Abstract
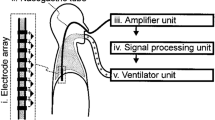
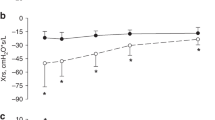
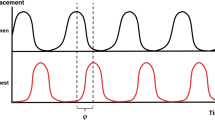
Mechanical ventilation may interfere with the spontaneous breathing pattern in infants because they have strong reflexes that play a large role in the control of breathing. This study aimed to answer the following questions: does a ventilator-assisted breath 1) reduce neural inspiratory time, 2) reduce the amplitude of the diaphragm electrical activity, and 3) prolong neural expiration, within the delivered breath? In 14 infants recovering from acute respiratory failure (mean age and weight were 2.3 ± 1.3 mo and 3.95 ± 0.82 kg, respectively), we measured 1) the electrical activity of the diaphragm with a multiple-array esophageal electrode, and 2) airway opening pressure, while patients breathed on synchronized intermittent mandatory ventilation (mean rate, 11.2 ± 6.5 breaths/min). We compared neural inspiratory and expiratory times for the mandatory breaths and for the spontaneous breaths immediately preceding and following the mandatory breath. Although neural inspiratory time was not different between mandatory and spontaneous breaths, neural expiratory time was significantly increased (p < 0.001) for the mandatory breaths (953 ± 449 ms) compared with the premandatory and postmandatory spontaneous breaths (607 ± 268 ms and 560 ± 227 ms, respectively). Delivery of the mandatory breath resulted in a reduction in neural respiratory frequency by 28.6 ± 6.4% from the spontaneous premandatory frequency. The magnitude of inspiratory electrical activity of the diaphragm was similar for all three breath conditions. For the mandatory breaths, ventilatory assist persisted for 507 ± 169 ms after the end of neural inspiratory time. Infant–ventilator asynchrony (both inspiratory and expiratory asynchrony) was present in every mandatory breath and constituted 53.4 ± 26.2% of the total breath duration.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Abbreviations
- EAdi:
-
electrical activity of the diaphragm
- HB:
-
Hering-Breuer
- Pao:
-
airway opening pressure
- SIMV:
-
synchronized intermittent mandatory ventilation
- Te:
-
expiratory time
- Ti:
-
inspiratory time
References
Cross KW, Klaus M, Tooley WH, Weisser K 1960 The response of the new-born baby to inflation of the lungs. J Physiol (Lond) 151: 551–565.
Hering E, Breuer J 1868 Die Selbststeurung der athmung durch den nervus vagus. Sitzber Deut Akad Wiss Wein 57: 672–677.
Greenough A, Morley C, Davis J 1983 Interaction of spontaneous respiration with artificial ventilation in preterm babies. J Pediatr 103: 769–773.
Giffin F, Greenough A, Naik S 1996 The Hering-Breuer reflex in ventilated children. Respir Med 90: 463–466.
Carlo WA, Ambalavanan N 1999 Conventional mechanical ventilation: traditional and new strategies. Pediatr Rev 20:e117–e126.
Parthasarathy S, Jubran A, Tobin MJ 2000 Assessment of neural inspiratory time in ventilator-supported patients. Am J Respir Crit Care Med 162: 546–552.
Beck J, Sinderby C, Lindström L, Grassino A 1996 Influence of bipolar esophageal electrode positioning on measurements of human crural diaphragm EMG. J Appl Physiol 81: 1434–1449.
Sinderby C, Beck J, Lindstrom L, Grassino A 1997 Enhancement of signal quality in esophageal recordings of diaphragm EMG. J Appl Physiol 82: 1370–1377.
Sinderby C, Beck J, Weinberg J, Spahija J, Grassino A 1998 Voluntary activation of the human diaphragm in health and disease. J Appl Physiol 85: 2146–2158.
Sinderby C, Navalesi P, Beck J, Skrobik Y, Comtois N, Friberg S, Gottfried SB, Lindstrom L 1999 Neural control of mechanical ventilation in respiratory failure. Nat Med 5: 1433–1436.
Beck J, Sinderby C, Weinberg J, Grassino A 1995 Effects of muscle-to-electrode distance on the human diaphragm electromyogram. J Appl Physiol 79: 975–985.
Sinderby CA, Comtois AS, Thomson RG, Grassino AE 1996 Influence of the bipolar electrode transfer function on the electromyogram power spectrum. Muscle Nerve 19: 290–301.
Laing IA, Teele RL, Stark AR 1988 Diaphragmatic movement in newborn infants. J Pediatr 112: 638–643.
Sinderby C, Lindstrom L, Grassino AE 1995 Automatic assessment of electromyogram quality. J Appl Physiol 79: 1803–1815.
Gandevia SC, McKenzie DK 1986 Human diaphragmatic EMG: changes with lung volume and posture during supramaximal phrenic stimulation. J Appl Physiol 60: 1420–1428.
Brancatisano A, Kelly SM, Tully A, Loring SH, Engel LA 1989 Postural changes in spontaneous and evoked regional diaphragmatic activity in dogs. J Appl Physiol 66: 1699–1705.
Beck J, Sinderby C, Lindstrom L, Grassino A 1998 Effects of lung volume on diaphragm EMG signal strength during voluntary contractions. J Appl Physiol 85: 1123–1134.
Sinderby C, Lindstrom L, Comtois N, Grassino AE 1996 Effects of diaphragm shortening on the mean action potential conduction velocity. J Physiol (Lond) 490: 207–214.
Brown K, Stocks J, Aun C, Rabette PS 1998 The Hering-Breuer reflex in anesthetized infants: end-inspiratory vs. end-expiratory occlusion techniques. J Appl Physiol 84: 1437–1446.
Rabbette PS, Stocks J 1998 Influence of volume dependency and timing of airway occlusions on the Hering-Breuer reflex in infants. J Appl Physiol 85: 2033–2039.
Hassan A, Gossage J, Ingram D, Lee S, Milner D 2001 Volume of activation of the Hering-Breuer inflation reflex in the newborn infant. J Appl Physiol 90: 763–769.
Merazzi D, Mortola J 1999 Hering-Breuer reflex in conscious newborn rats: effects of changes in ambient temperature during hypoxia. J Appl Physiol 87: 1656–1661.
Younes M, Vaillancourt P, Milic-Emili J 1974 Interaction between chemical factors and duration of apnea following lung inflation. J Appl Physiol 36: 190–201.
Knox CK 1973 Characteristics of inflation and deflation reflexes during expiration in cats. J Neurophysiol 36: 284–295.
Sammon M, Romaniuk JR, Bruce EN 1993 Bifurcations of the respiratory pattern produced with phasic vagal stimulation in the rat. J Appl Physiol 75: 912–926.
Clark FJ, von Euler C 1972 On the regulation of depth and rate of breathing. J Physiol (Lond) 222: 267–295.
Satoh M, Eastwood PR, Smith CA, Dempsey JA 2001 Nonchemical elimination of inspiratory motor output via mechanical ventilation in sleep. Am J Respir Crit Care Med 163: 1356–1364.
Kondili E, Prinianakis G, Anastasaki M, Georgopoulos D 2001 Acute effects of ventilator settings on respiratory motor output in patients with acute lung injury. Intensive Care Med 27: 1147–1157.
Bryan AC, Bryan MH, Kirkpatrick SM, Knill RL 1976 The use of airway occlusion in infants. Chest 70: 142–145.
Olinsky A, Bryan MH, Bryan AC 1974 Influence of lung inflation on respiratory control in neonates. J Appl Physiol 36: 426–429.
Witte MK, Carlo W 1987 Prolongation of inspiration during lower airway occlusion in children. J Appl Physiol 62: 1860–1864.
Younes M, Baker JP, Polachek J, Remmers JE 1978 Termination of inspiration through graded inhibition of inspiratory activity. Adv Exp Med 99: 383–395.
Imsand C, Feihl F, Perret C, Fitting JW 1994 Regulation of inspiratory neuromuscular output during synchronized intermittent mechanical ventilation. Anesthesiology 80: 13–22.
Esteban A, Anzueto A, Alia I, Gordo F, Apezteguia C, Palizas F, Cide D, Goldwaser R, Soto L, Bugedo G, Rodrigo C, Pimentel J, Raimondi G, Tobin MJ 2000 How is mechanical ventilation employed in the intensive care unit? Am J Respir Crit Care M. ed 161: 1450–1458.
Imanaka H, Nishimura M, Miyano H, Uemura H, Yagihara T 2001 Effect of synchronized intermittent mandatory ventilation on respiratory workload in infants after cardiac surgery. Anesthesiology 95: 881–888.
Sassoon C 1994 Intermittent mandatory ventilation. In: Tobin MJ (ed) Principles and Practice of Mechanical Ventilation. McGraw Hill, New York, 221–238.
Greenough A, Milner AD, Dimitriou G 2001 Synchronized mechanical ventilation for respiratory support in newborn infants. Cochrane Database Syst Rev 1: CD000456
Greenough A, Wood S, Morley CJ, Davis JA 1984 Pancuronium prevents pneumothoraces in ventilated premature babies who actively expire against positive pressure ventilation. Lancet 1: 1–13.
Lipscomb AP, Thorburn RJ, Reynolds EO, Blackwell RJ, Stewart AL, Blackwell RJ, Cusick G, Whitehead MD 1981 Pneumothorax and cerebral haemorrhage in preterm infants. Lancet 1: 414–416.
Henry GW, Stevens CS, Schreiner RL, Grosfeld JL, Ballantine TV 1979 Respiratory paralysis to improve oxygenation and mortality in large newborn infants with respiratory distress. J Pediatr Surg 14: 761–766.
Stark AR, Bascom R, Frantz ID 1978 Muscle relaxation in mechanically ventilated infants. J Pediatr 94: 439–443.
Tokioka H, Tanaka T, Ishizu T, Fukushima T, Iwaki T, Nakamura Y, Kosogabe Y 2001 The effect of breath termination criterion on breathing patterns and the work of breathing during pressure support ventilation. Anesth Analg 92: 161–165.
Calderini E, Confalonieri M, Puccio PG, Francavilla N, Stella L, Gregoretti C 1999 Patient-ventilator asynchrony during noninvasive ventilation: the role of expiratory trigger. Intensive Care Med 25: 662–667.
Al-Hathlol K, Idiong N, Hussain A, Kwiatkowski K, Alvaro RE, Weintraub Z, Cares DB, Rigatto H 2000 A study of breathing pattern and ventilation in newborn infants and adult subjects. Acta Paediatr 89: 1420–1425.
Navalesi P, Costa R 2003 New modes of mechanical ventilation: proportional assist ventilation, neurally adjusted ventilatory assist, and fractal ventilation. Curr Opin Crit Care 9: 51–58.
Acknowledgements
The authors thank M. Norman Comtois, M. Sylvain Morneau, R.T., and Mlle Roxanne Trahan, R.N., for their help during the studies. We also thank Dr. Jim Duffin for his comments on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by Fonds de la Recherche en Santé du Québec (FRSQ), Canadian Intensive Care Foundation, and Fondation de l'Hôpital Sainte-Justine.
Rights and permissions
About this article
Cite this article
Beck, J., Tucci, M., Emeriaud, G. et al. Prolonged Neural Expiratory Time Induced by Mechanical Ventilation in Infants. Pediatr Res 55, 747–754 (2004). https://doi.org/10.1203/01.PDR.0000119368.21770.33
Received:
Accepted:
Issue date:
DOI: https://doi.org/10.1203/01.PDR.0000119368.21770.33
This article is cited by
-
Quantifying neonatal patient effort using non-invasive model-based methods
Medical & Biological Engineering & Computing (2022)
-
Patient–ventilator asynchrony during conventional mechanical ventilation in children
Annals of Intensive Care (2017)
-
Neurally adjusted ventilatory assist (NAVA) allows patient-ventilator synchrony during pediatric noninvasive ventilation: a crossover physiological study
Critical Care (2015)
-
Evolution of inspiratory diaphragm activity in children over the course of the PICU stay
Intensive Care Medicine (2014)
-
La ventilation non invasive en mode NAVA (neurally adjusted ventilatory assist) en réanimation pédiatrique
Réanimation (2014)