Abstract
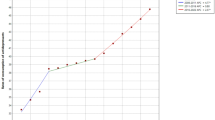
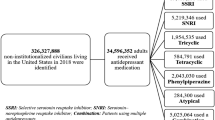
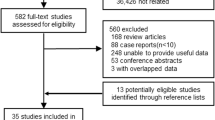
Increased sympathetic activity has been hypothesized to have a role in the elevated somatic disease risk in persons with depressive or anxiety disorders. However, it remains unclear whether increased sympathetic activity reflects a direct effect of anxiety or depression or an indirect effect of antidepressant medication. The aim of this study was to test longitudinally whether cardiac sympathetic control, measured by pre-ejection period (PEP), was increased by depression/anxiety status and by antidepressant use. Cross-sectional and longitudinal data were from a depression and anxiety cohort: the Netherlands Study of Depression and Anxiety (NESDA). Baseline data of 2838 NESDA subjects (mean age 41.7 years, 66.7% female) and 2-year follow-up data of 2226 subjects were available for analyses. Included were subjects with and without depressive/anxiety disorders, using or not using different antidepressants at baseline or follow-up. The PEP was measured non-invasively by 1.5 h of ambulatory impedance cardiography. Cross-sectional analyses compared PEP across psychopathology and antidepressant groups. Longitudinal analyses compared 2-year changes in PEP in relation to changes in psychopathology and antidepressant use. Cross-sectional analyses showed that antidepressant-naïve depressive/anxious subjects had comparable PEP as controls, whereas subjects using tricyclic (TCA) or combined serotonergic/noradrenergic antidepressants (SNRI) had significantly shorter PEP compared with controls. In contrast, subjects using selective serotonin re-uptake inhibitors (SSRIs) had longer PEP than controls. Longitudinal results confirmed these findings: compared with 2-year change in PEP in continuous non-users (+2 ms), subjects who started TCA or SNRI treatment showed significantly shortened PEP (−11 ms, p=0.005 and p<0.001), whereas subjects who started SSRI treatment showed significant prolongation of PEP (+9 ms, p=0.002). Reversed findings were observed among those who stopped antidepressant use. These findings suggest that depressive and anxiety disorders are not associated with increased cardiac sympathetic control. However, results pose that TCA and SNRI use increases sympathetic control, whereas SSRI use decreases sympathetic control.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Ahrens T, Deuschle M, Krumm B, van der PG, den Boer JA, Lederbogen F (2008). Pituitary-adrenal and sympathetic nervous system responses to stress in women remitted from recurrent major depression. Psychosom Med 70: 461–467.
American Psychiatric Association (2001). Diagnostic and Statistical Manual of Mental Disorders, 4th edn, Washington.
Barton DA, Dawood T, Lambert EA, Esler MD, Haikerwal D, Brenchley C et al (2007). Sympathetic activity in major depressive disorder: identifying those at increased cardiac risk? J Hypertens 25: 2117–2124.
Berntson GG, Cacioppo JT, Binkley PF, Uchino BN, Quigley KS, Fieldstone A (1994). Autonomic cardiac control. III. Psychological stress and cardiac response in autonomic space as revealed by pharmacological blockades. Psychophysiology 31: 599–608.
Booth M (2000). Assessment of physical activity: an international perspective. Res Q Exerc Sport 71: S114–S120.
Bruno RL, Myers SJ, Glassman AH (1983). A correlational study of cardiovascular autonomic functioning and unipolar depression. Biol Psychiatry 18: 227–235.
Cacioppo JT, Berntson GG, Binkley PF, Quigley KS, Uchino BN, Fieldstone A (1994). Autonomic cardiac control. II. Noninvasive indices and basal response as revealed by autonomic blockades. Psychophysiology 31: 586–598.
Cohen J (1988). Statistical power analysis for the behavioral sciences 2nd (edn). Lawrence Earlbaurn Associates: Hillsdale, NJ.
Cohen HW, Gibson G, Alderman MH (2000). Excess risk of myocardial infarction in patients treated with antidepressant medications: association with use of tricyclic agents. Am J Med 108: 2–8.
Dawood T, Schlaich M, Brown A, Lambert G (2009). Depression and blood pressure control: all antidepressants are not the same. Hypertension 54: e1.
de Geus EJ, Willemsen GH, Klaver CH, van Doornen LJ (1995). Ambulatory measurement of respiratory sinus arrhythmia and respiration rate. Biol Psychol 41: 205–227.
Degner D, Grohmann R, Kropp S, Ruther E, Bender S, Engel RR et al (2004). Severe adverse drug reactions of antidepressants: results of the German multicenter drug surveillance program AMSP. Pharmacopsychiatry 37 (Suppl 1): S39–S45.
Eaker ED, Sullivan LM, Kelly-Hayes M, D’Agostino Sr RB, Benjamin EJ (2005). Tension and anxiety and the prediction of the 10-year incidence of coronary heart disease, atrial fibrillation, and total mortality: the Framingham Offspring Study. Psychosom Med 67: 692–696.
Eckberg DL (2003). The human respiratory gate. J Physiol 548: 339–352.
Eisenhofer G, Friberg P, Rundqvist B, Quyyumi AA, Lambert G, Kaye DM et al (1996). Cardiac sympathetic nerve function in congestive heart failure. Circulation 93: 1667–1676.
Elam M, Thoren P, Svensson TH (1986). Locus coeruleus neurons and sympathetic nerves: activation by visceral afferents. Brain Res 375: 117–125.
Elam M, Yao T, Svensson TH, Thoren P (1984). Regulation of locus coeruleus neurons and splanchnic, sympathetic nerves by cardiovascular afferents. Brain Res 290: 281–287.
Esler M, Alvarenga M, Lambert G, Kaye D, Hastings J, Jennings G et al (2004). Cardiac sympathetic nerve biology and brain monoamine turnover in panic disorder. Ann NY Acad Sci 1018: 505–514.
Esler M, Straznicky N, Eikelis N, Masuo K, Lambert G, Lambert E (2006). Mechanisms of sympathetic activation in obesity-related hypertension. Hypertension 48: 787–796.
Esler M, Turbott J, Schwarz R, Leonard P, Bobik A, Skews H et al (1982). The peripheral kinetics of norepinephrine in depressive illness. Arch Gen Psychiatry 39: 295–300.
Flaa A, Aksnes TA, Kjeldsen SE, Eide I, Rostrup M (2008a). Increased sympathetic reactivity may predict insulin resistance: an 18-year follow-up study. Metabolism 57: 1422–1427.
Flaa A, Sandvik L, Kjeldsen SE, Eide IK, Rostrup M (2008b). Does sympathoadrenal activity predict changes in body fat? An 18-y follow-up study. Am J Clin Nutr 87: 1596–1601.
Glassman A (2008). Depression and cardiovascular disease. Pharmacopsychiatry 41: 221–225.
Gold PW, Wong ML, Goldstein DS, Gold HK, Ronsaville DS, Esler M et al (2005). Cardiac implications of increased arterial entry and reversible 24-h central and peripheral norepinephrine levels in melancholia. Proc Natl Acad Sci USA 102: 8303–8308.
Grant MM, Weiss JM (2001). Effects of chronic antidepressant drug administration and electroconvulsive shock on locus coeruleus electrophysiologic activity. Biol Psychiatry 49: 117–129.
Grossman P, van Beek J, Wientjes C (1990). A comparison of three quantification methods for estimation of respiratory sinus arrhythmia. Psychophysiology 27: 702–714.
Guinjoan SM, Bernabo JL, Cardinali DP (1995). Cardiovascular tests of autonomic function and sympathetic skin responses in patients with major depression. J Neurol Neurosurg Psychiatry 59: 299–302.
Harris WS, Schoenfeld CD, Weissler AM (1967). Effects of adrenergic receptor activation and blockade on the systolic preejection period, heart rate, and arterial pressure in man. J Clin Invest 46: 1704–1714.
Helke CJ, Capuano S, Tran N, Zhuo H (1997). Immunocytochemical studies of the 5-HT(1A) receptor in ventral medullaryneurons that project to the intermediolateral cell column and contain serotonin or tyrosine hydroxylase immunoreactivity. J Comp Neurol 379: 261–270.
Houtveen JH, de Groot PF, de Geus EJ (2005). Effects of variation in posture and respiration on RSA and pre-ejection period 1. Psychophysiology 42: 713–719.
Howell C, Wilson AD, Waring WS (2007). Cardiovascular toxicity due to venlafaxine poisoning in adults: a review of 235 consecutive cases. Br J Clin Pharmacol 64: 192–197.
Koschke M, Boettger MK, Schulz S, Berger S, Terhaar J, Voss A et al (2009). Autonomy of autonomic dysfunction in major depression. Psychosom Med 71: 852–860.
Krzeminski K, Kruk B, Nazar K, Ziemba AW, Cybulski G, Niewiadomski W (2000). Cardiovascular, metabolic and plasma catecholamine responses to passive and active exercises. J Physiol Pharmacol 51: 267–278.
Lamers F, Hoogendoorn A, Smit JH, van Dyck R, Zitman FG, Nolen WA et al (2012). Socio-demographic and psychiatric determinants of attrition in the Netherlands Study of Depression and Anxiety (NESDA). Compr Psychiatry 53: 63–70.
Licht CMM, de Geus EJ, Penninx BWJH (2009a). Depression and blood pressure control: all antidepressants are not the same. Hypertension 54: e2.
Licht CMM, de Geus EJ, Seldenrijk A, van Hout HP, Zitman FG, van Dyck R et al (2009b). Depression is associated with decreased blood pressure, but antidepressant use increases the risk for hypertension. Hypertension 53: 631–638.
Licht CMM, de Geus EJ, van Dyck R, Penninx BWJH (2009c). Association between anxiety disorders and heart rate variability in the Netherlands Study of Depression and Anxiety (NESDA). Psychosom Med 71: 508–518.
Licht CMM, de Geus EJ, van Dyck R, Penninx BWJH (2010). Longitudinal evidence for unfavorable effects of antidepressants on heart rate variability. Biol Psychiatry 68: 861–868.
Licht CMM, de Geus EJ, Zitman FG, Hoogendijk WJ, van Dyck R, Penninx BWJH (2008). Association between major depressive disorder and heart rate variability in the Netherlands Study of Depression and Anxiety (NESDA). Arch Gen Psychiatry 65: 1358–1367.
Light KC, Kothandapani RV, Allen MT (1998). Enhanced cardiovascular and catecholamine responses in women with depressive symptoms. Int J Psychophysiol 28: 157–166.
Masuo K, Katsuya T, Fu Y, Rakugi H, Ogihara T, Tuck ML (2005). Beta2-adrenoceptor polymorphisms relate to insulin resistance and sympathetic overactivity as early markers of metabolic disease in nonobese, normotensive individuals. Am J Hypertens 18: 1009–1014.
Masuo K, Rakugi H, Ogihara T, Esler MD, Lambert GW (2010). Cardiovascular and renal complications of type 2 diabetes in obesity: role of sympathetic nerve activity and insulin resistance. Curr Diabetes Rev 6: 58–67.
Mezzacappa ES, Kelsey RM, Katkin ES (1999). The effects of epinephrine administration on impedance cardiographic measures of cardiovascular function. Int J Psychophysiol 31: 189–196.
Miyamoto Y, Higuchi J, Abe Y, Hiura T, Nakazono Y, Mikami T (1983). Dynamics of cardiac output and systolic time intervals in supine and upright exercise. J Appl Physiol 55: 1674–1681.
Nalivaiko E (2006). 5-HT(1A) receptors in stress-induced cardiac changes: a possible link between mental and cardiac disorders. Clin Exp Pharmacol Physiol 33: 1259–1264.
Nelesen RA, Shaw R, Ziegler MG, Dimsdale JE (1999). Impedance cardiography-derived hemodynamic responses during baroreceptor testing with amyl nitrite and phenylephrine: a validity and reliability study. Psychophysiology 36: 105–108.
Newlin DB, Levenson RW (1979). Pre-ejection period: measuring beta-adrenergic influences upon the heart. Psychophysiology 16: 546–553.
Nicholson A, Kuper H, Hemingway H (2006). Depression as an aetiologic and prognostic factor in coronary heart disease: a meta-analysis of 6362 events among 146 538 participants in 54 observational studies. Eur Heart J 27: 2763–2774.
Norton JM (2001). Toward consistent definitions for preload and afterload. Adv Physiol Educ 25: 53–61.
Penninx BWJH, Beekman AT, Honig A, Deeg DJ, Schoevers RA, van Eijk JT et al (2001). Depression and cardiac mortality: results from a community-based longitudinal study. Arch Gen Psychiatry 58: 221–227.
Penninx BWJH, Beekman AT, Smit JH, Zitman FG, Nolen WA, Spinhoven P et al (2008). The Netherlands Study of Depression and Anxiety (NESDA): rationale, objectives and methods. Int J Methods Psychiatr Res 17: 121–140.
Roth WT, Doberenz S, Dietel A, Conrad A, Mueller A, Wollburg E et al (2008). Sympathetic activation in broadly defined generalized anxiety disorder. J Psychiatr Res 42: 205–212.
Roth WT, Telch MJ, Taylor CB, Agras WS (1988). Autonomic changes after treatment of agoraphobia with panic attacks. Psychiatry Res 24: 95–107.
Rush AJ, Gullion CM, Basco MR, Jarrett RB, Trivedi MH (1996). The Inventory of Depressive Symptomatology (IDS): psychometric properties. Psychol Med 26: 477–486.
Schachinger H, Weinbacher M, Kiss A, Ritz R, Langewitz W (2001). Cardiovascular indices of peripheral and central sympathetic activation. Psychosom Med 63: 788–796.
Sherwood A, Allen MT, Fahrenberg J, Kelsey RM, Lovallo WR, van Doornen LJ (1990). Methodological guidelines for impedance cardiography. Psychophysiology 27: 1–23.
Sherwood A, Allen MT, Obrist PA, Langer AW (1986). Evaluation of beta-adrenergic influences on cardiovascular and metabolic adjustments to physical and psychological stress. Psychophysiology 23: 89–104.
Shimizu S, Akiyama T, Kawada T, Shishido T, Mizuno M, Kamiya A et al (2010). In vivo direct monitoring of interstitial norepinephrine levels at the sinoatrial node. Auton Neurosci 152: 115–118.
Shores MM, Pascualy M, Lewis NL, Flatness D, Veith RC (2001). Short-term sertraline treatment suppresses sympathetic nervous system activity in healthy human subjects. Psychoneuroendocrinology 26: 433–439.
Smith JJ, Muzi M, Barney JA, Ceschi J, Hayes J, Ebert TJ (1989). Impedance-derived cardiac indices in supine and upright exercise. Ann Biomed Eng 17: 507–515.
Steer RA, Kumar G, Ranieri WF, Beck AT (1995). Use of the Beck Anxiety Inventory with adolescent psychiatric outpatients. Psychol Rep 76: 459–465.
Svedenhag J, Martinsson A, Ekblom B, Hjemdahl P (1986). Altered cardiovascular responsiveness to adrenaline in endurance-trained subjects. Acta Physiol Scand 126: 539–550.
Svensson TH (1987). Peripheral, autonomic regulation of locus coeruleus noradrenergic neurons in brain: putative implications for psychiatry and psychopharmacology. Psychopharmacology (Berl) 92: 1–7.
Tata LJ, West J, Smith C, Farrington P, Card T, Smeeth L et al (2005). General population based study of the impact of tricyclic and selective serotonin reuptake inhibitor antidepressants on the risk of acute myocardial infarction. Heart 91: 465–471.
van Reedt Dortland AK, Giltay EJ, van VT, Zitman FG, Penninx BW (2010). Metabolic syndrome abnormalities are associated with severity of anxiety and depression and with tricyclic antidepressant use. Acta Psychiatr Scand 122: 30–39.
Veith RC, Lewis N, Linares OA, Barnes RF, Raskind MA, Villacres EC et al (1994). Sympathetic nervous system activity in major depression. Basal and desipramine-induced alterations in plasma norepinephrine kinetics 5. Arch Gen Psychiatry 51: 411–422.
Veith RC, Raskind MA, Barnes RF, Gumbrecht G, Ritchie JL, Halter JB (1983). Tricyclic antidepressants and supine, standing, and exercise plasma norepinephrine levels. Clin Pharmacol Ther 33: 763–769.
Vincent S, Bieck PR, Garland EM, Loghin C, Bymaster FP, Black BK et al (2004). Clinical assessment of norepinephrine transporter blockade through biochemical and pharmacological profiles. Circulation 109: 3202–3207.
Weissler AM, Harris WS, Schoenfeld CD (1968). Systolic time intervals in heart failure in man. Circulation 37: 149–159.
Wilkinson DJ, Thompson JM, Lambert GW, Jennings GL, Schwarz RG, Jefferys D et al (1998). Sympathetic activity in patients with panic disorder at rest, under laboratory mental stress, and during panic attacks. Arch Gen Psychiatry 55: 511–520.
Willemsen GH, de Geus EJ, Klaver CH, van Doornen LJ, Carroll D (1996). Ambulatory monitoring of the impedance cardiogram. Psychophysiology 33: 184–193.
Winzer A, Ring C, Carroll D, Willemsen G, Drayson M, Kendall M (1999). Secretory immunoglobulin A and cardiovascular reactions to mental arithmetic, cold pressor, and exercise: effects of beta-adrenergic blockade. Psychophysiology 36: 591–601.
Wittchen HU (1994). Reliability and validity studies of the WHO—Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res 28: 57–84.
Wolf GK, Belz GG, Stauch M (1978). Systolic time intervals—correction for heart rate. Basic Res Cardiol 73: 85–96.
World Health Organization Collaborating Centre for Drug Statistics Methodology (2010). Anatomical Therapeutic Chemical (ATC) classification. Available at: http://www.whocc.no/atcddd.
Acknowledgements
The infrastructure for the NESDA study (http://www.nesda.nl) is funded through the Geestkracht program of the Netherlands Organization for Health Research and Development (Zon-Mw, grant number 10-000-1002) and is supported by participating universities and mental health-care organizations (VU University Medical Center, GGZ inGeest, Arkin, Leiden University Medical Center, GGZ Rivierduinen, University Medical Center Groningen, Lentis, GGZ Friesland, GGZ Drenthe, Scientific Institute for Quality of Healthcare (IQ healthcare), Netherlands Institute for Health Services Research (NIVEL) and Netherlands Institute of Mental Health and Addiction (Trimbos). Data analyses were supported by NWO grant (Vidi, 917.66.320) to Dr Penninx and an EMGO fellowship to Dr Licht.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
PowerPoint slides
Rights and permissions
About this article
Cite this article
Licht, C., Penninx, B. & de Geus, E. Effects of Antidepressants, but not Psychopathology, on Cardiac Sympathetic Control: A Longitudinal Study. Neuropsychopharmacol 37, 2487–2495 (2012). https://doi.org/10.1038/npp.2012.107
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/npp.2012.107
Keywords
This article is cited by
-
Non-suicidal Self-injury History Moderates the Association Between Maternal Emotional Support and Adolescent Affect During Conflict
Child Psychiatry & Human Development (2024)
-
Drug-Induced Hypertension: Focus on Mechanisms and Management
Current Hypertension Reports (2017)
-
Systolic Time Intervals and New Measurement Methods
Cardiovascular Engineering and Technology (2016)
-
Pain in dementia: prevalence and associated factors: protocol of a multidisciplinary study
BMC Geriatrics (2015)
-
Behandlung der Depression bei koronarer Herzerkrankung
Der Nervenarzt (2015)