Abstract
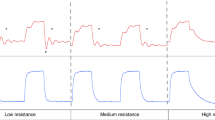
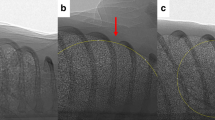
The effect of a 20 s sustained inflation (SI) and positive end-expiratory pressure (PEEP) on functional residual capacity (FRC) formation at birth were investigated. Preterm rabbit pups (28 d) were randomized at birth into four groups (n = 6 for each): 1) SI, PEEP 5 cm H2O, 2) no SI, PEEP 5 cm H2O, 3) no SI + no PEEP, 4) SI + no PEEP. FRC and tidal volume (Vt) were measured by plethysmography and uniformity of lung aeration by phase contrast x-ray imaging. Ventilation with a SI and PEEP uniformly aerated the lung and Vt and FRC were recruited by the first tidal inflation. Ventilation without a SI, with PEEP, gradually recruited Vt and FRC with each inflation but aeration was not uniform. Ventilation without a SI or PEEP, gradually recruited Vt, but no FRC. Ventilation with a SI, without PEEP, uniformly aerated the lung and recruited Vt but no FRC. FRC was greater with SI (p = 0.006) during the first minute, but was larger with PEEP than without PEEP throughout the first 7 min (p < 0.0005). Effects of PEEP and SI were additive. In ventilated preterm rabbits at birth, combining a SI and PEEP improved FRC formation and uniformity of lung aeration, but PEEP had the greatest influence.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Abbreviations
- FRC:
-
functional residual capacity
- PEEP:
-
positive end-expiratory pressure
- PPV:
-
positive pressure ventilation
- SI:
-
sustained inflation
- Vt:
-
tidal volume
References
International Liaison Committee on Resuscitation 2006 The International Liaison Committee on Resuscitation (ILCOR) consensus on science with treatment recommendations for pediatric and neonatal patients: neonatal resuscitation. Pediatrics 117: e978–e988
Bjorklund LJ, Ingimarsson J, Curstedt T, John J, Robertson B, Werner O, Vilstrup CT 1997 Manual ventilation with a few large breaths at birth compromises the therapeutic effect of subsequent surfactant replacement in immature lambs. Pediatr Res 42: 348–355
Wada K, Jobe AH, Ikegami M 1997 Tidal volume effects on surfactant treatment responses with the initiation of ventilation in preterm lambs. J Appl Physiol 83: 1054–1061
Lindner W, Vossbeck S, Hummler H, Pohlandt F 1999 Delivery room management of extremely low birth weight infants: spontaneous breathing or intubation?. Pediatrics 103: 961–967
Aly H, Massaro AN, Patel K, El Mohandes AA 2005 Is it safer to intubate premature infants in the delivery room?. Pediatrics 115: 1660–1665
te Pas AB, Walther FJ 2007 A randomized, controlled trial of delivery-room respiratory management in very preterm infants. Pediatrics 120: 322–329
Jobe AH, Kramer BW, Moss TJ, Newnham JP, Ikegami M 2002 Decreased indicators of lung injury with continuous positive expiratory pressure in preterm lambs. Pediatr Res 52: 387–392
Thomson MA, Yoder BA, Winter VT, Martin H, Catland D, Siler-Khodr TM, Coalson JJ 2004 Treatment of immature baboons for 28 days with early nasal continuous positive airway pressure. Am J Respir Crit Care Med 169: 1054–1062
Bjorklund LJ, Ingimarsson J, Curstedt T, Larsson A, Robertson B, Werner O 2001 Lung recruitment at birth does not improve lung function in immature lambs receiving surfactant. Acta Anaesthesiol Scand 45: 986–993
Ingimarsson J, Bjorklund LJ, Curstedt T, Gudmundsson S, Larsson A, Robertson B, Werner O 2004 Incomplete protection by prophylactic surfactant against the adverse effects of large lung inflations at birth in immature lambs. Intensive Care Med 30: 1446–1453
Ikegami M, Kallapur S, Michna J, Jobe AH 2000 Lung injury and surfactant metabolism after hyperventilation of premature lambs. Pediatr Res 47: 398–404
Lindner W, Hogel J, Pohlandt F 2005 Sustained pressure-controlled inflation or intermittent mandatory ventilation in preterm infants in the delivery room? A randomized, controlled trial on initial respiratory support via nasopharyngeal tube. Acta Paediatr 94: 303–309
Vyas H, Milner AD, Hopkin IE, Boon AW 1981 Physiologic responses to prolonged and slow-rise inflation in the resuscitation of the asphyxiated newborn infant. J Pediatr 99: 635–639
Upton CJ, Milner AD 1991 Endotracheal resuscitation of neonates using a rebreathing bag. Arch Dis Child 66: 39–42
Naik AS, Kallapur SG, Bachurski CJ, Jobe AH, Michna J, Kramer BW, Ikegami M 2001 Effects of ventilation with different positive end-expiratory pressures on cytokine expression in the preterm lamb lung. Am J Respir Crit Care Med 164: 494–498
Morley C 2007 New Australian Neonatal Resuscitation Guidelines. J Paediatr Child Health 43: 6–8
Kitchen MJ, Lewis RA, Morgan MJ, Wallace MJ, Siew ML, Siu KK, Habib A, Fouras A, Yagi N, Uesugi K, Hooper SB 2008 Dynamic measures of regional lung air volume using phase contrast x-ray imaging. Phys Med Biol 53: 6065–6077
Hooper SB, Kitchen MJ, Wallace MJ, Yagi N, Uesugi K, Morgan MJ, Hall C, Siu KK, Williams IM, Siew M, Irvine SC, Pavlov K, Lewis RA 2007 Imaging lung aeration and lung liquid clearance at birth. FASEB J 21: 3329–3337
Lewis RA, Yagi N, Kitchen MJ, Morgan MJ, Paganin D, Siu KK, Pavlov K, Williams I, Uesugi K, Wallace MJ, Hall CJ, Whitley J, Hooper SB 2005 Dynamic imaging of the lungs using x-ray phase contrast. Phys Med Biol 50: 5031–5040
Lachmann B, Grossmann G, Nilsson R, Robertson B 1979 Lung mechanics during spontaneous ventilation in premature and fullterm rabbit neonates. Respir Physiol 38: 283–302
Vyas H, Field D, Milner AD, Hopkin IE 1986 Determinants of the first inspiratory volume and functional residual capacity at birth. Pediatr Pulmonol 2: 189–193
Vyas H, Milner AD, Hopkins IE 1981 Intrathoracic pressure and volume changes during the spontaneous onset of respiration in babies born by cesarean section and by vaginal delivery. J Pediatr 99: 787–791
Milner AD, Saunders RA, Hopkin IE 1978 Is air trapping important in the maintenance of the functional residual capacity in the hours after birth?. Early Hum Dev 2: 97–105
Boon AW, Milner AD, Hopkin IE 1979 Lung expansion, tidal exchange, and formation of the functional residual capacity during resuscitation of asphyxiated neonates. J Pediatr 95: 1031–1036
Milner AD, Sauders RA 1977 Pressure and volume changes during the first breath of human neonates. Arch Dis Child 52: 918–924
Saunders RA, Milner AD 1978 Pulmonary pressure/volume relationships during the last phase of delivery and the first postnatal breaths in human subjects. J Pediatr 93: 667–673
Karlberg P, Cherry RB, Escardo FE, Koch G 1962 Repiratory Studies in Newborn Infants. II: pulmonary ventilation and mechanics of breathing in the first minutes of life, including the onset of respiration. Acta Paediatr 51: 121–136
Mortola JP, Fisher JT, Smith JB, Fox GS, Weeks S, Willis D 1982 Onset of respiration in infants delivered by cesarean section. J Appl Physiol 52: 716–724
Probyn ME, Hooper SB, Dargaville PA, McCallion N, Crossley K, Harding R, Morley CJ 2004 Positive end expiratory pressure during resuscitation of premature lambs rapidly improves blood gases without adversely affecting arterial pressure. Pediatr Res 56: 198–204
Probyn ME, Hooper SB, Dargaville PA, McCallion N, Harding R, Morley CJ 2005 Effects of tidal volume and positive end-expiratory pressure during resuscitation of very premature lambs. Acta Paediatr 94: 1764–1770
O'Donnell C, Davis P, Morley C 2004 Positive end-expiratory pressure for resuscitation of newborn infants at birth. Cochrane Database Syst Rev 4: CD004341
Finer NN, Carlo WA, Duara S, Fanaroff AA, Donovan EF, Wright LL, Kandefer S, Poole WK 2004 Delivery room continuous positive airway pressure/positive end-expiratory pressure in extremely low birth weight infants: a feasibility trial. Pediatrics 114: 651–657
Enhorning G, Robertson B 1972 Lung expansion in the premature rabbit fetus after tracheal deposition of surfactant. Pediatrics 50: 58–66
Enhorning G, Grossman G, Robertson B 1973 Effect of tracheal deposition of surfactant on air expansion of lungs–study on premature rabbit fetuses. Arch Dis Child 48: 162
Author information
Authors and Affiliations
Corresponding author
Additional information
Support was provided by SPring-8 synchrotron facility (Japan), granted under the approval of the SPring-8 Program Review Committee (proposal nos. 2006B0002, 2007A0002).A.B.P. is a recipient of a Ter Meulen Fund grant for working visits, Royal Netherlands Academy of Arts and Sciences, The Netherlands and recipient of a Royal Women's Hospital postgraduate scholarship. M.J.K. is a recipient of an ARC Post-Doctoral Fellowship.
Rights and permissions
About this article
Cite this article
te Pas, A., Siew, M., Wallace, M. et al. Establishing Functional Residual Capacity at Birth: The Effect of Sustained Inflation and Positive End-Expiratory Pressure in a Preterm Rabbit Model. Pediatr Res 65, 537–541 (2009). https://doi.org/10.1203/PDR.0b013e31819da21b
Received:
Accepted:
Issue date:
DOI: https://doi.org/10.1203/PDR.0b013e31819da21b
This article is cited by
-
Sustained inflation improves initial lung aeration in newborn rabbits with a diaphragmatic hernia
Pediatric Research (2024)
-
Comparison of positive pressure ventilation devices during compliance changes in a neonatal ovine model
Pediatric Research (2024)
-
Critical functional lung volumes in neonatal intensive care: evidence and clinical applications
Pediatric Research (2023)
-
Respiratory strategy at birth initiates distinct lung injury phenotypes in the preterm lamb lung
Respiratory Research (2022)
-
Lung recruitment improves the efficacy of intubation-surfactant-extubation treatment for respiratory distress syndrome in preterm neonates, a randomized controlled trial
BMC Pediatrics (2022)