Abstract
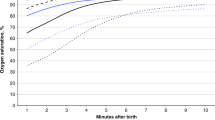
The optimal inhaled oxygen fraction for newborn resuscitation is still not settled. We hypothesized that short-lasting oxygen ventilation after intrauterine asphyxia would not cause arterial or cerebral hyperoxia, and therefore be innocuous. The umbilical cord of fetal sheep was clamped and 10 min later, after delivery, ventilation with air (n = 7) or with 100% oxygen for 3 (n = 6) or 30 min (n = 5), followed by air, was started. Among the 11 lambs given 100% oxygen, oxygen tension (PO2) was 10.7 (1.8–56) kPa [median (range)] in arterial samples taken after 2.5 min of ventilation. In those ventilated with 100% oxygen for 30 min, brain tissue PO2 (PbtO2) increased from less than 0.1 kPa in each lamb to individual maxima of 56 (30–61) kPa, whereas in those given oxygen for just 3 min, PbtO2 peaked at 4.2 (2.9–46) kPa. The maximal PbtO2 in air-ventilated lambs was 2.9 (0.8–5.4) kPa. Heart rate and blood pressure increased equally fast in the three groups. Thus, prolonged ventilation with 100% oxygen caused an increase in PbtO2 of a magnitude previously only reported under hyperbaric conditions. Reducing the time of 100% oxygen ventilation to 3 min did not consistently avert systemic hyperoxia.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Abbreviations
- BE:
-
arterial base excess
- Bpm:
-
beats per minute
- CrSO2:
-
regional cerebral oxygen saturation
- FiO2:
-
inspired fraction of oxygen
- Hb:
-
hemoglobin
- HR:
-
heart rate
- MAP:
-
mean arterial pressure
- PbtO2:
-
brain tissue partial pressure of oxygen
References
The International Liaison Committee on Resuscitation 2006 The International Liaison Committee on Resuscitation (ILCOR) consensus on science with treatment recommendations for pediatric and neonatal patients: pediatric basic and advanced life support. Pediatrics 117: e955–e977
Munkeby BH, Børke WB, Bjørnland K, Sikkeland LI, Borge GI, Halvorsen B, Saugstad OD 2004 Resuscitation with 100% O2 increases cerebral injury in hypoxemic piglets. Pediatr Res 56: 783–790
Graulich J, Hoffmann U, Maier RF, Ruscher K, Pomper JK, Ko HK, Gabriel S, Obladen M, Heinemann U 2002 Acute neuronal injury after hypoxia is influenced by the reoxygenation mode in juvenile hippocampal slice cultures. Brain Res Dev Brain Res 137: 35–42
Døhlen G, Carlsen H, Blomhoff R, Thaulow E, Saugstad OD 2005 Reoxygenation of hypoxic mice with 100% oxygen induces brain nuclear factor-kappa B. Pediatr Res 58: 941–945
Solas AB, Munkeby BH, Saugstad OD 2004 Comparison of short- and long-duration oxygen treatment after cerebral asphyxia in newborn piglets. Pediatr Res 56: 125–131
Saugstad OD, Rootwelt T, Aalen O 1998 Resuscitation of asphyxiated newborn infants with room air or oxygen: an international controlled trial: the Resair 2 study. Pediatrics 102: e1
Ramji S, Rasaily R, Mishra PK, Narang A, Jayam S, Kapoor AN, Kambo I, Mathur A, Saxena BN 2003 Resuscitation of asphyxiated newborns with room air or 100% oxygen at birth: a multicentric clinical trial. Indian Pediatr 40: 510–517
Vento M, Asensi M, Sastre J, Lloret A, Garcia-Sala F, Vina J 2003 Oxidative stress in asphyxiated term infants resuscitated with 100% oxygen. J Pediatr 142: 240–246
Vento M, Sastre J, Asensi MA, Vina J 2005 Room-air resuscitation causes less damage to heart and kidney than 100% oxygen. Am J Respir Crit Care Med 172: 1393–1398
Naumburg E, Bellocco R, Cnattingius S, Jonzon A, Ekbom A 2002 Supplementary oxygen and risk of childhood lymphatic leukaemia. Acta Paediatr 91: 1328–1333
Spector LG, Klebanoff MA, Feusner JH, Georgieff MK, Ross JA 2005 Childhood cancer following neonatal oxygen supplementation. J Pediatr 147: 27–31
Rabi Y, Rabi D, Yee W 2007 Room air resuscitation of the depressed newborn: a systematic review and meta-analysis. Resuscitation 72: 353–363
Vento M, Asensi M, Sastre J, García-Sala F, Pallardó FV, Viña J 2001 Resuscitation with room air instead of 100% oxygen prevents oxidative stress in moderately asphyxiated term neonates. Pediatrics 107: 642–647
Kamlin CO, O'Donnell CP, Davis PG, Morley CJ 2006 Oxygen saturation in healthy infants immediately after birth. J Pediatr 148: 585–589
Rabi Y, Yee W, Chen SY, Singhal N 2006 Oxygen saturation trends immediately after birth. J Pediatr 148: 590–594
Markus T, Hansson S, Amer-Wåhlin I, Saugstad OD, Hellström-Westas L, Ley D 2007 Cerebral inflammatory response after fetal asphyxia and hyperoxic resuscitation in newborn sheep. Pediatr Res 62: 71–77
Robertson B 1992 Animal models of neonatal surfactant dysfunction. In: Robertson B, van Golde LM, Batenburg JJ (eds) Pulmonary Surfactant: from Molecular Biology to Clinical Practice. Elsevier Science Publishers B.V., Amsterdam, pp 459–484
van Hulst RA, Haitsma JJ, Klein J, Lachmann B 2003 Oxygen tension under hyperbaric conditions in healthy pig brain. Clin Physiol Funct Imaging 23: 143–148
Thorngren-Jerneck K, Ley D, Hellström-Westas L, Hernandez-Andrade E, Lingman G, Ohlsson T, Oskarsson G, Pesonen E, Sandell A, Strand SE, Werner O, Marsal K 2001 Reduced postnatal cerebral glucose metabolism measured by PET after asphyxia in near term fetal lambs. J Neurosci Res 66: 844–850
Lyng K, Braakhuis M, Frøen JF, Stray-Pedersen B, Saugstad OD 2005 Inflammation increases vulnerability to hypoxia in newborn piglets: effect of reoxygenation with 21% and 100% O2. Am J Obstet Gynecol 192: 1172–1178
Saugstad OD 2004 The role of oxygen in neonatal resuscitation. Clin Perinatol 31: 431–443
Grosenbaugh DA, Alben JO, Muir WW 1997 Absorbance spectra of inter-species hemoglobins in the visible and near infrared regions. J Vet Emerg Crit Care 7: 36–42
Haase E, Bigam DL, Nakonechny QB, Rayner D, Korbutt G, Cheung PY 2005 Cardiac function, myocardial glutathione, and matrix metalloproteinase-2 levels in hypoxic newborn pigs reoxygenated by 21%, 50%, or 100% oxygen. Shock 23: 383–389
Acknowledgements
We thank Tina Markus for the analysis of cytokine expression in brain tissue, GE Healthcare Technologies for lending a Datex-Ohmeda AS/3 Compact Anesthesia Monitor, and Research Manager, Juha Virtanen, Ph.D., for technical advice.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by The Laerdal Foundation, The Swedish Medical Research Council (grant nos 14940, 4732), University Hospital of Lund and Lund's Medical Faculty grants, the Segerfalk Foundation, and the Craaford Foundation.
Rights and permissions
About this article
Cite this article
Perez-de-Sa, V., Cunha-Goncalves, D., Nordh, A. et al. High Brain Tissue Oxygen Tension During Ventilation With 100% Oxygen After Fetal Asphyxia in Newborn Sheep. Pediatr Res 65, 57–61 (2009). https://doi.org/10.1203/PDR.0b013e31818a01a4
Received:
Accepted:
Issue date:
DOI: https://doi.org/10.1203/PDR.0b013e31818a01a4
This article is cited by
-
Neonatal chest compressions: time to act
Pediatric Research (2021)
-
Randomized trial of oxygen weaning strategies following chest compressions during neonatal resuscitation
Pediatric Research (2021)
-
Versorgung und Reanimation des Neugeborenen nach der Geburt
Notfall + Rettungsmedizin (2021)
-
Excess cerebral oxygen delivery follows return of spontaneous circulation in near-term asphyxiated lambs
Scientific Reports (2020)
-
Neonatal resuscitation adhering to oxygen saturation guidelines in asphyxiated lambs with meconium aspiration
Pediatric Research (2016)