Abstract
Clinical evidence suggests that after initiation of dopaminergic medications some patients with Parkinson's disease (PD) develop psychotic symptoms, such as hallucinations and delusions. Here, we tested the hypothesis that the neurocognitive basis of this phenomenon can be defined as the formation of arbitrary and illusory associations between conditioned stimuli and reward signals, called aberrant salience. Young, never-medicated PD patients and matched controls were assessed on a speeded reaction time task in which the probe stimulus was preceded by conditioned stimuli that could signal monetary reward by color or shape. The patients and controls were re-evaluated after 12 weeks during which the patients received a dopamine agonist (pramipexole or ropinirole). Results indicated that dopamine agonists increased both adaptive and aberrant salience in PD patients, that is, formation of real and illusory associations between conditioned stimuli and reward, respectively. This effect was present when associations were assessed by means of faster responding after conditioned stimuli signaling reward (implicit salience) and overt rating of stimulus–reward links (explicit salience). However, unusual feelings and experiences, which are subclinical manifestations of psychotic-like symptoms, were specifically related to irrelevant and illusory stimulus–reward associations (aberrant salience) in PD patients receiving dopamine agonists. The learning of relevant and real stimulus–reward associations (adaptive salience) was not related to unusual experiences. These results suggest that dopamine agonists may increase psychotic-like experiences in young patients with PD, possibly by facilitating dopaminergic transmission in the ventral striatum, which results in aberrant associations between conditioned stimuli and reward.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Berridge KC (2007). The debate over dopamine's role in reward: the case for incentive salience. Psychopharmacology (Berl) 191: 391–431.
Bódi N, Kéri S, Nagy H, Moustafa A, Myers CE, Daw N et al (2009). Reward-learning and the novelty-seeking personality: a between- and within-subjects study of the effects of dopamine agonists on young Parkinson's patients. Brain 132: 2385–2395.
Cirino PT, Chin CE, Sevcik RA, Wolf M, Lovett M, Morris RD (2002). Measuring socioeconomic status: reliability and preliminary validity for different approaches. Assessment 9: 145–155.
Cools R, Barker RA, Sahakian BJ, Robbins TW (2001). Enhanced or impaired cognitive function in Parkinson's disease as a function of dopaminergic medication and task demands. Cereb Cortex 11: 1136–1143.
Cools R, Barker RA, Sahakian BJ, Robbins TW (2003). L-Dopa medication remediates cognitive inflexibility, but increases impulsivity in patients with Parkinson's disease. Neuropsychologia 41: 1431–1441.
Cools R, Altamirano L, D’Esposito M (2006). Reversal learning in Parkinson's disease depends on medication status and outcome valence. Neuropsychologia 44: 1663–1673.
Cools R, Rogers R, Barker RA, Robbins TW (2010a). Top-down attentional control in Parkinson's disease: salient considerations. J Cogn Neurosci 22: 848–859.
Cools R, Miyakawa A, Sheridan M, D′Esposito M (2010b). Enhanced frontal function in Parkinson's disease. Brain 133: 225–233.
Ecker D, Unrath A, Kassubek J, Sabolek M (2009). Dopamine agonists and their risk to induce psychotic episodes in Parkinson's disease: a case–control study. BMC Neurol 9: 23.
Frank MJ, Seeberger LC, O’reilly RC (2004). By carrot or by stick: cognitive reinforcement learning in parkinsonism. Science 306: 1940–1943.
Frank MJ, Samanta J, Moustafa AA, Sherman SJ (2007). Hold your horses: impulsivity, deep brain stimulation, and medication in parkinsonism. Science 318: 1309–1312.
Gerlach M, Double K, Arzberger T, Leblhuber F, Tatschner T, Riederer P (2003). Dopamine receptor agonists in current clinical use: comparative dopamine receptor binding profiles defined in the human striatum. J Neural Transm 110: 1119–1127.
Gotham AM, Brown RG, Marsden CD (1988). Frontal’ cognitive function in patients with Parkinson's disease ‘on’ and ‘off’ levodopa. Brain 111: 299–321.
Graef S, Biele G, Krugel LK, Marzinzik F, Wahl M, Wotka J et al (2010). Differential influence of levodopa on reward-based learning in Parkinson's disease. Front Hum Neurosci 4: 169.
Hoehn MM, Yahr MD (1967). Parkinsonism: onset, progression and mortality. Neurology 17: 427–442.
Housden CR, O′Sullivan SS, Joyce EM, Lees AJ, Roiser JP (2010). Intact reward learning but elevated delay discounting in Parkinson's disease patients with impulsive-compulsive spectrum behaviors. Neuropsychopharmacology 35: 2155–2164.
Hughes AJ, Daniel SE, Kilford L, Lees AJ (1992). Accuracy of clinical diagnosis of idiopathic Parkinson's disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 55: 181–184.
Ishibashi K, Ishii K, Oda K, Mizusawa H, Ishiwata K (2011). Binding of pramipexole to extrastriatal dopamine D2/D3 receptors in the human brain: a positron emission tomography study using 11C-FLB 457. PLoS One 9: e17723.
Jahanshahi M, Wilkinson L, Gahir H, Dharminda A, Lagnado DA (2010). Medication impairs probabilistic classification learning in Parkinson's disease. Neuropsychologia 48: 1096–1103.
Kapur S (2003). Psychosis as a state of aberrant salience: a framework linking biology, phenomenology, and pharmacology in schizophrenia. Am J Psychiatry 160: 13–23.
King R, Barchas JD, Huberman BA (1984). Chaotic behavior in dopamine neurodynamics. Proc Natl Acad Sci USA 81: 1244–1247.
Kish SJ, Shannak K, Hornykiewicz O (1988). Uneven pattern of dopamine loss in the striatum of patients with idiopathic Parkinson's disease. Pathophysiologic and clinical implications. N Engl J Med 318: 876–880.
Knutson B, Bjork JM, Fong GW, Hommer D, Mattay VS, Weinberger DR (2004). Amphetamine modulates human incentive processing. Neuron 43: 261–269.
Kobayakawa M, Tsuruya N, Kawamura M (2010). Sensitivity to reward and punishment in Parkinson's disease: an analysis of behavioral patterns using a modified version of the Iowa gambling task. Parkinsonism Relat Disord 16: 453–457.
Kosaka H, Omori M, Murata T, Iidaka T, Yamada H, Okada T et al (2002). Differential amygdala response during facial recognition in patients with schizophrenia: an fMRI study. Schizophr Res 57: 87–95.
Lang AE, Fahn S (1989). Assessment of Parkinson's disease. In: Munsat TL (ed) Quantification of Neurologic Deficit. Butterworth-Heinemann: Boston, Mass. pp 285–309.
MacDonald PA, Macdonald AA, Seergobin KN, Tamjeedi R, Ganjavi H, Provost JS et al (2011). The effect of dopamine therapy on ventral and dorsal striatum-mediated cognition in Parkinson's disease: support from functional MRI. Brain 134: 1447–1463.
Maia TV, Frank MJ (2011). From reinforcement learning models to psychiatric and neurological disorders. Nat Neurosci 14: 154–162.
Mannan SK, Hodgson TL, Husain M, Kennard C (2008). Eye movements in visual search indicate impaired saliency processing in Parkinson's disease. Prog Brain Res 171: 559–562.
Mason O, Claridge G, Jackson M (1995). New scales for the assessment of schizotypy. Pers Indiv Differ 18: 7–13.
McGowan S, Lawrence AD, Sales T, Quested D, Grasby P (2004). Presynaptic dopaminergic dysfunction in schizophrenia: a positron emission tomographic [18F]fluorodopa study. Arch Gen Psychiatry 61: 134–142.
Mehler-Wex C, Riederer P, Gerlach M (2006). Dopaminergic dysbalance in distinct basal ganglia neurocircuits: implications for the pathophysiology of Parkinson's disease, schizophrenia and attention deficit hyperactivity disorder. Neurotox Res 10: 167–179.
Miller R (1993). Striatal dopamine in reward and attention: a system for understanding the symptomatology of acute schizophrenia and mania. Int Rev Neurobiol 35: 161–278.
Moore JW, Schneider SA, Schwingenschuh P, Moretto G, Bhatia KP, Haggard P (2010). Dopaminergic medication boosts action–effect binding in Parkinson's disease. Neuropsychologia 48: 1125–1132.
Mountjoy CQ, Roth M (1982). Studies in the relationship between depressive disorders and anxiety states. Part 1. Rating scales. J Affect Disord 4: 127–147.
Pessiglione M, Seymour B, Flandin G, Dolan RJ, Frith CD (2006). Dopamine-dependent prediction errors underpin reward-seeking behaviour in humans. Nature 442: 1042–1045.
Roiser JP, Stephan KE, den Ouden HE, Barnes TR, Friston KJ, Joyce EM (2009). Do patients with schizophrenia exhibit aberrant salience? Psychol Med 39: 199–209.
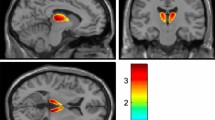
Roiser JP, Stephan KE, den Ouden HE, Friston KJ, Joyce EM (2010). Adaptive and aberrant reward prediction signals in the human brain. Neuroimage 50: 657–664.
Schmidt K, Roiser JP (2009). Assessing the construct validity of aberrant salience. Front Behav Neurosci 3: 58.
Schultz W (2007). Multiple dopamine functions at different time courses. Annu Rev Neurosci 30: 259–288.
Shaner A (1999). Delusions, superstitious conditioning and chaotic dopamine neurodynamics. Med Hypotheses 52: 119–123.
Shohamy D, Myers CE, Geghman KD, Sage J, Gluck MA (2006). L-dopa impairs learning, but spares generalization, in Parkinson's disease. Neuropsychologia 44: 774–784.
Stoner SC, Dahmen MM, Makos M, Lea JW, Carver LJ, Rasu RS (2009). An exploratory retrospective evaluation of ropinirole-associated psychotic symptoms in an outpatient population treated for restless legs syndrome or Parkinson's disease. Ann Pharmacother 43: 1426–1432.
Subramanian L, Hindle JV, Jackson MC, Linden DE (2010). Dopamine boosts memory for angry faces in Parkinson's disease. Mov Disord 25: 2792–2799.
van Eimeren T, Ballanger B, Pellecchia G, Miyasaki JM, Lang AE, Strafella AP (2009). Dopamine agonists diminish value sensitivity of the orbitofrontal cortex: a trigger for pathological gambling in Parkinson's disease? Neuropsychopharmacology 34: 2758–2766.
Verbaan D, van Rooden SM, Visser M, Marinus J, Emre M, van Hilten JJ (2009). Psychotic and compulsive symptoms in Parkinson's disease. Mov Disord 24: 738–744.
Voss M, Moore J, Hauser M, Gallinat J, Heinz A, Haggard P (2010). Altered awareness of action in schizophrenia: a specific deficit in predicting action consequences. Brain 133: 3104–3112.
Voon V, Fox SH (2007). Medication-related impulse control and repetitive behaviors in Parkinson disease. Arch Neurol 64: 1089–1096.
Wechsler D (1981). Wechsler Adult Intelligence Scale—Revised Manual. Psychological Corporation: New York, NY.
Weintraub D, Burn DJ (2011). Parkinson's disease: the quintessential neuropsychiatric disorder. Mov Disord 26: 1022–1031.
Winstanley CA, Cocker PJ, Rogers RD (2011). Dopamine modulates reward expectancy during performance of a slot machine task in rats: evidence for a ‘near-miss’ effect. Neuropsychopharmacology 36: 913–925.
Wyvell CL, Berridge KC (2000). Intra-accumbens amphetamine increases the conditioned incentive salience of sucrose reward: enhancement of reward ‘wanting’ without enhanced ‘liking’ or response reinforcement. J Neurosci 20: 8122–8130.
Ye Z, Hammer A, Camara E, Münte TF (2011). Pramipexole modulates the neural network of reward anticipation. Hum Brain Mapp 32: 800–811.
Yin HH, Knowlton BJ (2006). The role of the basal ganglia in habit formation. Nat Rev Neurosci 7: 464–476.
Young RC, Biggs JT, Ziegler VE, Meyer DA (1978). A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry 133: 429–435.
Acknowledgements
This study was supported by the Hungarian Research Fund (OTKA NF72488) and TAMOP-4.2.1.B-09/1/KMR.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Nagy, H., Levy-Gigi, E., Somlai, Z. et al. The Effect of Dopamine Agonists on Adaptive and Aberrant Salience in Parkinson's Disease. Neuropsychopharmacol 37, 950–958 (2012). https://doi.org/10.1038/npp.2011.278
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/npp.2011.278
Keywords
This article is cited by
-
Schizotypy in Parkinson’s disease predicts dopamine-associated psychosis
Scientific Reports (2021)
-
Dopaminergic drug treatment remediates exaggerated cingulate prediction error responses in obsessive-compulsive disorder
Psychopharmacology (2019)
-
A single dose of l-DOPA changes perceptual experiences and decreases latent inhibition in Parkinson’s disease
Journal of Neural Transmission (2017)
-
A pilot psychometric study of aberrant salience state in patients with Parkinson’s disease and its association with dopamine replacement therapy
Neurological Sciences (2014)