Abstract
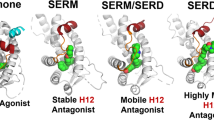
As the current management of BPH/lower urinary tract symptoms by traditionally involved pharmacological agents such as 5alpha-reductase inhibitors and α1-adrenoceptor antagonists is suboptimal, there is definite need of new therapeutic strategies. There is ample evidence in literature that suggests the role of estrogens in BPH development and management through the different tissue and cell-specific receptors. This article reviews the beneficial actions of selective estrogen receptor modulator (SERM) and ERβ-selective ligands, which have been demonstrated through in vitro studies using human prostate cell lines and in vivo animal studies. SERMs have anti-proliferative, anti-inflammatory and pro-apoptotic mechanisms in BPH, and also act by inhibiting various growth factors, and thus represent a unique and novel approach in BPH management directed at estrogen receptors or estrogen metabolism.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Tang J, Yang J . Etiopathogenesis of benign prostatic hyperplasia. IJU 2009; 25: 312–331.
Roehrborn CG . Male lower urinary tract symptoms (LUTS) and benign prostatic hyperplasia (BPH). Medical Clin N Am 2011; 95: 87–100.
Kumar R, Verma V, Sarswat A, Maikhuri JP, Dalela D, Gupta G et al. Selective estrogen receptor modulators regulate stromal proliferation in human benign prostatic hyperplasia by multiple beneficial mechanisms-action of two new agents. Invest New Drugs 2010; 30: 582–593.
Gray A, Feldman HA, McKinlay JB, Longcope C . Age, disease, and changing sex hormone levels in middle-aged men: results of the Massachusetts Male Aging Study. J Clin Endocrinol Metabol 1991; 73: 1016–1025.
Harman SM, Metter EJ, Tobin JD, Pearson J, Blackman MR . Longitudinal effects of aging on serum total and free testosterone levels in healthy men. Baltimore Longitudinal Study of Aging. J Clin Endocrinol Metabol 2001; 86: 724–731.
Vermeulen A, Kaufman JM, Goemaere S, van Pottelberg I . Estradiol in elderly men. Aging Male 2002; 5: 98–102.
Vermeulen A . Testicular hormonal secretion and aging in males. In: Grayhack JT, Wilson JD, Scherbenske MJ (eds) Benign Prostatic Hyperplasia. Proceedings of Workshop Sponsored by the Kindney Disease and Urology Program of the NIAMDD, 20–21 February, 1975. US Government Printing office: Washington, DC, USA, 1976; pp 77–182.
Stone NN, Fair WR, Fishman J . Estrogen formation in human prostatic tissue from patients with and without benign prostatic hyperplasia. Prostate 1986; 9: 311–318.
Krieg M, Nass R, Tunn S . Effect of aging on endogenous level of 5a-hihydrotestosterone, testosterone, estradiol and estrone in epithelium and stroma of normal and hyperplastic human prostate. J Clin Endocrinol Metab 1993; 77: 361–375.
Walsh PC, Wilson JD . The induction of prostatic hypertrophy in the dog with androstenediol. J Clin Invest 1976; 57: 1093–1097.
Collins AT, Zhiming B, Gilmore K, Neal DE . Androgen and oestrogen responsiveness of stromal cells derived from the human hyperplastic prostate: oestrogen regulation of the androgen receptor. J Endocrinol 1994; 143: 269–277.
Deklerk DP, Coffey DS, Ewing LL, McDermott IR, Reiner WG, Robinson CH et al. Comparison of spontaneous and experimentally induced canine prostatic hyperplasia. J Clin Invest 1979; 64: 842–849.
Clement KM, Nanda J, Chapman KE, Habib FK . Oestrogen and benign prostatic hyperplasia: effects on stromal cell proliferation and local formation from androgen. J Endocrinol 2008; 197: 483–491.
Shapiro E, Steiner MS . Role of growth factors in prostatic development. In: Kirby R (ed) Textbook of Benign Prostatic Hyperplasia. ISIS Medical Media: Oxford, UK, 1996; pp 17–19.
Brolin J, Skoog L, Ekman P . Immunohistochemistry and biochemistry in detection of androgen, progesterone and estrogen receptors in benign and malignant human prostatic tissue. Prostate 1992; 20: 281–295.
Horwitz KB, Jackson TA, Bain DL, Richer JK, Takimoto GS, Tung I . Nuclear receptor coactivators and corepressors. Mol Endocrinol 1996; 10: 1167–1177.
Helguero LA, Faulds MH, Gustafsson JA, Haldosen LA . Estrogen receptors alpha (ERα) and beta (ERβ) differentially regulate proliferation and apoptosis of the normal murine mammary epithelial cell line HC11. Oncogene 2005; 24: 6605–6616.
Murphy LC, Peng B, Lewis A, Davie JR, Leygue E, Kemp A et al. Inducible upregulation of oestrogen receptor-β1 affects oestrogen and tamoxifen responsiveness in MCF7 human breast cancer cells. J Mol Endocrinol 2005; 34: 553–566.
Treeck O, Lattrich C, Springwald A, Ortmann O . Estrogen receptor beta exerts growth-inhibitory effects on human mammary epithelial cells. Breast Cancer Res Treat 2010; 120: 557–565.
Hodges-Gallagher L, Valentine C, Bader S, Kushner P . Estrogen receptor beta increases the efficacy of antiestrogens by effects on apoptosis and cell cycling in breast cancer cells. Breast Cancer Res Treat 2008; 109: 241–250.
Paruthiyil S, Parmar H, Kerekatte V, Cunha GR, Firestone GL, Leitman DC . Estrogen receptor β inhibits human breast cancer cell proliferation and tumor formation by causing a G2 cell cycle arrest. Cancer Res 2004; 64: 423–428.
Ström A, Hartman J, Foster JS, Kietz S, Wimalasena J, Gustafsson JA . Estrogen receptor β inhibits 17β-estradiol-stimulated proliferation of the breast cancer cell line T47D. Proc Natl Acad Sci USA 2004; 101: 1566–1571.
Hartman J, Lindberg K, Morani A, Inzunza J, Strom A, Gustafsson JA . Estrogen receptor beta inhibits angiogenesis and growth of T47D breast cancer xenografts. Cancer Res 2006; 66: 11207–11213.
Weryha G, Pascal-Vigneron V, Klein M, Leclère J . Selective estrogen receptor modulators. Curr Opin Rheumatol 1999; 11: 301–306.
Weihua Z, Lathe R, Warner M, Gustaffson JA . An endocrine pathway in the prostate.ERbeta.AR, 5 alpha androstane 3 beta, 17 beta-diol and CYP7BI, regulates prostate growth. Proc Natl Acad Sci USA 2002; 99: 13589–13594.
Mc person SJ, Ellem SJ, Simpson ER, Pachev V, Risbridger GP . Essential role for estrogen receptor beta in stromal- epithial regualation of prostatic hyperplasia. Encrinology 2007; 148: 566–574.
Mc person SJ, Ellem SJ, Risbridger GP . Estrogen regulated development and differentiation of prostate. Differentiation 2008; 76: 660–670.
Minutolo F, Macchia M, Katzenellenbogen BS, Katzenellenbogen JA . Estrogen receptor beta ligands: recent advances and biomedical applications. Med Res Rev 2011; 31: 364–442.
Cassidy A . Potential risks and benefits of phytoestrogen-rich diets. Int J Vitam Nutr Res 2003; 73: 120–126.
Prins GS, Korach KS . The role of estrogens and estrogen receptors in normal prostate growth and disease. Steroids 2008; 73: 233–244.
Jarred RA, Keikha M, Dowling C, McPherson SJ, Clare AM, Husband AJ et al. Induction of apoptosis in low grade human prostate carcinoma by red clover-derived dietary isoflavones. Cancer Epidemiol Biomarkers Prev 2002; 11: 1689–1696.
Morton M, Turkes A, Denis L, Griffith K . Can dietary factors influence prostatic disease? BJU Int 1999; 84: 594–554.
Severson RK, Nomura AM, Grove JS, Stemmermann GN . A prospective study of demographics, diet, and prostate cancer among men of Japanese ancestry in Hawaii. Cancer Res 1989; 49: 1857–1860.
Adlercreutz H, Honjo H, Higashi A, Fotsis T, Hämäläinen E, Hasegawa T et al. Urinary excretion of lignans and isoflavonoid phytoestrogens in Japanese men and women consuming a traditional Japanese diet. Am J Clin Nutr 1991; 54: 1093–1100.
Jong FH, Oishi K, Hayes RB, Bogdanowicz JF, Raatgever JW, van der Maas PJ et al. Peripheral hormone levels in controls and patients with prostatic cancer or benign prostatic hyperplasia: results from the Dutch-Japanese case-control study. Cancer Res 1991; 51: 3445–3450.
Kuiper GG, Carlsson B, Grandien K, Enmark E, Haggblad J, Nilsson S et al. Comparison of the ligand binding specificity and transcript tissue distribution of estrogen receptors alpha and beta. Endocrinology 1997; 138: 863–870.
Mersereau JE, Levy N, Staub RE, Baggett S, Zogric T, Chow S et al. Liquiritigenin is a plant-derived highly selective estrogen receptor beta agonist. Mol Cell Endocrinol 2008; 283: 49–57.
Paruthiyil S, Cvoro A, Zhao X, Wu Z, Sui Y, Staub RE et al. Drug and cell type-specific regulation of genes with different classes of estrogen receptor β-selective agonists. PLoS ONE 2009; 4: e6271.
Yang R, Ma YX, Chen LF, Zhou Y, Yang ZP, Zhu Y et al. Antagonism of estrogen-mediated cell proliferation by raloxifene in prevention of ageing-related prostatic hyperplasia. Asian J Androl 2010; 12: 735–743.
Eaton CL . Aetiology and pathogenesis of benign prostatic hyperplasia. Curr Opin Urol 2003; 13: 7–10.
Soulitzis N, Karyotis I, Delakas D, Spandidos DA . Expression analysis of peptide growth factors VEGF, FGF2, TGFBT, EGF, and IGF1 in prostate cancer and BPH. Int J Oncol 2006; 29: 305–314.
Rana S, Sen R, Kalra R, Arora B, Sharma P, Gahlawat S . Immunhistochemical study of the expression of epidermal growth factor receptor in BPH, prostatic intraepithilial neoplasia and prostatic carcinoma. Indian J Pathol Microbiol 2006; 49: 495–499.
Li Z, Habuchi T, Tsuchiya N, Mitsumori K, Wang L, Ohyama C . Increased risk of prostate cancer and benign prostatic hyperplasia associated with transforming growth factor-beta 1 gene polymorphism at codon 10. Carcinogenesis 2004; 25: 237–240.
Lee KL, Peehl DM . Molecular and cellular pathogenesis of benign prostatic hyperplasia. J Urol 2004; 172: 1784–1791.
Kramer G, Marberger M . Could inflammation be a key component in the progression of benign prostatic hyperplasia? Curr Opin Urol 2006; 16: 25–29.
Kohnen PW, Drach GW . Patterns of inflammation in prostatic hyperplasia: a histologic and bacterial study. J Urol 1979; 121: 755–760.
Theyer G, Kramer G, Assmann I, Sherwood E, Preinfalk W, Marberger M et al. Phenotypic characterization of infiltrating leukocytes in benign prostatic hyperplasia. Lab Invest 1992; 66: 96–107.
Steiner G, Gessl A, Kramer G, Schollhammer A, Forster O, Marberger M . Phenotype and function of peripheral and prostatic lymphocytes in patients with benign prostatic hyperplasia. J Urol 1994; 151: 480–484.
Kramer G, Steiner GE, Handisurya A, Stix U, Haitel A, Knerer B et al. Increased expression of lymphocyte-derived cytokines in benign hyperplastic prostate tissue, identification of the producing cell types and effect of differentially expressed cytokines on stromal cell proliferation. Prostate 2002; 52: 43–48.
Yatkin E, Bernoulli J, Lammintausta R, Santti R . Fispemifene [Z-2-{2-[4-(4-chloro-1,2-diphenylbut-1-enyl)-phenoxy]ethoxy}-ethanol], a novel selective estrogen receptor modulator, attenuates glandular inflammation in an animal model of chronic nonbacterial prostatitis. J Pharmacol Exp Ther 2008; 327: 58–67.
Sharma OP, Adlercreutz H, Strandberg JD, Zirkin BR, Coffey DS, Ewing LL . Soy of dietary source plays a preventive role against the pathogenesis of prostatitis in rats. J Steroid Biochem 1992; 43: 557–564.
Masumori N, Tsukamoto T, Kumamoto Y, Miyake H, Rhodes T, Girman GJ et al. Japanese men have smaller prostate volume but comparable urinary flow rates relative to American men: results of community based studies in 2 countries. J Urol 1996; 155: 1324–1327.
Fujikawa S, Matsuura H, Kanai M, Fumino M, Ishii K, Arima K et al. Natural history of human prostate gland: morphometric and histopathological analysis of Japanese men. Prostate 2006; 65: 355–364.
McPherson S, Hussaina S, Balanathana P, Hedwardsa S, Niranjana B, Granta M et al. Estrogen receptor–β activated apoptosis in benign hyperplasia and cancer of the prostate is androgen independent and TNFα mediated. PNAS 2010; 107: 3123–3128.
Glienke W, Dolgova Y, Müller I, Grösch S, Binder J, Geisslinger G et al. Induction of apoptosis in human prostate stromal cells by 4-hydroxytamoxifen: an alternative therapy for benign prostate hyperplasia. World J Urol 2004; 22: 452–456.
Hayward SW, Rosen MA, Cunha GR . Stromal-epithelial interactions in the normal and neoplastic prostate. Br J Urol 1997; 79: 18–26.
Rijken AM, Hu J, Perlman EJ, Morsberger LA, Long P, Kern SE et al. Genomic alterations in distal bile duct carcinoma by comparative genomic hybridization and karyotype analysis. Genes Chromosomes Cancer 1999; 26: 185–191.
Norman BH, Dodge JA, Richardson TI, Borromeo PS, Lugar CW, Jones SA et al. Benzopyrans are selective estrogen receptor β agonists with novel activity in models of benign prostatic hyperplasia. J Med Chem 2006; 49: 6155–6157.
Wilson D . The pathogenesis of bellign prostatic hyperplasia. Am Med 1980; 68: 745.
McNeal E . Origin and evolution of benign prostatic enlargement. Invest. Urol 1978; 5: 340.
Lawson RK . Etiology of benign prostatic hyperplasia. In Lepoy, Hand Lawson, RK (eds) Prostatic diseases. W:B. Sallnders: Philadelphia, PA, USA., Ch. 7 1993; pp 89–95.
Isaac JT, Coffey DS . Etiology and disease process of benign prostatic hypelplasia. Prostate Suppl 1989; 2: 33.
Hu WY, Shi GB, Lam HM, Hu DP, Ho SM, Madueke IC et al. Estrogen-initiated transformation of prostate epithelium derived from normal human prostate stem-progenitor cells. Endocrinology 2011; 152: 2150–2163.
Ho CK, Habib FK . Estrogen and androgen signaling in the pathogenesis of BPH. Nat Rev Urol 2011; 8: 29–41.
Risbridger GP, Frydenberg M, Hayward SW, Clark PE, Appu S . Endocrinology of the prostate. In Groot LJD (ed), 6th edn 2010.
Ellem SJ, Risbridger GP . Treating prostate cancer: a rationale for targeting local oestrogens. Nat Rev Cancer 2007; 7: 621–627.
Shanle ER, Xu W . Selectively targeting estrogen receptors for cancer treatment. Adv Drug Deliv Rev 2010; 62: 1265–1276.
Matthews J, Gustafsson JA . Estrogen signaling: a subtle balance between ER alpha and ER beta. Mol Interv 2003; 3: 281–292.
Wang Z, Zhang X, Shen P, Loggie BW, Chang Y, Deuel TF . A variant of estrogen receptor-, hER- 36: transduction of estrogen- and antiestrogen-dependent membrane-initiated mitogenic signaling. Proc Natl Acad Sci USA 2006; 103: 9063–9068.
Levin ER . Cell localization, physiology, and nongenomic actions of estrogen receptors. J Appl Physiol 2001; 91: 1860–1867.
Bjornstrom L, Sjoberg M . Mechanisms of estrogen receptor signaling: convergence of genomic and nongenomic actions on target genes. Mol Endocrinol 2005; 19: 833–842.
Kuiper GG, Enmark E, Pelto-Huikko M, Nilsson S, Gustafsson JA . Cloning of a novel receptor expressed in rat prostate and ovary. Proc Natl Acad Sci USA 1996; 93: 5925–5930.
Mewshaw RE, Edsall RJ, Yang C, Manas ES . ERβ ligands. 3. Exploiting two binding orientations of the 2-phenylnaphthalene scaffold to achieve ERβ selectivity. J Med Chem 2005; 48: 3953–3979.
Neubauer BL, McNulty AM, Chedid M, Chen K, Goode RL, Johnson MA et al. The selective estrogen receptor modulator trioxifene (LY133314) inhibits metastasis and extends survival in the PAIII rat prostatic carcinoma model. Cancer Res 2003; 63: 6056–6062.
Elloso MM, Phiel K, Henderson RA, Harris HA, Adelman SJ . Suppression of experimental autoimmune encephalomyelitis using estrogen receptor-selective ligands. J Endocrinol 2005; 185: 243–252.
Davis DD, Díaz-Cruz ES, Landini S, Kim Y-W, Brueggemeier RW . Evaluation of synthetic isoflavones on cell proliferation, estrogen receptor binding affinity, and apoptosis in human breast cancer cells. J Steroid Biochem Mol Biol 2008; 108: 23–31.
Meyers MJ, Sun J, Carlson KE, Marriner GA, Katzenellenbogen BS, Katzenellenbogen JA . Estrogen receptor-b potency-selective ligands: structure-activity relationship studies of diarylpropionitriles and their acetylene and polar analogues. J Med Chem 2001; 44: 4230–4251.
Imamov O, Shim GJ, Warner M, Gustafsson JA . Estrogen receptor beta in health and disease. Biol Reprod 2005; 73: 866–871.
Zhou Y, Xiao XQ, Chen LF, Yang R, Shi JD, Du XL et al. Proliferation and phenotypic changes of stromal cells in response to varying estrogen/androgen levels in castrated rats. Asian J Androl 2009; 11: 451–459.
Hong SG, Kim MK, Jang G, Oh HJ, Park JE, Kang JT et al. Generation of red fluorescent protein transgenic dogs. Genesis 2009; 47: 314–322.
Nicholson TM, Ricke EA, Marker PC, Miano JM, Mayer RD, Timms BG et al. Testosterone and 17β-estradiol induce glandular prostatic growth, bladder outlet obstruction, and voiding dysfunction in male mice. Endocrinology 2012; 153: 5556–5565.
Nomura H, Kawashima H, Masaki S, Hosono TY, Matsumura K, Tamada S et al. Effect of selective estrogen receptor modulators on cell proliferation and estrogen receptor activities in normal human prostate stromal and epithelial cells. Prostate Cancer Prostatic Dis 2009; 12: 375–381.
Nicholson TM, Ricke WA . Androgens and estrogens in benign prostatic hyperplasia: past, present and future. Differentiation 2011; 82: 184–199.
Corrada Y, Arias D, Rodriguez R, Spaini E, Fava F, Gobello C . Effect of tamoxifen citrate on reproductive parameters of male dogs. Theriogenology 2004; 61: 1327–1341.
Gonzalez G, Guendulain C, Maffrand C, Gobello C . Comparison of the effect of the aromatase inhibitor, anastrazole, to the antioestrogen, tamoxifen citrate, on canine prostate and semen. Reprod Domest Anim 2009; 44: 316–319.
Smith MR, Morton RA, Barnette KG, Sieber PR, Malkowicz SB, Rodriguez D et al. Toremifene to reduce fracture risk in men receiving androgen deprivation therapy for prostate cancer. J Urol 2010; 184: 1316–1321.
Taneja SS, Morton R, Barnette G, Sieber P, Hancock ML, Steiner M . Prostate cancer diagnosis among men with isolated high-grade intraepithelial neoplasia enrolled onto a 3-year prospective phase III clinical trial of oral toremifene. J Clin Oncol 2013; 31: 523–529.
Smith MR, Malkowicz SB, Chu F, Forrest J, Sieber P, Barnette KG et al. Toremifene improves lipid profiles in men receiving androgen-deprivation therapy for prostate cancer: interim analysis of a multicenter phase III study. J Clin Oncol 2008; 26: 1824–1829.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Garg, M., Dalela, D., Dalela, D. et al. Selective estrogen receptor modulators for BPH: new factors on the ground. Prostate Cancer Prostatic Dis 16, 226–232 (2013). https://doi.org/10.1038/pcan.2013.17
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pcan.2013.17
Keywords
This article is cited by
-
Which play a more important role in the development of large-sized prostates (≥80 ml), androgen receptors or oestrogen receptors? A comparative study
International Urology and Nephrology (2016)
-
Estrogens and Male Lower Urinary Tract Dysfunction
Current Urology Reports (2015)