanyo B, Tanacs A, Kovacs Z, Janka Z et al (2005). Dopamine transporter availability in medication free and in bupropion treated depression: a 99mTc-TRODAT-1 SPECT study. J Affect Disord 89: 115–123.
Balfour DJ (2001). The pharmacology underlying pharmacotherapy for tobacco dependence: a focus on bupropion. Int J Clin Pract 55: 53–57.
Bates T, Mangan G, Stough C, Corballis P (1995). Smoking, processing speed and attention in a choice reaction time task. Psychopharmacology (Berlin) 120: 209–212.
Brody AL (2006). Functional brain imaging of tobacco use and dependence. J Psychiatr Res 40: 404–418.
Brody AL, Mandelkern MA, Lee G, Smith E, Sadeghi M, Saxena S et al (2004). Attenuation of cue-induced cigarette craving and anterior cingulate cortex activation in bupropion-treated smokers: a preliminary study. Psychiatry Res 130: 269–281.
Brody AL, Saxena S, Stoessel P, Gillies LA, Fairbanks LA, Alborzian S et al (2001). Regional brain metabolic changes in patients with major depression treated with either paroxetine or interpersonal therapy: preliminary findings. Arch Gen Psychiatry 58: 631–640.
Carmody TP (1990). Preventing relapse in the treatment of nicotine addiction: current issues and future directions. J Psychoactive Drugs 22: 211–238.
CDC (2004). 2004 Surgeon General's Report—the health consequences of smoking.
CDC (2007). Cigarette smoking among adults—United States, 2006 In MMWR pp 1157–1161.
DeGrado TR, Turkington TG, Williams JJ, Stearns CW, Hoffman JM, Coleman RE (1994). Performance characteristics of a whole-body PET scanner. J Nucl Med 35: 1398–1406.
Dhir A, Kulkarni SK (2007). Involvement of nitric oxide (NO) signaling pathway in the antidepressant action of bupropion, a dopamine reuptake inhibitor. Eur J Pharmacol 568: 177–185.
Domino EF, Minoshima S, Guthrie S, Ohl L, Ni L, Koeppe RA et al (2000a). Nicotine effects on regional cerebral blood flow in awake, resting tobacco smokers. Synapse 38: 313–321.
Domino EF, Minoshima S, Guthrie SK, Ohl L, Ni L, Koeppe RA et al (2000b). Effects of nicotine on regional cerebral glucose metabolism in awake resting tobacco smokers. Neuroscience 101: 277–282.
Dooley RT, Halford WK (1992). A comparison of relapse prevention with nicotine gum or nicotine fading in modification of smoking. Aust Psychol 27: 186–191.
Durcan MJ, Deener G, White J, Johnston JA, Gonzales D, Niaura R et al (2002). The effect of bupropion sustained-release on cigarette craving after smoking cessation. Clin Ther 24: 540–551.
Fagerstrom KO (1978). Measuring degree of physical dependence to tobacco smoking with reference to individualization of treatment. Addict Behav 3: 235–241.
Fiore MC, Bailey WC, Cohen SJ, Dorfman SF, Goldstein MG, Gritz ER et al (2000). Treating Tobacco Use and Dependence. Clinical Practice Guideline. U.S. Department of Health and Human Services. Public Health Service: Rockville, MD.
First MB, Spitzer RL, Gibbon M, Williams JBW (1995). Structured Clinical Interview for DSM-IV Axis I Disorders—Patient Edition (SCID-I/P, version 2.0). Biometrics Research Department, New York State Psychiatric Institute: New York.
Fransson P, Marrelec G (2008). The precuneus/posterior cingulate cortex plays a pivotal role in the default mode network: evidence from a partial correlation network analysis. Neuroimage 42: 1178–1184.
Gusnard DA, Raichle ME (2001). Searching for a baseline: functional imaging and the resting human brain. Nat Rev Neurosci 2: 685–694.
Hamilton M (1967). Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol 6: 278–296.
Hamilton M (1969). Diagnosis and rating of anxiety. Br J Psychiatry 3: 76–79.
Hays JT, Hurt RD, Rigotti NA, Niaura R, Gonzales D, Durcan MJ et al (2001). Sustained-release bupropion for pharmacologic relapse prevention after smoking cessation. a randomized, controlled trial. Ann Intern Med 135: 423–433.
Hill P, Haley NJ, Wynder EL (1983). Cigarette smoking: carboxyhemoglobin, plasma nicotine, cotinine and thiocyanate vs self-reported smoking data and cardiovascular disease. J Chronic Dis 36: 439–449.
Holm KJ, Spencer CM (2000). Bupropion: a review of its use in the management of smoking cessation. Drugs 59: 1007–1024.
Horst WD, Preskorn SH (1998). Mechanisms of action and clinical characteristics of three atypical antidepressants: venlafaxine, nefazodone, bupropion. J Affect Disord 51: 237–254.
Hughes JR, Stead LF, Lancaster T (2007). Antidepressants for smoking cessation. Cochrane Database Syst Rev 1: CD000031.
Jacobs Jr DR, Adachi H, Mulder I, Kromhout D, Menotti A, Nissinen A et al (1999). Cigarette smoking and mortality risk: twenty-five-year follow-up of the Seven Countries Study. Arch Intern Med 159: 733–740.
Jarvik ME, Madsen DC, Olmstead RE, Iwamoto-Schaap PN, Elins JL, Benowitz NL (2000). Nicotine blood levels and subjective craving for cigarettes. Pharmacol Biochem Behav 66: 553–558.
Jorenby DE, Leischow SJ, Nides MA, Rennard SI, Johnston JA, Hughes AR et al (1999). A controlled trial of sustained-release bupropion, a nicotine patch, or both for smoking cessation. N Engl J Med 340: 685–691.
Karnath B (2002). Smoking cessation. Am J Med 112: 399–405.
Kennedy SH, Konarski JZ, Segal ZV, Lau MA, Bieling PJ, McIntyre RS et al (2007). Differences in brain glucose metabolism between responders to CBT and venlafaxine in a 16-week randomized controlled trial. Am J Psychiatry 164: 778–788.
Lancaster T, Stead LF (2000). Individual behavioural counselling for smoking cessation. Cochrane Database Syst Rev 2: CD001292.
Leshner AI, Koob GF (1999). Drugs of abuse and the brain. Proc Assoc Am Physicians 111: 99–108.
London ED, Connolly RJ, Szikszay M, Wamsley JK, Dam M (1988a). Effects of nicotine on local cerebral glucose utilization in the rat. J Neurosci 8: 3920–3928.
London ED, Dam M, Fanelli RJ (1988b). Nicotine enhances cerebral glucose utilization in central components of the rat visual system. Brain Res Bull 20: 381–385.
Mai JK (2008). Atlas of the Human Brain: 3rd Edition, 3rd edn. Academic Press: New York, NY.
Martin SD, Martin E, Rai SS, Richardson MA, Royall R (2001). Brain blood flow changes in depressed patients treated with interpersonal psychotherapy or venlafaxine hydrochloride: preliminary findings. Arch Gen Psychiatry 58: 641–648.
Meyer JH, Goulding VS, Wilson AA, Hussey D, Christensen BK, Houle S (2002). Bupropion occupancy of the dopamine transporter is low during clinical treatment. Psychopharmacology (Berlin) 163: 102–105.
Nofzinger EA, Berman S, Fasiczka A, Miewald JM, Meltzer CC, Price JC et al (2001). Effects of bupropion SR on anterior paralimbic function during waking and REM sleep in depression: preliminary findings using. Psychiatry Res 106: 95–111.
Paterson NE, Balfour DJ, Markou A (2007). Chronic bupropion attenuated the anhedonic component of nicotine withdrawal in rats via inhibition of dopamine reuptake in the nucleus accumbens shell. Eur J Neurosci 25: 3099–3108.
Raichle ME, MacLeod AM, Snyder AZ, Powers WJ, Gusnard DA, Shulman GL (2001). A default mode of brain function. Proc Natl Acad Sci USA 98: 676–682.
Reus VI, Smith BJ (2008). Multimodal techniques for smoking cessation: a review of their efficacy and utilisation and clinical practice guidelines. Int J Clin Pract 62: 1753–1768.
Robertson B, Wang L, Diaz MT, Aiello M, Gersing K, Beyer J et al (2007). Effect of bupropion extended release on negative emotion processing in major depressive disorder: a pilot functional magnetic resonance imaging study. J Clin Psychiatry 68: 261–267.
Rose JE, Behm FM, Westman EC, Mathew RJ, London ED, Hawk TC et al (2003). PET studies of the influences of nicotine on neural systems in cigarette smokers. Am J Psychiatry 160: 323–333.
Russell MA, Feyerabend C, Cole PV (1976). Plasma nicotine levels after cigarette smoking and chewing nicotine gum. Br Med J 1: 1043–1046.
Slemmer JE, Martin BR, Damaj MI (2000). Bupropion is a nicotinic antagonist. J Pharmacol Exp Ther 295: 321–327.
Stahl SM, Pradko JF, Haight BR, Modell JG, Rockett CB, Learned-Coughlin S (2004). A review of the neuropharmacology of bupropion, a dual norepinephrine and dopamine reuptake inhibitor. Prim Care Companion J Clin Psychiatry 6: 159–166.
Stapleton JM, Gilson SF, Wong DF, Villemagne VL, Dannals RF, Grayson RF et al (2003). Intravenous nicotine reduces cerebral glucose metabolism: a preliminary study. Neuropsychopharmacology 28: 765–772.
Stead LF, Lancaster T (2005). Group behaviour therapy programmes for smoking cessation. Cochrane Database Syst Rev 2: CD001007.
Stein EA, Pankiewicz J, Harsch HH, Cho JK, Fuller SA, Hoffmann RG et al (1998). Nicotine-induced limbic cortical activation in the human brain: a functional MRI study. Am J Psychiatry 155: 1009–1015.
Tapper AR, McKinney SL, Nashmi R, Schwarz J, Deshpande P, Labarca C et al (2004). Nicotine activation of alpha4* receptors: sufficient for reward, tolerance, and sensitization. Science 306: 1029–1032.
Thiel CM, Fink GR (2007). Visual and auditory alertness: modality-specific and supramodal neural mechanisms and their modulation by nicotine. J Neurophysiol 97: 2758–2768.
Tonnesen P, Mikkelsen K, Bremann L (2008). Smoking cessation with smokeless tobacco and group therapy: an open, randomized, controlled trial. Nicotine Tob Res 10: 1365–1372.
Acknowledgements
Supported by the National Institute on Drug Abuse (ALB (R01 DA20872)), the Veterans Administration (ALB (Merit Review Type I Award)), the Tobacco-Related Disease Research Program (ALB (16RT-0098)), the Office of National Drug Control Policy (EDL (DABT 63-00-C-1003)), and the National Alliance for Research on Schizophrenia and Depression (ALB). Initial study results were presented at the 2008 Society for Research on Nicotine and Tobacco meeting. We thank Josephine Ribe and Michael Clark for technical support in performing positron emission tomography and magnetic resonance imaging scans, respectively.
Author information
Authors and Affiliations
Corresponding author
Additional information
DISCLOSURE
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Costello, M., Mandelkern, M., Shoptaw, S. et al. Effects of Treatment for Tobacco Dependence on Resting Cerebral Glucose Metabolism. Neuropsychopharmacol 35, 605–612 (2010). https://doi.org/10.1038/npp.2009.165
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/npp.2009.165
Keywords
This article is cited by
-
Lost in Translation: the Gap Between Neurobiological Mechanisms and Psychosocial Treatment Research for Substance Use Disorders
Current Addiction Reports (2021)
-
Altered spontaneous activity of posterior cingulate cortex and superior temporal gyrus are associated with a smoking cessation treatment outcome using varenicline revealed by regional homogeneity
Brain Imaging and Behavior (2017)
-
Neural correlates of 12-h abstinence-induced craving in young adult smokers: a resting-state study
Brain Imaging and Behavior (2017)
-
Neuroimaging the Effectiveness of Substance Use Disorder Treatments
Journal of Neuroimmune Pharmacology (2016)
-
Altered spontaneous brain activity in heavy smokers revealed by regional homogeneity
Psychopharmacology (2015)