Abstract
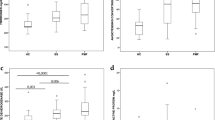
Sickle cell anemia (HbSS) is characterized by hypermetabolism, chronic inflammation, and increased oxidative stress, but the relationship between these factors is undefined. In this study, we examined indicators of inflammatory process and markers of oxidative damage and their impact on resting energy expenditure (REE) in stable HbSS adolescents (n = 35) and healthy controls carrying normal hemoglobin genotype (HbAA) (n = 39). C-reactive protein (CRP), white blood cell (WBC) count, and proinflammatory cytokines were measured as markers of inflammation and 2,3-dinor-5,6-dihydro-15-F2t-isoprostane (F2-IsoPM) as a marker of oxidative stress. REE was measured by indirect calorimetry. WBC counts (11.90 ± 5.3 ×103/μL versus 5.6 ± 1.9 ×103/μL; p < 0.001), serum CRP (9.1 ± 11.0 μg/mL versus 0.4 ± 0.7 μg/mL; p < 0.001) and serum IL-8 (7.5 ± 4.4 pg/mL versus 5.5 ± 4.8 pg/mL; p = 0.011) were higher in HbSS than HbAA, suggesting an anti-inflammatory response in HbSS. Higher urinary F2-IsoPM in HbSS (1.2 ± 0.4 versus 0.7 ± 0.3 ng/mg creatinine; p < 0.001) indicates increased oxidative stress. Fat free mass (FFM), hemoglobin (Hgb), interleukin (IL)-8, and F2-IsoPM were independent predictors of REE in HbSS (overall r2 = 0.778; p < 0.001). Low-grade inflammation and increased oxidative stress are present in adolescents with HbSS in the absence of acute crisis, and their markers are correlated with elevated REE.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Abbreviations
- CRP:
-
C-reactive protein
- F2-IsoPM:
-
2,3-dinor-5,6-dihydro-15-F2t-isoprostane
- FFM:
-
fat free mass
- FM:
-
fat mass
- GCRC:
-
General Clinical Research Center
- HbAA:
-
healthy controls carrying normal hemoglobin genotype
- HbSS:
-
sickle cell anemia
- Hgb:
-
hemoglobin
- REE:
-
resting energy expenditure
- RetCt%:
-
reticulocyte proportion
- WBC:
-
circulating white blood cell
References
Bunn HF 1997 Pathogenesis and treatment of sickle cell disease. N Engl J Med 337: 762–769
Embury SH, Hebbel RP, Steinberg MH, Mohandas N 1994 Pathogenesis of vasoocclusion. In: Embury SH, Hebbel RP, Mohandas N, Steinberg MH (eds) Sickle Cell Disease: Basic Principles and Clinical Practice. Lippincott-Raven, Philadelphia, pp 311–326
Akinola NO, Stevens SM, Franklin IM, Nash GB, Stuart J 1992 Subclinical ischaemic episodes during the steady state of sickle cell anaemia. J Clin Pathol 45: 902–906
Duits AJ, Schnog JB, Lard LR, Saleh AW, Rojer RA 1998 Elevated IL-8 levels during sickle cell crisis. Eur J Haematol 61: 302–305
Hibbert JM, Hsu LL, Bhathena SJ, Irune I, Sarfo B, Creary MS, Gee BE, Mohamed AI, Buchanan ID, Al-Mahmoud A, Stiles JK 2005 Proinflammatory cytokines and the hypermetabolism of children with sickle cell disease. Exp Biol Med (Maywood) 230: 68–74
Makis AC, Hatzimichael EC, Stebbing J, Bourantas KL 2006 C-reactive protein and vascular cell adhesion molecule-1 as markers of severity in sickle cell disease. Arch Intern Med 166: 366–368
Hebbel RP, Eaton JW, Balasingam M, Steinberg MH 1982 Spontaneous oxygen radical generation by sickle erythrocytes. J Clin Invest 70: 1253–1259
Hebbel RP 1991 Beyond hemoglobin polymerization: the red blood cell membrane and sickle disease pathophysiology. Blood 77: 214–237
Klings ES, Farber HW 2001 Role of free radicals in the pathogenesis of acute chest syndrome in sickle cell disease. Respir Res 2: 280–285
Aslan M, Thornley-Brown D, Freeman BA 2000 Reactive species in sickle cell disease. Ann N Y Acad Sci 899: 375–391
Jain SK, Shohet SB 1984 A novel phospholipid in irreversibly sickled cells: evidence for in vivo peroxidative membrane damage in sickle cell disease. Blood 63: 362–367
Morrow JD, Hill KE, Burk RF, Nammour TM, Badr KF, Roberts LJ 2nd 1990 A series of prostaglandin F2-like compounds are produced in vivo in humans by a non-cyclooxygenase, free radical-catalyzed mechanism. Proc Natl Acad Sci U S A 87: 9383–9387
Davi G, Ciabattoni G, Consoli A, Mezzetti A, Falco A, Santarone S, Pennese E, Vitacolonna E, Bucciarelli T, Costantini F, Capani F, Patrono C 1999 In vivo formation of 8-iso-prostaglandin F2{alpha} and platelet activation in diabetes mellitus: effects of improved metabolic control and vitamin E supplementation. Circulation 99: 224–229
Klings ES, Christman BW, McClung J, Stucchi AF, McMahon L, Brauer M, Farber HW 2001 Increased F2 isoprostanes in the acute chest syndrome of sickle cell disease as a marker of oxidative stress. Am J Respir Crit Care Med 164: 1248–1252
Psathakis K, Papatheodorou G, Plataki M, Panagou P, Loukides S, Siafakas NM, Bouros D 2004 8-Isoprostane, a marker of oxidative stress, is increased in the expired breath condensate of patients with pulmonary sarcoidosis. Chest 125: 1005–1011
Roberts LJ, Morrow JD 2000 Measurement of F(2)-isoprostanes as an index of oxidative stress in vivo. Free Radic Biol Med 28: 505–513
Barden EM, Zemel BS, Kawchak DA, Goran MI, Ohene-Frempong K, Stallings VA 2000 Total and resting energy expenditure in children with sickle cell disease. J Pediatr 136: 73–79
Buchowski MS, Chen KY, Byrne D, Wang WC 2002 Equation to estimate resting energy expenditure in adolescents with sickle cell anemia. Am J Clin Nutr 76: 1335–1344
Salman EK, Haymond MW, Bayne E, Sager BK, Wiisanen A, Pitel P, Darmaun D 1996 Protein and energy metabolism in prepubertal children with sickle cell anemia. Pediatr Res 40: 34–40
Buchholz AC, Buchowski MS 2004 Energy and protein metabolism in sickle cell disease: Evidence of aberrations. In: Focus on Sickle Cell Research. Plasmar RL (ed). Nova Science Publishers, Hauppauge, NY, pp 1–17
Adams JG 3rd 1994 Clinical laboratory diagnosis. In: Embury SH, Hebbel RP, Mohandas N, Steinberg MH (eds) Sickle Cell Disease: Basic Principles and Clinical Practice. Lippincott-Raven, Philadelphia, pp 457–468
Henry CJ, Lightowler HJ, Marchini J 2003 Intra-individual variation in resting metabolic rate during the menstrual cycle. Br J Nutr 89: 811–817
Morrow JD, Zackert WE, Yang JP, Kurhts EH, Callewaert D, Dworski R, Kanai K, Taber D, Moore K, Oates JA, Roberts LJ 1999 Quantification of the major urinary metabolite of 15-F2t-isoprostane (8-iso-PGF2[alpha]) by a stable isotope dilution mass spectrometric assay. Anal Biochem 269: 326–331
Poehlman ET, Toth MJ 1995 Mathematical ratios lead to spurious conclusions regarding age- and sex- related differences in resting metabolic rate. Am J Clin Nutr 61: 482–485
Chies JA, Nardi NB 2001 Sickle cell disease: a chronic inflammatory condition. Med Hypotheses 57: 46–50
Goncalves MS, Queiroz IL, Cardoso SA, Zanetti A, Strapazoni AC, Adorno E, Albuquerque A, Sant'Ana A, dos Reis MG, Barral A, Barral Netto M 2001 Interleukin 8 as a vaso-occlusive marker in Brazilian patients with sickle cell disease. Braz J Med Biol Res 34: 1309–1313
Ridker PM, Hennekens CH, Buring JE, Rifai N 2000 C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med 342: 836–843
Harada A, Mukaida N, Matsushima K 1996 Interleukin 8 as a novel target for intervention therapy in acute inflammatory diseases. Mol Med Today 2: 482–489
Okpala I 2006 Leukocyte adhesion and the pathophysiology of sickle cell disease. Curr Opin Hematol 13: 40–44
Hammerman SI, Klings ES, Hendra KP, Upchurch GR Jr, Rishikof DC, Loscalzo J, Farber HW 1999 Endothelial cell nitric oxide production in acute chest syndrome. Am J Physiol 277: H1579–H1592
Kaul DK, Hebbel RP 2000 Hypoxia/reoxygenation causes inflammatory response in transgenic sickle mice but not in normal mice. J Clin Invest 106: 411–420
Utaka S, Avesani CM, Draibe SA, Kamimura MA, Andreoni S, Cuppari L 2005 Inflammation is associated with increased energy expenditure in patients with chronic kidney disease. Am J Clin Nutr 82: 801–805
Badaloo A, Jackson AA, Jahoor F 1989 Whole body protein turnover and resting metabolic rate in homozygous sickle cell disease. Clin Sci (Lond) 77: 93–97
Borel MJ, Buchowski MS, Turner EA, Goldstein RE, Flakoll PJ 1998 Protein turnover and energy expenditure increase during exogenous nutrient availability in sickle cell disease. Am J Clin Nutr 68: 607–614
Wautier JL, Pintigny D, Maclouf J, Wautier MP, Corvazier E, Caen J 1986 Release of prostacyclin after erythrocyte adhesion to cultured vascular endothelium. J Lab Clin Med 107: 210–215
Alexander N, Higgs D, Dover G, Serjeant GR 2004 Are there clinical phenotypes of homozygous sickle cell disease?. Br J Haematol 126: 606–611
Kato GJ, Martyr S, Blackwelder WC, Nichols JS, Coles WA, Hunter LA, Brennan ML, Hazen SL, Gladwin MT 2005 Levels of soluble endothelium-derived adhesion molecules in patients with sickle cell disease are associated with pulmonary hypertension, organ dysfunction, and mortality. Br J Haematol 130: 943–953
Harmatz P, Butensky E, Quirolo K, Williams R, Ferrell L, Moyer T, Golden D, Neumayr L, Vichinsky E 2000 Severity of iron overload in patients with sickle cell disease receiving chronic red blood cell transfusion therapy. Blood 96: 76–79
Brittenham GM, Cohen AR, McLaren CF, Martin MB, Griffith PM, Nienhuis AW, Young NS, Allen CJ, Farrell DE, Harris JW 1993 Hepatic iron stores and plasma ferritin concentration in patients with sickle cell anemia and thalassemia major. Am J Hematol 42: 81–85
Acknowledgements
The authors thank the staff of the General Clinical Research Center at Vanderbilt University for help with this project. They also thank Kay Hongu, Ph.D., and Cindy Dorminy, M.Ed., for their technical assistance; Dan Byrne, M.S., for statistical expertise in analyzing the data; and Leena Choi, Ph.D., for helping with graphic data presentation. Finally, they acknowledge our participants and their parents for their enthusiasm and commitment to this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Study supported in part by National Institutes of Health grants M01 RR00095 and by funds from GM008037, GM15431, CA77839, DK48831, and ES13125.
Rights and permissions
About this article
Cite this article
Akohoue, S., Shankar, S., Milne, G. et al. Energy Expenditure, Inflammation, and Oxidative Stress in Steady-State Adolescents With Sickle Cell Anemia. Pediatr Res 61, 233–238 (2007). https://doi.org/10.1203/pdr.0b013e31802d7754
Received:
Accepted:
Issue date:
DOI: https://doi.org/10.1203/pdr.0b013e31802d7754
This article is cited by
-
Does ( −)-epigallocatechin-3-gallate protect the neurotoxicity induced by bisphenol A in vivo?
Environmental Science and Pollution Research (2022)
-
Nutritional perspectives on sickle cell disease in Africa: a systematic review
BMC Nutrition (2021)
-
Precipitating factors and targeted therapies in combating the perils of sickle cell disease--- A special nutritional consideration
Nutrition & Metabolism (2016)
-
Triterpenoid inducers of Nrf2 signaling as potential therapeutic agents in sickle cell disease: a review
Frontiers of Medicine (2015)
-
Genetic polymorphism of APOB is associated with diabetes mellitus in sickle cell disease
Human Genetics (2015)