Abstract
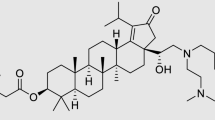
Anecdotal reports have surfaced concerning misuse of the HIV antiretroviral medication efavirenz ((4S)-6-chloro-4-(2-cyclopropylethynyl)-4-(trifluoromethyl)-2,4-dihydro-1H-3,1-benzoxazin-2-one) by HIV patients and non-infected teens who crush the pills and smoke the powder for its psychoactive effects. Molecular profiling of the receptor pharmacology of efavirenz pinpointed interactions with multiple established sites of action for other known drugs of abuse including catecholamine and indolamine transporters, and GABAA and 5-HT2A receptors. In rodents, interaction with the 5-HT2A receptor, a primary site of action of lysergic acid diethylamine (LSD), appears to dominate efavirenz’s behavioral profile. Both LSD and efavirenz reduce ambulation in a novel open-field environment. Efavirenz occasions drug-lever responding in rats discriminating LSD from saline, and this effect is abolished by selective blockade of the 5-HT2A receptor. Similar to LSD, efavirenz induces head-twitch responses in wild-type, but not in 5-HT2A-knockout, mice. Despite having GABAA-potentiating effects (like benzodiazepines and barbiturates), and interactions with dopamine transporter, serotonin transporter, and vesicular monoamine transporter 2 (like cocaine and methamphetamine), efavirenz fails to maintain responding in rats that self-administer cocaine, and it fails to produce a conditioned place preference. Although its molecular pharmacology is multifarious, efavirenz’s prevailing behavioral effect in rodents is consistent with LSD-like activity mediated via the 5-HT2A receptor. This finding correlates, in part, with the subjective experiences in humans who abuse efavirenz and with specific dose-dependent adverse neuropsychiatric events, such as hallucinations and night terrors, reported by HIV patients taking it as a medication.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Adams LM, Geyer MA (1982). LSD-induced alterations of locomotor patterns and exploration in rats. Psychopharmacology (Berl) 77: 179–185.
Adams LM, Geyer MA (1985). Effects of DOM and DMT in a proposed animal model of hallucinogenic activity. Prog Neuropsychopharmacol Biol Psychiatry 9: 121–132.
Anthony JC, Warner LA, Kessler RC (1994). Comparative epidemiology of dependence on tobacco, alcohol, controlled substances, and inhalants: basic findings from the national comorbidity survey. Exp Clin Psychopharmacol 2: 244–268.
Arribas JR (2003). Efavirenz: enhancing the gold standard. Int J STD AIDS 14 (Suppl 1): 6–14.
Best BM, Goicoechea M (2008). Efavirenz—still first-line king? Expert Opin Drug Metab Toxicol 4: 965–972.
Best BM, Koopmans PP, Letendre SL, Capparelli EV, Rossi SS, Clifford DB et alCHARTER Group (2011). Efavirenz concentrations in CSF exceed IC50 for wild-type HIV. J Antimicrob Chemother 66: 354–357.
Brown JM, Hanson GR, Fleckenstein AE (2001). Regulation of the vesicular monoamine transporter-2: a novel mechanism for cocaine and other psychostimulants. J Pharmacol Exp Ther 296: 762–767.
Central Intelligence Agency (CIA) World Fact Book (2009). Country Comparisons—HIV/AIDS—adult prevalence rate. Data from 2007 estimates Available at: https://www.cia.gov/library/publications/the-world-factbook/rankorder/2155rank.html.
Cespedes MS, Aberg JA (2006). Neuropsychiatric complications of antiretroviral therapy. Drug Saf 29: 865–874.
Cesura AM, Bertocci B, Da Prada M (1990). Binding of [3H]dihydrotetrabenazine and [125I]azidoiodoketanserin photoaffinity labeling of the monoamine transporter of platelet 5-HT organelles. Eur J Pharmacol 1990 186: 95–104.
Chen CY, Storr CL, Anthony JC (2009). Early-onset drug use and risk for drug dependence problems. Addict Behav 34: 319–322.
Cunningham CL, Gremel CM, Groblewski PA (2006). Drug-induced conditioned place preference and aversion in mice. Nat Protoc 1: 1662–1670.
Dybul M, Fauci AS, Bartlett JG, Kaplan JE, Pau AK, Panel on Clinical Practices for Treatment of HIV (2002). Guidelines for using antiretroviral agents among HIV-infected adults and adolescents. Ann Intern Med 137: 381–433.
Ericksen SS, Cummings DF, Weinstein H, Schetz JA (2009). Ligand selectivity of D2 dopamine receptors is modulated by changes in local dynamics produced by sodium binding. J Pharm Exp Ther 328: 40–54.
Erickson JD, Schafer MK, Bonner TI, Eiden LE, Weihe E (1996). Distinct pharmacological properties and distribution in neurons and endocrine cells of two isoforms of the human vesicular monoamine transporter. Proc Natl Acad Sci USA 93: 5166–5171.
Fantegrossi WE, Harrington AW, Kiessel CL, Eckler JR, Rabin RA, Winter JC et al (2006). Hallucinogen-like actions of 5-methoxy-N,N-diisopropyltryptamine in mice and rats. Pharmacol Biochem Behav 83: 122–129.
Fantegrossi WE, Murnane KS, Reissig CJ (2008). The behavioral pharmacology of hallucinogens. Biochem Pharmacol 75: 17–33.
Fiorella D, Rabin RA, Winter JC (1995). The role of the 5-HT2A and 5-HT2C receptors in the stimulus effects of hallucinogenic drugs. I: Antagonist correlation analysis. Psychopharmacology (Berl) 121: 347–356.
Gatch MB, Rutledge M, Carbonaro T, Forster MJ (2009). Comparison of the discriminative stimulus effects of dimethyltryptamine with different classes of psychoactive compounds in rats. Psychopharmacology 204: 715–724.
Glennon RA, Titeler M, McKenney JD (1984). Evidence for 5-HT2 involvement in the mechanism of action of hallucinogenic agents. Life Sci 35: 2505–2511.
Gonzalez LA, Gatch MB, Taylor CM, Bell-Horner CL, Forster MJ, Dillon GH (2009). Carisoprodol-mediated modulation of GABAA receptors: in vitro and in vivo studies. J Pharmacol Exp Ther 329: 827–837.
González-Maeso J, Weisstaub NV, Zhou M, Chan P, Ivic L, Ang R et al (2007). Hallucinogens recruit specific cortical 5-HT(2A) receptor-mediated signaling pathways to affect behavior. Neuron 53: 439–452.
Gonzalez-Maeso J, Ang RL, Yuen T, Chan P, Weisstaub NV, Lopez-Gimenez JF et al (2008). Identification of a serotonin/glutamate receptor complex implicated in psychosis. Nature 452: 93–97.
Gulick RM, Ribaudo HJ, Shikuma CM, Lustgarten S, Squires KE, Meyer WA et al (2004). Triple-nucleoside regimens versus efavirenz-containing regimens for the initial treatment. N Engl J Med 350: 1850–1861.
Grailhe R, Waeber C, Dulawa SC, Hornung JP, Zhuang X, Brunner D et al (1999). Increased exploratory activity and altered response to LSD in mice lacking the 5-HT(5A) receptor. Neuron 22: 581–591.
Gutiérrez F, Navarro A, Padilla S, Antón R, Masiá M, Borrás J et al (2005). Prediction of neuropsychiatric adverse events associated with long-term efavirenz therapy, using plasma drug level monitoring. Clin Infect Dis 41: 1648–1653.
Halberstadt AL, van der Heijden I, Ruderman MA, Risbrough VB, Powell SB (2009). 5-HT2A and 5-HT2C receptors exert opposing effects on locomotor activity in mice (2009). Neuropsychopharmacology 34: 1958–1967.
Hammer SM, Eron JJ Jr, Reiss P, Schooley RT, Thompson MA, Walmsley S et al (2008). International AIDS Society-USA. Antiretroviral treatment of adult HIV infection: 2008 recommendations of the International AIDS Society-USA panel. JAMA 300: 555–570.
Han DD, Gu HH (2006). Comparison of the monoamine transporters from human and mouse in their sensitivities to psychostimulant drugs. BMC Pharmacol 6: 7.
Huang RQ, Singh M, Dillon GH (2010). Genistein directly inhibits NMDA receptors in mouse hippocampal neurons. Neuropharmacology 58: 1246–1251.
Huestis MA, Gorelick DA, Heishman SJ, Preston KL, Nelson RA, Moolchan ET et al (2001). Blockade of effects of smoked marijuana by the CB1-selective cannabinoid receptor antagonist SR141716. Arch Gen Psychiatry 58: 322–328.
Lacivita E, Paola De Giorgio P, Lee IT, Rodeheaver SI, Weiss BA, Fracasso C et al (2010). Design, synthesis, radiolabeling and in vivo evaluation of carbon-11 labeled N-[2-[4-(3-cyanopyridin-2-yl)piperazin-1-yl]ethyl]-3-methoxybenzamide, a potential PET tracer for the dopamine D4 receptors. J Med Chem 53: 7344–7355.
Marwaha A (2008). Getting High on HIV drugs in S Africa, BBC News, 8 December 2008 Available at: http://news.bbc.co.uk/2/hi/africa/7768059.stm.
Meltzer HY, Fessler RG, Simonovic M, Doherty J, Fang VS (1977). Lysergic acid diethylamide: evidence for stimulation of pituitary dopamine receptors. Psychopharmacology (Berl) 54: 39–44.
National Research Council (2003) Guidelines for the care and use of mammals in neuroscience and behavioral research. The National Academies Press: Washington, DC.
Nichols DE (2004). Hallucinogens. Pharmacol Ther 101: 131–181.
Patel AK, Patel KK (2006). Future implications: compliance and failure with antiretroviral treatment. J Postgrad Med 52: 197–200.
Rossi S, Yaksh T, Bentley H, van den Brande G, Grant I, Ellis R (2006). Characterization of interference with 6 commercial delta-9-tetrahydrocannabinol immunoassays by Efavirenz (glucuronide) in urine. Clin Chem 52: 896–898.
Sciutto J (2009). ABC World News Report (4 May 2009) Shorten version 6 April 2009: ‘No Turning Back’: Teens Abuse HIV Drugs. Teens in South Africa Smoke Anti-Retroviral Drug Efavirenz for Cheap High portions archived at http://www.youtube.com/watch?v=hjVtthQJnyU.
Sierra-Madero J, Villasis-Keever A, Méndez P, Mosqueda-Gómez JL, Torres-Escobar I, Gutiérrez-Escolano F et al (2010). Prospective, randomized, open label trial of Efavirenz vs Lopinavir/Ritonavir in HIV+ treatment-naive subjects with CD4+<200 cell/mm3 in Mexico. J Acquir Immune Defic Syndr 53: 582–588.
Vazquez E (1999). Sustiva flashbacks. Posit Aware 10: 17.
Vollenweider FX, Vollenweider-Scherpenhuyzen MF, Bäbler A, Vogel H, Hell D (1998). Psilocybin induces schizophrenia-like psychosis in humans via a serotonin-2 agonist action. Neuroreport 9: 3897–3902.
Winter JC (2009). Hallucinogens as discriminative stimuli in animals: LSD, phenethylamines, and tryptamines. Psychopharmacology (Berl) 203: 251–263.
Acknowledgements
We thank Dr Michael Oglesby for critical reading of early versions of the manuscript, Dr Kathyrn Cunningham for insightful discussions related to this work, and Brian Weiss, Shahnawaz Amdani, Marshayla McPhaul, Terrell Holloway and Fatima Sahyouni for technical assistance. We also thank Dr David Lynch (University of Pennsylvania) for providing the cDNAs encoding rat NR1a, NR2A, and NR2B, Dr Eldo Kuzhikandathil (UMDNJ-New Jersey Medical School) for providing an Att20 cell line stably expressing the human D3 receptor, and Dr David B Bylund (University of Nebraska Medical Center) for providing the HEK293 cell line stably expressing the human α2C adrenergic receptor. This work was supported, in part, by the National Institutes of Health (Grant R01-MH063162 (JAS); K05DA17918 (CPF); R01 MH084894 (JGM); R01-DA022370 (GHD, MJF); N01DA-7-8872 (HHSN271200700014C) (MJF)), UNTHSC Intramural Grant RI-6015 (JAS, MG, and MJF), and institutional funds (JAS, MJF, and GHD). A portion of this work was also supported by the Intramural Research Programs of the National Institute on Drug Abuse and the National Institute on Alcohol Abuse and Alcoholism (KCR).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gatch, M., Kozlenkov, A., Huang, RQ. et al. The HIV Antiretroviral Drug Efavirenz has LSD-Like Properties. Neuropsychopharmacol 38, 2373–2384 (2013). https://doi.org/10.1038/npp.2013.135
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/npp.2013.135
Keywords
This article is cited by
-
A Systematic Review of Risk Factors and Consequences of Nyaope Usage: The Illicit Street Drug Containing HIV Antiretrovirals
AIDS and Behavior (2023)
-
Evaluating Neurodevelopmental Consequences of Perinatal Exposure to Antiretroviral Drugs: Current Challenges and New Approaches
Journal of Neuroimmune Pharmacology (2021)
-
Bidirectional Associations among Nicotine and Tobacco Smoke, NeuroHIV, and Antiretroviral Therapy
Journal of Neuroimmune Pharmacology (2020)
-
HIV Neuropathogenesis in the Presence of a Disrupted Dopamine System
Journal of Neuroimmune Pharmacology (2020)
-
Neurodevelopmental and behavioral consequences of perinatal exposure to the HIV drug efavirenz in a rodent model
Translational Psychiatry (2019)