Key Points
-
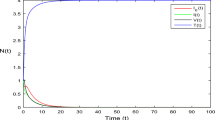
The early virological factors in HIV-1 infection, including transmission and the nature of the founder virus, can affect the time course of viraemia through the early peak to set point.
-
The identification of patients within the first few weeks of HIV-1 infection has provided early evidence of immune system damage, including massive apoptosis of CD4+ T cells, which is associated with the presence of apoptotic microparticles and TRAIL (tumour necrosis factor-related apoptosis-inducing ligand) in the blood, and damage to germinal centres in mucosal lymphoid tissues.
-
The first innate immune responses include the appearance of acute-phase proteins, early cytokine storm and activation of natural killer (NK) cells. An innate immune response to HIV-1 can be damaging, however, as it can draw susceptible T cells to the infection foci.
-
The first T cell response controls the founder virus by killing infected T cells. However, the T cell response also selects mutational changes in the founder virus, allowing immune evasion.
-
The first B cell response consists of early immune complexes, followed by non-neutralizing antibodies against the founder virus and then the slow development of broadly acting neutralizing antibodies. Development of vaccines that rapidly induce broadly acting neutralizing antibodies might be beneficial in preventing HIV infection.
-
Understanding the early events and immune responses is crucial to devising vaccine strategies that can improve the weak protection offered by current HIV vaccines that are being trialled, such as the RV144 (Thai) efficacy trial.
Abstract
The early immune response to HIV-1 infection is likely to be an important factor in determining the clinical course of disease. Recent data indicate that the HIV-1 quasispecies that arise following a mucosal infection are usually derived from a single transmitted virus. Moreover, the finding that the first effective immune responses drive the selection of virus escape mutations provides insight into the earliest immune responses against the transmitted virus and their contributions to the control of acute viraemia. Strong innate and adaptive immune responses occur subsequently but they are too late to eliminate the infection. In this Review, we discuss recent studies on the kinetics and quality of early immune responses to HIV-1 and their implications for developing a successful preventive HIV-1 vaccine.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Pilcher, C. D. et al. Detection of acute infections during HIV testing in North Carolina. N. Engl. J. Med. 352, 1873–1883 (2005).
Powers, K. A. et al. Improved detection of acute HIV-1 infection in sub-Saharan Africa: development of a risk score algorithm. AIDS 21, 2237–2242 (2007).
Hu, Q. et al. Blockade of attachment and fusion receptors inhibits HIV-1 infection of human cervical tissue. J. Exp. Med. 199, 1065–1075 (2004).
Veazey, R. S. et al. Protection of macaques from vaginal SHIV challenge by vaginally delivered inhibitors of virus-cell fusion. Nature 438, 99–102 (2005).
Margolis, L. & Shattock, R. Selective transmission of CCR5-utilizing HIV-1: the 'gatekeeper' problem resolved? Nature Rev. Microbiol. 4, 312–317 (2006).
Li, Q. et al. Visualizing antigen-specific and infected cells in situ predicts outcomes in early viral infection. Science 323, 1726–1729 (2009).
Miller, C. J. et al. Propagation and dissemination of infection after vaginal transmission of simian immunodeficiency virus. J. Virol. 79, 9217–9227 (2005).
Sodora, D. L., Gettie, A., Miller, C. J. & Marx, P. A. Vaginal transmission of SIV: assessing infectivity and hormonal influences in macaques inoculated with cell-free and cell-associated viral stocks. AIDS Res. Hum. Retroviruses 14, S119–S123 (1998).
Lai, S. K. et al. Human immunodeficiency virus type 1 is trapped by acidic but not by neutralized human cervicovaginal mucus. J. Virol. 83, 11196–11200 (2009).
Galvin, S. R. & Cohen, M. S. The role of sexually transmitted diseases in HIV transmission. Nature Rev. Microbiol. 2, 33–42 (2004).
Haaland, R. E. et al. Inflammatory genital infections mitigate a severe genetic bottleneck in heterosexual transmission of subtype A and C HIV-1. PLoS Pathog. 5, e1000274 (2009).
Keele, B. F. et al. Identification and characterization of transmitted and early founder virus envelopes in primary HIV-1 infection. Proc. Natl Acad. Sci. USA 105, 7552–7557 (2008). This study used single-genome amplification of viral RNA obtained from patients with acute HIV-1 infection to show that ∼80% of infections arise from a single transmitted or founder virus.
Abrahams, M. R. et al. Quantitating the multiplicity of infection with human immunodeficiency virus type 1 subtype C reveals a non-poisson distribution of transmitted variants. J. Virol. 83, 3556–3567 (2009).
Salazar-Gonzalez, J. F. et al. Genetic identity, biological phenotype, and evolutionary pathways of transmitted/founder viruses in acute and early HIV-1 infection. J. Exp. Med. 206, 1273–1289 (2009).
Keele, B. F. et al. Low-dose rectal inoculation of rhesus macaques by SIVsmE660 or SIVmac251 recapitulates human mucosal infection by HIV-1. J. Exp. Med. 206, 1117–1134 (2009).
Li, Q. et al. Glycerol monolaurate prevents mucosal SIV transmission. Nature 458, 1034–1038 (2009).
Bishop, K. N., Holmes, R. K., Sheehy, A. M. & Malim, M. H. APOBEC-mediated editing of viral RNA. Science 305, 645 (2004).
Geijtenbeek, T. B. et al. DC-SIGN, a dendritic cell-specific HIV-1-binding protein that enhances trans-infection of T cells. Cell 100, 587–597 (2000).
Moir, S. et al. B cells of HIV-1-infected patients bind virions through CD21–complement interactions and transmit infectious virus to activated T cells. J. Exp. Med. 192, 637–646 (2000).
Brenchley, J. M. et al. CD4+ T cell depletion during all stages of HIV disease occurs predominantly in the gastrointestinal tract. J. Exp. Med. 200, 749–759 (2004). In this study a combination of flow cytometry, endoscopy and histological techniques was used to show that the gastrointestinal tract is the site of the most profound depletion of CCR5+CD4+ T cells at all stages of HIV-1 disease.
Brenchley, J. M. et al. Microbial translocation is a cause of systemic immune activation in chronic HIV infection. Nature Med. 12, 1365–1371 (2006).
Brenchley, J. M. et al. Differential Th17 CD4 T-cell depletion in pathogenic and nonpathogenic lentiviral infections. Blood 112, 2826–2835 (2008).
Gasper-Smith, N. et al. Induction of plasma (TRAIL), TNFR-2, Fas ligand, and plasma microparticles after human immunodeficiency virus type 1 (HIV-1) transmission: implications for HIV-1 vaccine design. J. Virol. 82, 7700–7710 (2008).
Veazey, R. S. et al. Gastrointestinal tract as a major site of CD4+ T cell depletion and viral replication in SIV infection. Science 280, 427–431 (1998). The first demonstration that activated CD4+ T cells are depleted in the intestine within days of intravenous SIV infection of macaques, showing that the gastrointestinal tract is the major site of SIV replication.
Mattapallil, J. J. et al. Massive infection and loss of memory CD4+ T cells in multiple tissues during acute SIV infection. Nature 434, 1093–1097 (2005).
Levesque, M. C. et al. Polyclonal B cell differentiation and loss of gastrointestinal tract germinal centers in the earliest stages of HIV-1 infection. PLoS Med. 6, e1000107 (2009). This study used flow cytometry, histology and quantitative imaging techniques to show polyclonal B cell activation and destruction of germinal centres in acute HIV-1 infection.
Ho, D. D. et al. Rapid turnover of plasma virions and CD4 lymphocytes in HIV-1 infection. Nature 373, 123–126 (1995).
Schacker, T. W., Hughes, J. P., Shea, T., Coombs, R. W. & Corey, L. Biological and virologic characteristics of primary HIV infection. Ann. Intern. Med. 128, 613–620 (1998).
Rodriguez, B. et al. Predictive value of plasma HIV RNA level on rate of CD4 T-cell decline in untreated HIV infection. JAMA 296, 1498–1506 (2006).
Borrow, P., Lewicki, H., Hahn, B. H., Shaw, G. M. & Oldstone, M. B. Virus-specific CD8+ cytotoxic T-lymphocyte activity associated with control of viremia in primary human immunodeficiency virus type 1 infection. J. Virol. 68, 6103–6110 (1994).
Koup, R. A. et al. Temporal association of cellular immune responses with the initial control of viremia in primary human immunodeficiency virus type 1 syndrome. J. Virol. 68, 4650–4655 (1994).
Price, D. A. et al. Positive selection of HIV-1 cytotoxic T lymphocyte escape variants during primary infection. Proc. Natl Acad. Sci. USA 94, 1890–1895 (1997).
Wilson, J. D. et al. Direct visualization of HIV-1-specific cytotoxic T lymphocytes during primary infection. AIDS 14, 225–233 (2000).
Markowitz, M. et al. A novel antiviral intervention results in more accurate assessment of human immunodeficiency virus type 1 replication dynamics and T-cell decay in vivo. J. Virol. 77, 5037–5038 (2003).
Sedaghat, A. R., Siliciano, J. D., Brennan, T. P., Wilke, C. O. & Siliciano, R. F. Limits on replenishment of the resting CD4+ T cell reservoir for HIV in patients on HAART. PLoS Pathog. 3, e122 (2007).
Brennan, T. P. et al. Analysis of human immunodeficiency virus type 1 viremia and provirus in resting CD4+ T cells reveals a novel source of residual viremia in patients on antiretroviral therapy. J. Virol. 83, 8470–8481 (2009).
Dinoso, J. B. et al. Treatment intensification does not reduce residual HIV-1 viremia in patients on highly active antiretroviral therapy. Proc. Natl Acad. Sci. USA 106, 9403–9408 (2009). The stable reservoirs of latent HIV-1 infection were first identified in this study.
Finkel, T. H. et al. Apoptosis occurs predominantly in bystander cells and not in productively infected cells of HIV- and SIV-infected lymph nodes. Nature Med. 1, 129–134 (1995).
Silvestri, G. et al. Nonpathogenic SIV infection of sooty mangabeys is characterized by limited bystander immunopathology despite chronic high-level viremia. Immunity 18, 441–452 (2003). This study shows that SIV infected sooty mangabeys have high viral load but low immune activation with no loss of blood CD4+ T cells, suggesting chronic immune activation might be responsible for many of the problems in HIV-1 infection.
Liu, Z. et al. Elevated CD38 antigen expression on CD8+ T cells is a stronger marker for the risk of chronic HIV disease progression to AIDS and death in the Multicenter AIDS Cohort Study than CD4+ cell count, soluble immune activation markers, or combinations of HLA-DR and CD38 expression. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 16, 83–92 (1997).
Giorgi, J. V. et al. Predictive value of immunologic and virologic markers after long or short duration of HIV-1 infection. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 29, 346–355 (2002).
Deeks, S. G. et al. Immune activation set point during early HIV infection predicts subsequent CD4+ T-cell changes independent of viral load. Blood 104, 942–947 (2004). This paper shows that the level of immune activation is a better predictor of CD4+ T cell decline than viral load.
Li, Q. et al. Microarray analysis of lymphatic tissue reveals stage-specific, gene expression signatures in HIV-1 infection. J. Immunol. 183, 1975–1982 (2009).
Sodora, D. L. & Silvestri, G. Immune activation and AIDS pathogenesis. AIDS 22, 439–446 (2008).
Gao, F. et al. Origin of HIV-1 in the chimpanzee Pan troglodytes troglodytes. Nature 397, 436–441 (1999).
Korber, B. et al. Timing the ancestor of the HIV-1 pandemic strains. Science 288, 1789–1796 (2000).
Keele, B. F. et al. Chimpanzee reservoirs of pandemic and nonpandemic HIV-1. Science 313, 523–526 (2006).
Liu, R. et al. Homozygous defect in HIV-1 coreceptor accounts for resistance of some multiply-exposed individuals to HIV-1 infection. Cell 86, 367–377 (1996).
Carrington, M. & O'Brien, S. J. The influence of HLA genotype on AIDS. Annu. Rev. Med. 54, 535–551 (2003). A seminal review that describes the association between HLA-A, HLA-B and HLA-C alleles and the rate of disease progression.
Fellay, J. et al. A whole-genome association study of major determinants for host control of HIV-1. Science 317, 944–947 (2007).
Gao, X. et al. Effect of a single amino acid change in MHC class I molecules on the rate of progression to AIDS. N. Engl. J. Med. 344, 1668–1675 (2001).
Qi, Y. et al. KIR/HLA pleiotropism: protection against both HIV and opportunistic infections. PLoS Pathog. 2, e79 (2006).
Martin, M. P. et al. Epistatic interaction between KIR3DS1 and HLA-B delays the progression to AIDS. Nature Genet. 31, 429–434 (2002). The first report showing that NK cell receptors affect the progression to AIDS.
Martin, M. P. et al. Innate partnership of HLA-B and KIR3DL1 subtypes against HIV-1. Nature Genet. 39, 733–740 (2007).
Alter, G. et al. HLA class I subtype-dependent expansion of KIR3DS1+ and KIR3DL1+ NK cells during acute human immunodeficiency virus type 1 infection. J. Virol. 83, 6798–6805 (2009).
Alter, G. et al. Evolution of innate and adaptive effector cell functions during acute HIV-1 infection. J. Infect. Dis. 195, 1452–1460 (2007).
Tomaras, G. D. et al. Initial B-cell responses to transmitted human immunodeficiency virus type 1: virion-binding immunoglobulin M (IgM) and IgG antibodies followed by plasma anti-gp41 antibodies with ineffective control of initial viremia. J. Virol. 82, 12449–12463 (2008).
Stacey, A. R. et al. Induction of a striking systemic cytokine cascade prior to peak viremia in acute human immunodeficiency virus type 1 infection, in contrast to more modest and delayed responses in acute hepatitis B and C virus infections. J. Virol. 83, 3719–3733 (2009). In this article, the cytokine storm that follows HIV-1 infection was shown in a plasma donor cohort in which samples were available before and during the earliest stages of infection.
Raffatellu, M. et al. Simian immunodeficiency virus-induced mucosal interleukin-17 deficiency promotes Salmonella dissemination from the gut. Nature Med. 14, 421–428 (2008).
Nilsson, J. et al. Early immune activation in gut-associated and peripheral lymphoid tissue during acute HIV infection. AIDS 21, 565–574 (2007).
Lapenta, C. et al. Type I interferon is a powerful inhibitor of in vivo HIV-1 infection and preserves human CD4+ T cells from virus-induced depletion in SCID mice transplanted with human cells. Virology 263, 78–88 (1999).
de Jong, M. D. et al. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nature Med. 12, 1203–1207 (2006).
Cameron, M. J. et al. Interferon-mediated immunopathological events are associated with atypical innate and adaptive immune responses in patients with severe acute respiratory syndrome. J. Virol. 81, 8692–8706 (2007).
Killian, M. S., Fujimura, S. H., Hecht, F. M. & Levy, J. A. Similar changes in plasmacytoid dendritic cell and CD4 T-cell counts during primary HIV-1 infection and treatment. AIDS 20, 1247–1252 (2006).
Malleret, B. et al. Primary infection with simian immunodeficiency virus: plasmacytoid dendritic cell homing to lymph nodes, type I interferon, and immune suppression. Blood 112, 4598–4608 (2008).
Lore, K. et al. Accumulation of DC-SIGN+CD40+ dendritic cells with reduced CD80 and CD86 expression in lymphoid tissue during acute HIV-1 infection. AIDS 16, 683–692 (2002).
Beignon, A. S. et al. Endocytosis of HIV-1 activates plasmacytoid dendritic cells via Toll-like receptor-viral RNA interactions. J. Clin. Invest. 115, 3265–3275 (2005).
Granelli-Piperno, A., Golebiowska, A., Trumpfheller, C., Siegal, F. P. & Steinman, R. M. HIV-1-infected monocyte-derived dendritic cells do not undergo maturation but can elicit IL-10 production and T cell regulation. Proc. Natl Acad. Sci. USA 101, 7669–7674 (2004).
Boasso, A. et al. HIV inhibits CD4+ T-cell proliferation by inducing indoleamine 2, 3-dioxygenase in plasmacytoid dendritic cells. Blood 109, 3351–3359 (2007).
Manches, O. et al. HIV-activated human plasmacytoid DCs induce Tregs through an indoleamine 2, 3-dioxygenase-dependent mechanism. J. Clin. Invest. 118, 3431–3439 (2008).
Sabado, R. L. et al. In vitro priming recapitulates in vivo HIV-1 specific T cell responses, revealing rapid loss of virus reactive CD4+ T cells in acute HIV-1 infection. PLoS ONE. 4, e4256 (2009).
Borrow, P. & Bhardwaj, N. Innate immune responses in primary HIV-1 infection. Curr. Opin. HIV AIDS 3, 36–44 (2008).
Clay, C. C. et al. Neuroinvasion of fluorescein-positive monocytes in acute simian immunodeficiency virus infection. J. Virol. 81, 12040–12048 (2007).
Ward, J. et al. HIV modulates the expression of ligands important in triggering natural killer cell cytotoxic responses on infected primary T-cell blasts. Blood 110, 1207–1214 (2007).
Goonetilleke, N. et al. The first T cell response to transmitted/founder virus contributes to the control of acute viremia in HIV-1 infection. J. Exp. Med. 206, 1253–1272 (2009). This paper shows that the first HIV-1-specific CD8+ T cells make an important contribution to the control of viraemia in acute HIV-1 infection.
Cooper, M. A. et al. Cytokine-induced memory-like natural killer cells. Proc. Natl Acad. Sci. USA 106, 1915–1919 (2009).
Sun, J. C., Beilke, J. N. & Lanier, L. L. Adaptive immune features of natural killer cells. Nature 457, 557–561 (2009).
Cummins, J. E. Jr & Doncel, G. F. Biomarkers of cervicovaginal inflammation for the assessment of microbicide safety. Sex. Transm. Dis. 36, S84–S91 (2009).
Li, Q. et al. Peak SIV replication in resting memory CD4+ T cells depletes gut lamina propria CD4+ T cells. Nature 434, 1148–1152 (2005).
Mueller, Y. M. et al. IL-15 treatment during acute simian immunodeficiency virus (SIV) infection increases viral set point and accelerates disease progression despite the induction of stronger SIV-specific CD8+ T cell responses. J. Immunol. 180, 350–360 (2008).
Pantaleo, G. et al. Major expansion of CD8+ T cells with a predominant Vβ usage during the primary immune response to HIV. Nature 370, 463–467 (1994).
Fiebig, E. W. et al. Dynamics of HIV viremia and antibody seroconversion in plasma donors: implications for diagnosis and staging of primary HIV infection. AIDS 17, 1871–1879 (2003).
Bernardin, F., Kong, D., Peddada, L., Baxter-Lowe, L. A. & Delwart, E. Human immunodeficiency virus mutations during the first month of infection are preferentially found in known cytotoxic T-lymphocyte epitopes. J. Virol. 79, 11523–11528 (2005).
Draenert, R. et al. Immune selection for altered antigen processing leads to cytotoxic T lymphocyte escape in chronic HIV-1 infection. J. Exp. Med. 199, 905–915 (2004).
Jones, N. A. et al. Determinants of human immunodeficiency virus type 1 escape from the primary CD8+ cytotoxic T lymphocyte response. J. Exp. Med. 200, 1243–1256 (2004).
Tenzer, S. et al. Antigen processing influences HIV-specific cytotoxic T lymphocyte immunodominance. Nature Immunol. 10, 636–646 (2009).
Turnbull, E. L. et al. Kinetics of expansion of epitope-specific T cell responses during primary HIV-1 infection. J. Immunol. 182, 7131–7145 (2009).
Wang, Y. E. et al. Protective HLA class I alleles that restrict acute-phase CD8+ T-cell responses are associated with viral escape mutations located in highly conserved regions of human immunodeficiency virus type 1. J. Virol. 83, 1845–1855 (2009).
Streeck, H. et al. Human immunodeficiency virus type 1-specific CD8+ T-cell responses during primary infection are major determinants of the viral set point and loss of CD4+ T cells. J. Virol. 83, 7641–7648 (2009).
Goepfert, P. A. et al. Transmission of HIV-1 Gag immune escape mutations is associated with reduced viral load in linked recipients. J. Exp. Med. 205, 1009–1017 (2008).
Koup, R. A. Virus escape from CTL recognition. J. Exp. Med. 180, 779–782 (1994).
Borrow, P. et al. Antiviral pressure exerted by HIV-1-specific cytotoxic T lymphocytes (CTLs) during primary infection demonstrated by rapid selection of CTL escape virus. Nature Med. 3, 205–211 (1997).
O'Connor, D. H. et al. Acute phase cytotoxic T lymphocyte escape is a hallmark of simian immunodeficiency virus infection. Nature Med. 8, 493–499 (2002).
Leslie, A. J. et al. HIV evolution: CTL escape mutation and reversion after transmission. Nature Med. 10, 282–289 (2004). This report describes the reversion of virus sequence in the absence of HLA-specific selective immune pressure.
Allen, T. M. et al. Selective escape from CD8+ T-cell responses represents a major driving force of human immunodeficiency virus type 1 (HIV-1) sequence diversity and reveals constraints on HIV-1 evolution. J. Virol. 79, 13239–13249 (2005).
Fernandez, C. S. et al. Rapid viral escape at an immunodominant simian-human immunodeficiency virus cytotoxic T-lymphocyte epitope exacts a dramatic fitness cost. J. Virol. 79, 5721–5731 (2005).
Martinez-Picado, J. et al. Fitness cost of escape mutations in p24 Gag in association with control of human immunodeficiency virus type 1. J. Virol. 80, 3617–3623 (2006).
Schneidewind, A. et al. Escape from the dominant HLA-B27-restricted cytotoxic T-lymphocyte response in Gag is associated with a dramatic reduction in human immunodeficiency virus type 1 replication. J. Virol. 81, 12382–12393 (2007).
Brumme, Z. L. et al. Marked epitope- and allele-specific differences in rates of mutation in human immunodeficiency type 1 (HIV-1) Gag, Pol, and Nef cytotoxic T-lymphocyte epitopes in acute/early HIV-1 infection. J. Virol. 82, 9216–9227 (2008).
Asquith, B., Edwards, C. T., Lipsitch, M. & McLean, A. R. Inefficient cytotoxic T lymphocyte-mediated killing of HIV-1-infected cells in vivo. PLoS Biol. 4, e90 (2006). A mathematical model that describes the relationship between T cell killing, viral fitness and the rate of virus escape.
Crawford, H. et al. Compensatory mutation partially restores fitness and delays reversion of escape mutation within the immunodominant HLA-B*5703-restricted Gag epitope in chronic human immunodeficiency virus type 1 infection. J. Virol. 81, 8346–8351 (2007).
Addo, M. M. et al. Comprehensive epitope analysis of human immunodeficiency virus type 1 (HIV-1)-specific T-cell responses directed against the entire expressed HIV-1 genome demonstrate broadly directed responses, but no correlation to viral load. J. Virol. 77, 2081–2092 (2003).
Douek, D. C. et al. HIV preferentially infects HIV-specific CD4+ T cells. Nature 417, 95–98 (2002).
Pitcher, C. J. et al. HIV-1-specific CD4+ T cells are detectable in most individuals with active HIV-1 infection, but decline with prolonged viral suppression. Nature Med. 5, 518–525 (1999).
Kaufmann, D. E. et al. Comprehensive analysis of human immunodeficiency virus type 1-specific CD4 responses reveals marked immunodominance of gag and nef and the presence of broadly recognized peptides. J. Virol. 78, 4463–4477 (2004).
Oxenius, A. et al. Variable fate of virus-specific CD4+ T cells during primary HIV-1 infection. Eur. J. Immunol. 31, 3782–3788 (2001).
Gloster, S. E. et al. Association of strong virus-specific CD4 T cell responses with efficient natural control of primary HIV-1 infection. AIDS 18, 749–755 (2004).
Rosenberg, E. S. et al. Vigorous HIV-1-specific CD4+ T cell responses associated with control of viremia. Science 278, 1447–1450 (1997).
Oxenius, A. et al. Early highly active antiretroviral therapy for acute HIV-1 infection preserves immune function of CD8+ and CD4+ T lymphocytes. Proc. Natl Acad. Sci. USA 97, 3382–3387 (2000).
Sun, J. C., Williams, M. A. & Bevan, M. J. CD4+ T cells are required for the maintenance, not programming, of memory CD8+ T cells after acute infection. Nature Immunol. 5, 927–933 (2004).
Champagne, P. et al. Skewed maturation of memory HIV-specific CD8 T lymphocytes. Nature 410, 106–111 (2001).
Streeck, H., van Bockel, D. & Kelleher, A. T-cell responses in primary HIV-1 infection. Curr. Opin. HIV AIDS 3, 52–59 (2008).
Liu, J. et al. Immune control of an SIV challenge by a T-cell-based vaccine in rhesus monkeys. Nature 457, 87–91 (2009).
Dong, T. et al. HIV-specific cytotoxic T cells from long-term survivors select a unique T cell receptor. J. Exp. Med. 200, 1547–1557 (2004).
Turnbull, E. L. et al. HIV-1 epitope-specific CD8+ T cell responses strongly associated with delayed disease progression cross-recognize epitope variants efficiently. J. Immunol. 176, 6130–6146 (2006).
Wei, X. et al. Antibody neutralization and escape by HIV-1. Nature 422, 307–312 (2003). The timing of the first antibody-selected escape mutations of HIV-1 in acute infection highlights the role of the glycan shield.
Richman, D. D., Wrin, T., Little, S. J. & Petropoulos, C. J. Rapid evolution of the neutralizing antibody response to HIV type 1 infection. Proc. Natl Acad. Sci. USA 100, 4144–4149 (2003). This study shows that neutralizing antibodies account for the extensive variation in the HIV-1 Env proteins observed in the early months of primary infection.
Gray, E. S. et al. Neutralizing antibody responses in acute human immunodeficiency virus type 1 subtype C infection. J. Virol. 81, 6187–6196 (2007).
Stamatatos, L., Morris, L., Burton, D. R. & Mascola, J. R. Neutralizing antibodies generated during natural HIV-1 infection: good news for an HIV-1 vaccine? Nature Med. 15, 866–870 (2009).
Gray, E. S. et al. Broad neutralization of human immunodeficiency virus type 1 mediated by plasma antibodies against the gp41 membrane proximal external region. J. Virol. 83, 11265–11274 (2009).
Derdeyn, C. A. et al. Envelope-constrained neutralization-sensitive HIV-1 after heterosexual transmission. Science 303, 2019–2022 (2004).
Alam, S. M. et al. The role of antibody polyspecificity and lipid reactivity in binding of broadly neutralizing anti-HIV-1 envelope human monoclonal antibodies 2F5 and 4E10 to glycoprotein 41 membrane proximal envelope epitopes. J. Immunol. 178, 4424–4435 (2007).
Alam, S. M. et al. Human immunodeficiency virus type 1 gp41 antibodies that mask membrane proximal region epitopes: antibody binding kinetics, induction, and potential for regulation in acute infection. J. Virol. 82, 115–125 (2008).
Crooks, E. T. et al. A comparative immunogenicity study of HIV-1 virus-like particles bearing various forms of envelope proteins, particles bearing no envelope and soluble monomeric gp120. Virology 366, 245–262 (2007).
Tobin, G. J. et al. Deceptive imprinting and immune refocusing in vaccine design. Vaccine 26, 6189–6199 (2008).
Forthal, D. N., Landucci, G. & Daar, E. S. Antibody from patients with acute human immunodeficiency virus (HIV) infection inhibits primary strains of HIV type 1 in the presence of natural-killer effector cells. J. Virol. 75, 6953–6961 (2001).
Aasa-Chapman, M. M. et al. Detection of antibody-dependent complement-mediated inactivation of both autologous and heterologous virus in primary human immunodeficiency virus type 1 infection. J. Virol. 79, 2823–2830 (2005).
Burrer, R., Haessig-Einius, S., Aubertin, A. M. & Moog, C. Neutralizing as well as non-neutralizing polyclonal immunoglobulin (Ig)G from infected patients capture HIV-1 via antibodies directed against the principal immunodominant domain of gp41. Virology 333, 102–113 (2005).
Moore, P. L. et al. The c3-v4 region is a major target of autologous neutralizing antibodies in human immunodeficiency virus type 1 subtype C infection. J. Virol. 82, 1860–1869 (2008).
Calarese, D. A. et al. Antibody domain exchange is an immunological solution to carbohydrate cluster recognition. Science 300, 2065–2071 (2003).
Kwong, P. D. et al. HIV-1 evades antibody-mediated neutralization through conformational masking of receptor-binding sites. Nature 420, 678–682 (2002). This report shows that conformational masking enables HIV-1 to maintain receptor binding and simultaneously resist antibody-mediated neutralization.
Ofek, G. et al. Structure and mechanistic analysis of the anti-human immunodeficiency virus type 1 antibody 2F5 in complex with its gp41 epitope. J. Virol. 78, 10724–10737 (2004).
Cardoso, R. M. et al. Structural basis of enhanced binding of extended and helically constrained peptide epitopes of the broadly neutralizing HIV-1 antibody 4E10. J. Mol. Biol. 365, 1533–1544 (2007).
Nelson, J. D. et al. An affinity-enhanced neutralizing antibody against the membrane-proximal external region of human immunodeficiency virus type 1 gp41 recognizes an epitope between those of 2F5 and 4E10. J. Virol. 81, 4033–4043 (2007).
Shen, X. et al. In vivo gp41 antibodies targeting the 2F5 monoclonal antibody epitope mediate human immunodeficiency virus type 1 neutralization breadth. J. Virol. 83, 3617–3625 (2009).
Haynes, B. F., Moody, M. A., Verkoczy, L., Kelsoe, G. & Alam, S. M. Antibody polyspecificity and neutralization of HIV-1: a hypothesis. Hum. Antibodies 14, 59–67 (2005).
Fox, C. H. et al. Lymphoid germinal centers are reservoirs of human immunodeficiency virus type 1 RNA. J. Infect. Dis. 164, 1051–1057 (1991).
Pantaleo, G. et al. Lymphoid organs function as major reservoirs for human immunodeficiency virus. Proc. Natl Acad. Sci. USA 88, 9838–9842 (1991).
Muro-Cacho, C. A., Pantaleo, G. & Fauci, A. S. Analysis of apoptosis in lymph nodes of HIV-infected persons. Intensity of apoptosis correlates with the general state of activation of the lymphoid tissue and not with stage of disease or viral burden. J. Immunol. 154, 5555–5566 (1995).
Zhang, Z. Q. et al. Early depletion of proliferating B cells of germinal center in rapidly progressive simian immunodeficiency virus infection. Virology 361, 455–464 (2007).
Mascola, J. R. et al. Protection of macaques against vaginal transmission of a pathogenic HIV-1/SIV chimeric virus by passive infusion of neutralizing antibodies. Nature Med. 6, 207–210 (2000). An important study that showed that neutralizing antibodies can protect against mucosal transmission, thus providing a rationale for vaccine strategies aimed at eliciting these antibodies.
Hessell, A. J. et al. Fc receptor but not complement binding is important in antibody protection against HIV. Nature 449, 101–104 (2007).
Hessell, A. J. et al. Effective, low-titer antibody protection against low-dose repeated mucosal SHIV challenge in macaques. Nature Med. 15, 951–954 (2009). An elegant study addressing the level of antibody needed at mucosal sites for protection, which can inform experimental vaccine evaluation on the protocol needed for sufficient elicitation of antibodies.
Hessell, A. J. et al. Broadly neutralizing human anti-HIV antibody 2G12 is effective in protection against mucosal SHIV challenge even at low serum neutralizing titers. PLoS Pathog. 5, e1000433 (2009).
Engram, J. C. et al. Vaccine-induced, simian immunodeficiency virus-specific CD8+ T cells reduce virus replication but do not protect from simian immunodeficiency virus disease progression. J. Immunol. 183, 706–717 (2009).
Rerks-Ngarm, S. et al. Vaccination with ALVAC and AIDSVAX to prevent HIV-1 infection in Thailand. N. Engl. J. Med. 20 Oct 2009 (doi:10.1056/NEJMoa0908492).
Reynolds, M. R. et al. Macaques vaccinated with live-attenuated SIV control replication of heterologous virus. J. Exp. Med. 205, 2537–2550 (2008).
Althaus, C. L. & De Boer, R. J. Dynamics of immune escape during HIV/SIV infection. PLoS Comput. Biol. 4, e1000103 (2008).
Lee, J. K. et al. T cell cross-reactivity and conformational changes during TCR engagement. J. Exp. Med. 200, 1455–1466 (2004).
Santra, S. et al. A centralized gene-based HIV-1 vaccine elicits broad cross-clade cellular immune responses in rhesus monkeys. Proc. Natl Acad. Sci. USA 105, 10489–10494 (2008).
Barouch, D. & Korber, B. HIV-1 mosaic antigens expand cellular immune breadth and depth in rhesus monkeys. Abstr. S06-04 AIDS vaccine conference 2009, Paris (2009)
Korber, B., Gnankaran, S. & Perkins, S. New applications for mosaic antigen designs. Abstr. S06-03 AIDS vaccine conference 2009, Paris (2009)
Pitisuttithum, P. et al. Randomized, double-blind, placebo-controlled efficacy trial of a bivalent recombinant glycoprotein 120 HIV-1 vaccine among injection drug users in Bangkok, Thailand. J. Infect. Dis. 194, 1661–1671 (2006).
McElrath, M. J. et al. HIV-1 vaccine-induced immunity in the test-of-concept Step Study: a case-cohort analysis. Lancet 372, 1894–1905 (2008).
Buchbinder, S. P. et al. Efficacy assessment of a cell-mediated immunity HIV-1 vaccine (the Step Study): a double-blind, randomised, placebo-controlled, test-of-concept trial. Lancet 372, 1881–1893 (2008).
Casimiro, D. R. et al. Attenuation of simian immunodeficiency virus SIVmac239 infection by prophylactic immunization with dna and recombinant adenoviral vaccine vectors expressing Gag. J. Virol. 79, 15547–15555 (2005).
Hansen, S. G. et al. Effector memory T cell responses are associated with protection of rhesus monkeys from mucosal simian immunodeficiency virus challenge. Nature Med. 15, 293–299 (2009).
Walker, B. D. & Burton, D. R. Toward an AIDS vaccine. Science 320, 760–764 (2008).
Baker, B. M., Block, B. L., Rothchild, A. C. & Walker, B. D. Elite control of HIV infection: implications for vaccine design. Expert Opin. Biol. Ther. 9, 55–69 (2009).
Wong, S. B. J. & Siliciano, R. F. in AIDS Vaccine Development: Challenges and Opportunities (eds. Koff, W. C., Kahn, P. & Gust, I. D.) 17–22 (Caister Academic, UK, 2007).
Acknowledgements
This work was supported by the Center for HIV/AIDS Vaccine Immunology (CHAVI) grant A1067854-03. Additional support came from the Medical Research Human Immunology Unit, the National Institute for Health Research, Oxford Biomedical Research Centre and grants 38643 and 37874 from the Bill and Melinda Gates Foundation. A.J.M. and P.B. are Jenner Investigators and P.B. is supported by a Jenner Fellowship. G.D.T is supported by the US National Institutes of Health, grants RO1AI052779, U19AI067854, AI068618 and AI64518 and the Bill and Melinda Gates Foundation (grant 38619). We are grateful to members of the CHAVI Scientific Leadership Group, N. Letvin, M. Cohen, J. Sodroski, D. Goldstein and G. Shaw for scientific input and for reviewing this manuscript, and to the CHAVI Clinical Core Investigators and their patients for participation in the CHAVI studies cited in this review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Related links
Glossary
- Viral set point
-
The time at which plasma viraemia settles to a stable level (within approximately 3–6 months from the onset of HIV infection). Viral set point is partially predictive of both how quickly HIV infection will progress and the risk of HIV transmission.
- Founder virus
-
A transmitted virus or a virus that gives rise to all virus quasispecies in an infected individual.
- Viral fitness
-
The ability of a virus to replicate in a given environment. By definition in in vitro studies, a drug-resistant virus has greater ability to replicate than wild-type virus when measured in the presence of a drug, similarly a T cell escape mutant will replicate better than wild-type virus when co-cultured with specific T cells. The T cell-resistant or drug-resistant virus may replicate less well than the wild type when the selective force is withdrawn.
- Langerhans cell
-
A type of dendritic cell that is resident in the epithelial layer of the skin and mucosa.
- Single-genome amplification
-
A method of DNA sequencing that uses high-fidelity polymerase and minimizes PCR amplification, thereby excluding sequence errors and recombination events that may be introduced during amplification.
- Clade
-
HIV is subdivided, based on degree of sequence divergence, into three major groups, M, N and O; group M is subdivided into 10 subtypes or clades, of which clade C is the predominant subtype worldwide (prevalent in subSaharan Africa and India) and clade B is the most studied subtype (prevalent in North America and Eastern Europe).
- Quasispecies
-
A distribution of non-identical but closely related viral genomes. The entire distribution forms an organized cooperative structure, which acts like (quasi) a single unit (species).
- APOBEC cytidine deaminases
-
A family of host antiviral proteins that introduce multiple mutations, including stop codons, in retroviruses by deaminating cytosine residues in nascent retroviral cDNA.
- Germinal centre
-
A highly specialized and dynamic microenvironment located in peripheral lymphoid tissues (for example, the spleen or lymph nodes). It is the main site of B cell maturation, leading to the generation of memory B cells and plasma cells that produce high-affinity antibody.
- Regulatory T (TReg) cell
-
A type of CD4+ T cell that is characterized by its expression of forkhead box P3 (FOXP3) and high levels of CD25. TReg cells can suppress many types of immune responses.
- Genome-wide association study
-
An approach that involves rapidly scanning single nucleotide polymorphism markers across the complete genomes of many individuals to find genetic variations associated with a particular disease.
- Single nucleotide polymorphisms
-
(SNPs). Single nucleotide variations in genomic DNA sequences in which one of the four nucleotides is substituted for another. SNPs are the most frequent type of polymorphism in the genome and can be used to map genes connected by linkage disequilibrium.
- Bw4 motif
-
The amino acid sequences at positions 77–83 in the α1 domain of HLA class I heavy chains. There are four Bw4 motif sequences, which differ only at positions 77 (Asn, Asp or Ser) and 80 (Ile or Thr). The Bw4 motif is involved in the recognition of certain HLA alleles by killer immunoglobulin-like receptors.
- Seroconversion
-
Development of a detectable concentration of pathogen-specific antibodies in the serum as a result of infection or immunization. Seroconversion normally occurs in patients with HIV-1 infection 3–4 weeks following infection, around Fiebig stage III, typically when plasma virus loads are reaching their peak.
- Acute-phase proteins
-
A group of proteins, including C-reactive protein, serum amyloid A, complement components and fibrinogen, that are secreted into the blood in increased or decreased quantities by hepatocytes in response to trauma, inflammation or disease. These proteins can be inhibitors or mediators of inflammatory processes.
- T helper 17 cells
-
A subset of CD4+ T helper cells that produce interleukin-17 (IL-17) and that are thought to be important in antibacterial and antifungal immunity and may also have a role in autoimmune diseases. Their generation involves IL-23 and IL-21, as well as the transcription factors RORγt (retinoic acid-related orphan receptor-γt) and STAT3 (signal transducer and activator of transcription 3).
- Envelope proteins
-
Envelope proteins of HIV are initially produced as a precursor glycoprotein of 160 kDa (gp160) that is cleaved to generate gp120 and gp41. Three gp120 molecules and three gp41 molecules are thought to combine in a trimer to form the envelope spike.
- Fiebig stages
-
Stages of HIV-1 infection. They are defined by a series of laboratory tests that measure the emergence of HIV-1-specific antibodies, viral RNA and viral antigens.
- Class switching
-
The somatic-recombination process by which the class of immunoglobulin is switched from IgM to IgG, IgA or IgE.
- Peyer's patches
-
Specialized lymphoid follicles localized in the submucosa of the small intestine and appendix.
- Antibody-dependent cell-mediated cytotoxicity
-
(ADCC). A cytotoxic mechanism by which an antibody-coated target cell is directly killed by a leukocyte that expresses FcRs, such as an NK cell, macrophage or neutrophil.
Rights and permissions
About this article
Cite this article
McMichael, A., Borrow, P., Tomaras, G. et al. The immune response during acute HIV-1 infection: clues for vaccine development. Nat Rev Immunol 10, 11–23 (2010). https://doi.org/10.1038/nri2674
Published:
Issue date:
DOI: https://doi.org/10.1038/nri2674
This article is cited by
-
Strategies for HIV-1 vaccines that induce broadly neutralizing antibodies
Nature Reviews Immunology (2023)
-
MicroRNA let-7 and viral infections: focus on mechanisms of action
Cellular & Molecular Biology Letters (2022)
-
Deep sequencing of the HIV-1 polymerase gene for characterisation of cytotoxic T-lymphocyte epitopes during early and chronic disease stages
Virology Journal (2022)
-
A longitudinal analysis of immune escapes from HLA-B*13-restricted T-cell responses at early stage of CRF01_AE subtype HIV-1 infection and implications for vaccine design
BMC Immunology (2022)
-
Characteristics of recent HIV infection among individuals newly diagnosed as HIV-positive in South Korea (2008–2015)
Scientific Reports (2022)