Abstract
Although genetic defect of complement factor H (CFH) is a common cause of atypical hemolytic uremic syndrome (aHUS), development of autoantibodies to CFH (CFH-Ab) is also known to be an acquired cause of aHUS. Recently, a correlation between the development of CFH-Ab and the deficiency of the CFH-related proteins, CFHR1 and CFHR3, was identified. In this study, plasma complement profiles were measured and genetic analysis of the CFH, CFI, MCP, CFHR1, and CFHR3 genes were performed in three female patients diagnosed with aHUS with positive CFH-Ab. Acute stage plasmas of all the three patients revealed low C3, low or low-normal CFH antigenic levels, and high titers of CFH-Ab. All the patients also showed complete plasma CFHR1 deficiency and homozygous genomic deletion of CFHR1/CFHR3, but none had CFH, CFI, or MCP mutations. All the patients were treated with plasmapheresis, and two patients required additional immunosuppressive therapy. These patients had a novel subgroup of aHUS characterized by a combination of genetic (a homozygous deletion of CFHR1/CFHR3) and acquired (development of CFH-Ab) factors. Patients with this disease may need intensive immunosuppressive therapy in addition to plasmapheresis. Screening for CFH-Ab and the CFHR1/CFHR3 deficiency should be included in the diagnostic tests for patients with aHUS.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Abbreviations
- aHUS:
-
atypical hemolytic uremic syndrome
- ANA:
-
antinuclear antibody
- CCP:
-
complement control protein module
- CFH:
-
complement factor H
- CFH-Ab:
-
anticomplement factor H autoantibodies
- CFHR:
-
complement factor H-related protein
- HUS:
-
hemolytic uremic syndrome
References
Noris M, Remuzzi G 2005 Hemolytic uremic syndrome. J Am Soc Nephrol 16: 1035–1050
Kavanagh D, Goodship TH, Richards A 2006 Atypical haemolytic uraemic syndrome. Br Med Bull 77-78: 5–22
Caprioli J, Noris M, Brioschi S, Pianetti G, Castelletti F, Bettinaglio P, Mele C, Bresin E, Cassis L, Gamba S, Porrati F, Bucchioni S, Monteferrante G, Fang CJ, Liszewski MK, Kavanagh D, Atkinson JP, Remuzzi G 2006 Genetics of HUS: the impact of MCP, CFH, and IF mutations on clinical presentation, response to treatment, and outcome. Blood 108: 1267–1279
Sellier-Leclerc AL, Frémeaux-Bacchi V, Dragon-Durey MA, Macher MA, Niaudet P, Guest G, Boudailliez B, Bouissou F, Deschenes G, Gie S, Tsimaratos M, Fischbach M, Morin D, Nivet H, Alberti C, Loirat C 2007 Differential impact of complement mutations on clinical characteristics in atypical hemolytic uremic syndrome. J Am Soc Nephrol 18: 2392–2400
Goicoechea de Jorge E, Harris CL, Esparza-Gordillo J, Carreras L, Arranz EA, Garrido CA, Lopez-Trascasa M, Sanchez-Corral P, Morgan BP, Rodriguez de Cordoba S 2007 Gain-of-function mutations in complement factor B are associated with atypical hemolytic uremic syndrome. Proc Natl Acad Sci USA 104: 240–245
Frémeaux-Bacchi V, Miller EC, Liszewski MK, Strain L, Blouin J, Brown AL, Moghal N, Kaplan BS, Weiss RA, Lhotta K, Kapur G, Mattoo T, Nivet H, Wong W, Gie S, Hurault de Ligny B, Fischbach M, Gupta R, Hauhart R, Meunier V, Loirat C, Dragon-Durey MA, Fridman WH, Janssen BJ, Goodship TH, Atkinson JP 2008 Mutations in complement C3 predispose to development of atypical hemolytic uremic syndrome. Blood 112: 4948–4952
Neumann HP, Salzmann M, Bohnert-Iwan B, Mannuelian T, Skerka C, Lenk D, Bender BU, Cybulla M, Riegler P, Konigsrainer A, Neyer U, Bock A, Widmer U, Male DA, Franke G, Zipfel PF 2003 Haemolytic uraemic syndrome and mutations of the factor H gene: a registry-based study of German speaking countries. J Med Genet 40: 676–681
Dragon-Durey MA, Frémeaux-Bacchi V 2005 Atypical haemolytic uraemic syndrome and mutations in complement regulator genes. Springer Semin Immunopathol 27: 359–374
Frémeaux-Bacchi V, Kemp EJ, Goodship JA, Dragon-Durey MA, Strain L, Loirat C, Deng HW, Goodship TH 2005 The development of atypical haemolytic-uraemic syndrome is influenced by susceptibility factors in factor H and membrane cofactor protein: evidence from two independent cohorts. J Med Genet 42: 852–856
Esparza-Gordillo J, Goicoechea de Jorge E, Buil A, Carreras Berges L, Lopez-Trascasa M, Sanchez-Corral P, Rodriguez de Cordoba S 2005 Predisposition to atypical hemolytic uremic syndrome involves the concurrence of different susceptibility alleles in the regulators of complement activation gene cluster in 1q32. Hum Mol Genet 14: 703–712
Józsi M, Strobel S, Dahse HM, Liu WS, Hoyer PF, Oppermann M, Skerka C, Zipfel PF 2007 Anti factor H autoantibodies block C-terminal recognition function of factor H in hemolytic uremic syndrome. Blood 110: 1516–1518
Dragon-Durey MA, Loirat C, Cloarec S, Macher MA, Blouin J, Nivet H, Weiss L, Fridman WH, Fremeaux-Bacchi V 2005 Anti-Factor H autoantibodies associated with atypical hemolytic uremic syndrome. J Am Soc Nephrol 16: 555–563
Józsi M, Licht C, Strobel S, Zipfel SL, Richter H, Heinen S, Zipfel PF, Skerka C 2008 Factor H autoantibodies in atypical hemolytic uremic syndrome correlate with CFHR1/CFHR3 deficiency. Blood 111: 1512–1514
Male DA, Ormsby RJ, Ranganathan S, Giannakis E, Gordon DL 2000 Complement factor H: sequence analysis of 221 kb of human genomic DNA containing the entire fH, fHR-1 and fHR-3 genes. Mol Immunol 37: 41–52
Zipfel PF, Jokiranta TS, Hellwage J, Koistinen V, Meri S 1999 The factor H protein family. Immunopharmacology 42: 53–60
Dragon-Durey MA, Frémeaux-Bacchi V, Loirat C, Blouin J, Niaudet P, Deschenes G, Coppo P, Herman Fridman W, Weiss L 2004 Heterozygous and homozygous factor H deficiencies associated with hemolytic uremic syndrome or membranoproliferative glomerulonephritis: report and genetic analysis of 16 cases. J Am Soc Nephrol 15: 787–795
Schwartz GJ, Haycock GB, Edelmann CM Jr, Spitzer A 1976 A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58: 259–263
Kristensen T, Tack BF 1986 Murine protein H is comprised of 20 repeating units, 61 amino acids in length. Proc Natl Acad Sci USA 83: 3963–3967
Atkinson JP, Liszewski MK, Richards A, Kavanagh D, Moulton EA 2005 Hemolytic uremic syndrome: an example of insufficient complement regulation on self-tissue. Ann N Y Acad Sci 1056: 144–152
Jokiranta TS, Cheng ZZ, Seeberger H, Jozsi M, Heinen S, Noris M, Remuzzi G, Ormsby R, Gordon DL, Meri S, Hellwage J, Zipfel PF 2005 Binding of complement factor H to endothelial cells is mediated by the carboxy-terminal glycosaminoglycan binding site. Am J Pathol 167: 1173–1181
Hellwage J, Jokiranta TS, Friese MA, Wolk TU, Kampen E, Zipfel PF, Meri S 2002 Complement C3b/C3d and cell surface polyanions are recognized by overlapping binding sites on the most carboxyl-terminal domain of complement factor H. J Immunol 169: 6935–6944
Kavanagh D, Richards A, Atkinson J 2008 Complement regulatory genes and hemolytic uremic syndromes. Annu Rev Med 59: 293–309
Józsi M, Heinen S, Hartmann A, Ostrowicz CW, Halbich S, Richter H, Kunert A, Licht C, Saunders RE, Perkins SJ, Zipfel PF, Skerka C 2006 Factor H and atypical hemolytic uremic syndrome: mutations in the C-terminus cause structural changes and defective recognition functions. J Am Soc Nephrol 17: 170–177
Vaziri-Sani F, Holmberg L, Sjöholm AG, Kristoffersson AC, Manea M, Fremeaux-Bacchi V, Fehrman-Ekholm I, Raafat R, Karpman D 2006 Phenotypic expression of factor H mutations in patients with atypical hemolytic uremic syndrome. Kidney Int 69: 981–988
Manuelian T, Hellwage J, Meri S, Caprioli J, Noris M, Heinen S, Jozsi M, Neumann HP, Remuzzi G, Zipfel PF 2003 Mutations in factor H reduce binding affinity to C3b and heparin and surface attachment to endothelial cells in hemolytic uremic syndrome. J Clin Invest 111: 1181–1190
Lupski JR, Stankiewicz P 2005 Genomic disorders: molecular mechanisms for rearrangements and conveyed phenotypes. PLoS Genet 1: e49
Heinen S, Sanchez-Corral P, Jackson MS, Strain L, Goodship JA, Kemp EJ, Skerka C, Jokiranta TS, Meyers K, Wagner E, Robitaille P, Esparza-Gordillo J, Rodriguez de Cordoba S, Zipfel PF, Goodship TH 2006 De novo gene conversion in the RCA gene cluster (1q32) causes mutations in complement factor H associated with atypical hemolytic uremic syndrome. Hum Mutat 27: 292–293.
Venables JP, Strain L, Routledge D, Bourn D, Powell HM, Warwicker P, Diaz-Torres ML, Sampson A, Mead P, Webb M, Pirson Y, Jackson MS, Hughes A, Wood KM, Goodship JA, Goodship TH 2006 Atypical haemolytic uraemic syndrome associated with a hybrid complement gene. PLoS Med 3: e431
Zipfel PF, Edey M, Heinen S, Józsi M, Richter H, Misselwitz J, Hoppe B, Routledge D, Strain L, Hughes AE, Goodship JA, Licht C, Goodship TH, Skerka C 2007 Deletion of complement factor H-related genes CFHR1 and CFHR3 is associated with atypical hemolytic uremic syndrome. PLoS Genet 3: e41
Coppo P, Bengoufa D, Veyradier A, Wolf M, Bussel A, Millot GA, Malot S, Heshmati F, Mira JP, Boulanger E, Galicier L, Durey-Dragon MA, Fremeaux-Bacchi V, Ramakers M, Pruna A, Bordessoule D, Gouilleux V, Scrobohaci ML, Vernant JP, Moreau D, Azoulay E, Schlemmer B, Guillevin L, Lassoued K 2004 Severe ADAMTS13 deficiency in adult idiopathic thrombotic microangiopathies defines a subset of patients characterized by various autoimmune manifestations, lower platelet count, and mild renal involvement. Medicine (Baltimore) 83: 233–244
Kwon T, Dragon-Durey M-A, Macher M-A, Baudouin V, Maisin A, Peuchmaur M, Fremeaux-Bacchi V, Loirat C 2008 Successful pre-transplant management of a patient with anti-factor H autoantibodies-associated haemolytic uraemic syndrome. Nephrol Dial Transplant 23: 2088–2090
Le Quintrec M, Zuber J, Noel LH, Thervet E, Frémeaux-Bacchi V, Fridman WH, Legendre C, Dragon-Durey MA 2009 Anti-factor H-auto-antibodies in a fifth renal transplant recipient with atypical hemolytic and uremic syndrome. Am J Transplant 9: 1223–1229
Author information
Authors and Affiliations
Additional information
Supported by a Grant A080588 from the Korea Healthcare technology R&D Project, Ministry for Health, Welfare and Family Affairs, Republic of Korea and a Grant 06-2008-192-9 from the Seoul National University Hospital.
Rights and permissions
About this article
Cite this article
Lee, B., Kwak, S., Shin, J. et al. Atypical Hemolytic Uremic Syndrome Associated With Complement Factor H Autoantibodies and CFHR1/CFHR3 Deficiency. Pediatr Res 66, 336–340 (2009). https://doi.org/10.1203/PDR.0b013e3181b1bd4a
Received:
Accepted:
Issue date:
DOI: https://doi.org/10.1203/PDR.0b013e3181b1bd4a
This article is cited by
-
Mutations in the alternative complement pathway in multiple myeloma patients with carfilzomib-induced thrombotic microangiopathy
Blood Cancer Journal (2023)
-
Genotypic analysis of a large cohort of patients with suspected atypical hemolytic uremic syndrome
Journal of Molecular Medicine (2023)
-
Systematic review of atypical hemolytic uremic syndrome biomarkers
Pediatric Nephrology (2022)
-
Deficiency of CFHR plasma proteins and autoantibody positive hemolytic uremic syndrome: treatment rationale, outcomes, and monitoring
Pediatric Nephrology (2021)
-
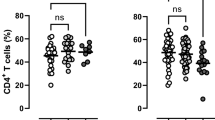
Altered Peripheral Blood Leucocyte Phenotype and Responses in Healthy Individuals with Homozygous Deletion of FHR1 and FHR3 Genes
Journal of Clinical Immunology (2019)