Abstract
Introduction:
Magnetic resonance imaging (MRI) and spectroscopy (MRS) have proven valuable in evaluating neonatal hypoxic–ischemic injury (HII).
Results:
MRI scores in the basal ganglia of HII/HT+ neonates were significantly lower than HII/HT− neonates, indicating less severe injury and were associated with lower discharge encephalopathy severity scores in the HII/HT+ group (P = 0.01). Lactate (Lac) was detected in the occipital gray matter (OGM) and thalamus (TH) of significantly more HII/HT− neonates (31.6 and 35.3%) as compared to the HII/HT+ group (10.5 and 15.8%). In contrast, the N-acetylaspartate (NAA)-based ratios in the OGM and TH did not differ between the HII groups.
Discussion:
Our data show that the HT was associated with a decrease in the number of HII neonates with detectable cortical and subcortical Lac as well as a decrease in the number of MRI-detectable subcortical lesions.
Methods:
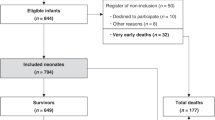
We retrospectively compared the medical and neuroimaging data of 19 HII neonates who received 72 h of whole-body cooling (HII/HT+) with those of 19 noncooled HII neonates (HII/HT−) to determine whether hypothermia was associated with improved recovery from the injury as measured by MRI and MRS within the first 14 days of life. MRI scores and metabolite ratios of HII/HT+ and HII/HT− neonates were also compared with nine healthy, nonasphyxiated “control” neonates.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Pin TW, Eldridge B, Galea MP . A review of developmental outcomes of term infants with post-asphyxia neonatal encephalopathy. Eur J Paediatr Neurol 2009;13:224–34.
Volpe JJ . Neurology of the Newborn. Philadelphia: WB Saunders, 2008: 331–41.
Shankaran S, Laptook AR, Ehrenkranz RA,et al.; National Institute of Child Health and Human Development Neonatal Research Network. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N Engl J Med 2005;353:1574–84.
Azzopardi DV, Strohm B, Edwards AD,et al.; TOBY Study Group. Moderate hypothermia to treat perinatal asphyxial encephalopathy. N Engl J Med 2009;361:1349–58.
de Vries LS, Jongmans MJ . Long-term outcome after neonatal hypoxic-ischaemic encephalopathy. Arch Dis Child Fetal Neonatal Ed 2010;95:F220–4.
Perlman M, Shah PS . Hypoxic-ischemic encephalopathy: challenges in outcome and prediction. J Pediatr 2011;158:e51–4.
Rutherford M, Pennock J, Schwieso J, Cowan F, Dubowitz L . Hypoxic-ischaemic encephalopathy: early and late magnetic resonance imaging findings in relation to outcome. Arch Dis Child Fetal Neonatal Ed 1996;75:F145–51.
Barkovich AJ, Hajnal BL, Vigneron D,et al. Prediction of neuromotor outcome in perinatal asphyxia: evaluation of MR scoring systems. AJNR Am J Neuroradiol 1998;19:143–9.
Rutherford M, Srinivasan L, Dyet L,et al. Magnetic resonance imaging in perinatal brain injury: clinical presentation, lesions and outcome. Pediatr Radiol 2006;36:582–92.
Ferriero DM, Miller SP . Imaging selective vulnerability in the developing nervous system. J Anat 2010;217:429–35.
Hanrahan JD, Sargentoni J, Azzopardi D,et al. Cerebral metabolism within 18 hours of birth asphyxia: a proton magnetic resonance spectroscopy study. Pediatr Res 1996;39:584–90.
Cady EB, Amess P, Penrice J, Wylezinska M, Sams V, Wyatt JS . Early cerebral-metabolite quantification in perinatal hypoxic-ischaemic encephalopathy by proton and phosphorus magnetic resonance spectroscopy. Magn Reson Imaging 1997;15:605–11.
Ashwal S, Holshouser BA, Tomasi LG,et al. 1H-magnetic resonance spectroscopy-determined cerebral lactate and poor neurological outcomes in children with central nervous system disease. Ann Neurol 1997;41:470–81.
Barkovich AJ, Baranski K, Vigneron D,et al. Proton MR spectroscopy for the evaluation of brain injury in asphyxiated, term neonates. AJNR Am J Neuroradiol 1999;20:1399–405.
Roelants-Van Rijn AM, van der Grond J, de Vries LS, Groenendaal F . Value of (1)H-MRS using different echo times in neonates with cerebral hypoxia-ischemia. Pediatr Res 2001;49:356–62.
Miller SP, Newton N, Ferriero DM,et al. Predictors of 30-month outcome after perinatal depression: role of proton MRS and socioeconomic factors. Pediatr Res 2002;52:71–7.
Inder TE, Hunt RW, Morley CJ,et al. Randomized trial of systemic hypothermia selectively protects the cortex on MRI in term hypoxic-ischemic encephalopathy. J Pediatr 2004;145:835–7.
Rutherford MA, Azzopardi D, Whitelaw A,et al. Mild hypothermia and the distribution of cerebral lesions in neonates with hypoxic-ischemic encephalopathy. Pediatrics 2005;116:1001–6.
Rutherford M, Ramenghi LA, Edwards AD,et al. Assessment of brain tissue injury after moderate hypothermia in neonates with hypoxic-ischaemic encephalopathy: a nested substudy of a randomised controlled trial. Lancet Neurol 2010;9:39–45.
Bonifacio SL, Glass HC, Vanderpluym J,et al. Perinatal events and early magnetic resonance imaging in therapeutic hypothermia. J Pediatr 2011;158:360–5.
Miller SP, Ramaswamy V, Michelson D,et al. Patterns of brain injury in term neonatal encephalopathy. J Pediatr 2005;146:453–60.
Shu SK, Ashwal S, Holshouser BA, Nystrom G, Hinshaw DB Jr . Prognostic value of 1H-MRS in perinatal CNS insults. Pediatr Neurol 1997;17:309–18.
Cady EB . Metabolite concentrations and relaxation in perinatal cerebral hypoxic-ischemic injury. Neurochem Res 1996;21:1043–52.
Barkovich AJ, Westmark KD, Bedi HS, Partridge JC, Ferriero DM, Vigneron DB . Proton spectroscopy and diffusion imaging on the first day of life after perinatal asphyxia: preliminary report. AJNR Am J Neuroradiol 2001;22:1786–94.
Amess PN, Penrice J, Wylezinska M,et al. Early brain proton magnetic resonance spectroscopy and neonatal neurology related to neurodevelopmental outcome at 1 year in term infants after presumed hypoxic-ischaemic brain injury. Dev Med Child Neurol 1999;41:436–45.
Provencher SW . Estimation of metabolite concentrations from localized in vivo proton NMR spectra. Magn Reson Med 1993;30:672–79.
Ashwal S, Holshouser BA, del Rio MJ, Tong KA, Applegate RL, Bailey LL . Serial proton magnetic resonance spectroscopy of the brain in children undergoing cardiac surgery. Pediatr Neurol 2003;29:99–110.
Angeles DM, Ashwal S, Wycliffe ND,et al. Relationship between opioid therapy, tissue-damaging procedures, and brain metabolites as measured by proton MRS in asphyxiated term neonates. Pediatr Res 2007;61:614–21.
Massaro AN, Kadom N, Chang T, Glass P, Nelson K, Baumgart S . Quantitative analysis of magnetic resonance images and neurological outcome in encephalopathic neonates treated with whole-body hypothermia. J Perinatol 2010;30:596–603.
Sarnat HB, Sarnat MS . Neonatal encephalopathy following fetal distress. A clinical and electroencephalographic study. Arch Neurol 1976;33:696–705.
Panigrahy A, Blüml S . Advances in magnetic resonance neuroimaging techniques in the evaluation of neonatal encephalopathy. Top Magn Reson Imaging 2007;18:3–29.
Panigrahy A, Nelson MD Jr, Blüml S . Magnetic resonance spectroscopy in pediatric neuroradiology: clinical and research applications. Pediatr Radiol 2010;40:3–30.
Obenaus A, Ashwal S . Magnetic resonance imaging in cerebral ischemia: focus on neonates. Neuropharmacology 2008;55:271–80.
Azzopardi D, Edwards AD . Magnetic resonance biomarkers of neuroprotective effects in infants with hypoxic ischemic encephalopathy. Semin Fetal Neonatal Med 2010;15:261–9.
Miller SP, Latal B, Clark H,et al. Clinical signs predict 30-month neurodevelopmental outcome after neonatal encephalopathy. Am J Obstet Gynecol 2004;190:93–9.
Groenendaal F, Veenhoven RH, van der Grond J, Jansen GH, Witkamp TD, de Vries LS . Cerebral lactate and N-acetyl-aspartate/choline ratios in asphyxiated full-term neonates demonstrated in vivo using proton magnetic resonance spectroscopy. Pediatr Res 1994;35:148–51.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Corbo, E., Bartnik-Olson, B., Machado, S. et al. The effect of whole-body cooling on brain metabolism following perinatal hypoxic–ischemic injury. Pediatr Res 71, 85–92 (2012). https://doi.org/10.1038/pr.2011.8
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2011.8
This article is cited by
-
Glucose and Intermediary Metabolism and Astrocyte–Neuron Interactions Following Neonatal Hypoxia–Ischemia in Rat
Neurochemical Research (2017)
-
MR spectroscopy in children: protocols and pitfalls in non-tumorous brain pathology
Pediatric Radiology (2016)
-
Peut-on établir un pronostic neurologique à la sortie de la néonatalogie pour les encéphalopathies anoxo-ischémiques du nouveau-né à terme ?
Revue de médecine périnatale (2013)
-
Hypothermie pour la neuroprotection cérébrale de l’encéphalopathie anoxo-ischémique: certitudes et incertitudes
Revue de médecine périnatale (2013)