Abstract
Background:
Risk factors for diastolic dysfunction in hypertrophic cardiomyopathy (HCM) are poorly understood. We investigated the association of variants in hypoxia-response genes with phenotype severity in pediatric HCM.
Methods:
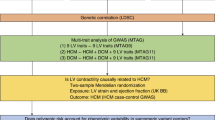
A total of 80 unrelated patients <21 y and 14 related members from eight families with HCM were genotyped for six variants associated with vascular endothelial growth factor A (VEGFA) downregulation, or hypoxia-inducible factor A (HIF1A) upregulation. Associations between risk genotypes and left-ventricular (LV) hypertrophy, LV dysfunction, and freedom from myectomy were assessed. Tissue expression was measured in myocardial samples from 17 patients with HCM and 20 patients without HCM.
Results:
Age at enrollment was 9 ± 5 y (follow-up, 3.1 ± 3.6 y). Risk allele frequency was 67% VEGFA and 92% HIF1A. Risk genotypes were associated with younger age at diagnosis (P < 0.001), septal hypertrophy (P < 0.01), prolonged E-wave deceleration time (EWDT) (P < 0.0001) and isovolumic relaxation time (IVRT) (P < 0.0001), and lower freedom from myectomy (P < 0.05). These associations were seen in sporadic and familial HCM independent of the disease-causing mutation. Risk genotypes were associated with higher myocardial HIF1A and transforming growth factor B1 (TGFB1) expression and increased endothelial-fibroblast transformation (P < 0.05).
Conclusion:
HIF1A-upregulation and/or VEGFA-downregulation genotypes were associated with more severe septal hypertrophy and diastolic dysfunction and may provide genetic markers to improve risk prediction in HCM.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Maron BJ, Pelliccia A, Spirito P . Cardiac disease in young trained athletes. Insights into methods for distinguishing athlete’s heart from structural heart disease, with particular emphasis on hypertrophic cardiomyopathy. Circulation 1995;91:1596–601.
Schwartzkopff B, Mundhenke M, Strauer BE . Alterations of the architecture of subendocardial arterioles in patients with hypertrophic cardiomyopathy and impaired coronary vasodilator reserve: a possible cause for myocardial ischemia. J Am Coll Cardiol 1998;31:1089–96.
Kofflard MJ, Michels M, Krams R, et al. Coronary flow reserve in hypertrophic cardiomyopathy: relation with microvascular dysfunction and pathophysiological characteristics. Neth Heart J 2007;15:209–15.
Johansson B, Mörner S, Waldenström A, Stål P . Myocardial capillary supply is limited in hypertrophic cardiomyopathy: a morphological analysis. Int J Cardiol 2008;126:252–7.
Takemura G, Takatsu Y, Fujiwara H . Luminal narrowing of coronary capillaries in human hypertrophic hearts: an ultrastructural morphometrical study using endomyocardial biopsy specimens. Heart 1998;79:78–85.
Bruder O, Wagner A, Jensen CJ, et al. Myocardial scar visualized by cardiovascular magnetic resonance imaging predicts major adverse events in patients with hypertrophic cardiomyopathy. J Am Coll Cardiol 2010;56:875–87.
O’Hanlon R, Grasso A, Roughton M, et al. Prognostic significance of myocardial fibrosis in hypertrophic cardiomyopathy. J Am Coll Cardiol 2010;56:867–74.
Ho CY, López B, Coelho-Filho OR, et al. Myocardial fibrosis as an early manifestation of hypertrophic cardiomyopathy. N Engl J Med 2010;363:552–63.
Wang GL, Jiang BH, Rue EA, Semenza GL . Hypoxia-inducible factor 1 is a basic-helix-loop-helix-PAS heterodimer regulated by cellular O2 tension. Proc Natl Acad Sci USA 1995;92:5510–4.
Rey S, Semenza GL . Hypoxia-inducible factor-1-dependent mechanisms of vascularization and vascular remodelling. Cardiovasc Res 2010;86:236–42.
Halberg N, Khan T, Trujillo ME, et al. Hypoxia-inducible factor 1alpha induces fibrosis and insulin resistance in white adipose tissue. Mol Cell Biol 2009;29:4467–83.
Kimura K, Iwano M, Higgins DF, et al. Stable expression of HIF-1alpha in tubular epithelial cells promotes interstitial fibrosis. Am J Physiol Renal Physiol 2008;295:F1023–9.
Moon JO, Welch TP, Gonzalez FJ, Copple BL . Reduced liver fibrosis in hypoxia-inducible factor-1alpha-deficient mice. Am J Physiol Gastrointest Liver Physiol 2009;296:G582–92.
Zeisberg EM, Tarnavski O, Zeisberg M, et al. Endothelial-to-mesenchymal transition contributes to cardiac fibrosis. Nat Med 2007;13:952–61.
Teekakirikul P, Eminaga S, Toka O, et al. Cardiac fibrosis in mice with hypertrophic cardiomyopathy is mediated by non-myocyte proliferation and requires Tgf-β. J Clin Invest 2010;120:3520–9.
Zheng ZL, Hwang YH, Kim SK, et al. Genetic polymorphisms of hypoxia-inducible factor-1 alpha and cardiovascular disease in hemodialysis patients. Nephron Clin Pract 2009;113:c104–11.
van der Meer P, De Boer RA, White HL, et al. The VEGF +405 CC promoter polymorphism is associated with an impaired prognosis in patients with chronic heart failure: a MERIT-HF substudy. J Card Fail 2005;11:279–84.
Hsieh YY, Wang JP, Lin CS . Four novel single nucleotide polymorphisms within the promoter region of p53 gene and their associations with uterine leiomyoma. Mol Reprod Dev 2007;74:815–20.
Foster BJ, Mackie AS, Mitsnefes M, Ali H, Mamber S, Colan SD . A novel method of expressing left ventricular mass relative to body size in children. Circulation 2008;117:2769–75.
Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 2005;18:1440–63.
Ackerman MJ . Genetic testing for risk stratification in hypertrophic cardiomyopathy and long QT syndrome: fact or fiction? Curr Opin Cardiol 2005;20:175–81.
Friehs I, Barillas R, Vasilyev NV, Roy N, McGowan FX, del Nido PJ . Vascular endothelial growth factor prevents apoptosis and preserves contractile function in hypertrophied infant heart. Circulation 2006;114:Suppl 1:I290–5.
Friehs I, Margossian RE, Moran AM, Cao-Danh H, Moses MA, del Nido PJ . Vascular endothelial growth factor delays onset of failure in pressure-overload hypertrophy through matrix metalloproteinase activation and angiogenesis. Basic Res Cardiol 2006;101:204–13.
Sano M, Minamino T, Toko H, et al. p53-induced inhibition of Hif-1 causes cardiac dysfunction during pressure overload. Nature 2007;446:444–8.
Maron BJ, Spirito P, Green KJ, Wesley YE, Bonow RO, Arce J . Noninvasive assessment of left ventricular diastolic function by pulsed Doppler echocardiography in patients with hypertrophic cardiomyopathy. J Am Coll Cardiol 1987;10:733–42.
Gidding SS, Snider AR, Rocchini AP, Peters J, Farnsworth R . Left ventricular diastolic filling in children with hypertrophic cardiomyopathy: assessment with pulsed Doppler echocardiography. J Am Coll Cardiol 1986;8:310–6.
Matsumura Y, Elliott PM, Virdee MS, Sorajja P, Doi Y, McKenna WJ . Left ventricular diastolic function assessed using Doppler tissue imaging in patients with hypertrophic cardiomyopathy: relation to symptoms and exercise capacity. Heart 2002;87:247–51.
McMahon CJ, Nagueh SF, Pignatelli RH, et al. Characterization of left ventricular diastolic function by tissue Doppler imaging and clinical status in children with hypertrophic cardiomyopathy. Circulation 2004;109:1756–62.
Geske JB, Sorajja P, Nishimura RA, Ommen SR . Evaluation of left ventricular filling pressures by Doppler echocardiography in patients with hypertrophic cardiomyopathy: correlation with direct left atrial pressure measurement at cardiac catheterization. Circulation 2007;116:2702–8.
Nagueh SF, Lakkis NM, Middleton KJ, Spencer WH 3rd, Zoghbi WA, Quiñones MA . Doppler estimation of left ventricular filling pressures in patients with hypertrophic cardiomyopathy. Circulation 1999;99:254–61.
Leask A . Potential therapeutic targets for cardiac fibrosis: TGFbeta, angiotensin, endothelin, CCN2, and PDGF, partners in fibroblast activation. Circ Res 2010;106:1675–80.
Eisenberg LM, Markwald RR . Molecular regulation of atrioventricular valvuloseptal morphogenesis. Circ Res 1995;77:1–6.
Broberg CS, Chugh SS, Conklin C, Sahn DJ, Jerosch-Herold M . Quantification of diffuse myocardial fibrosis and its association with myocardial dysfunction in congenital heart disease. Circ Cardiovasc Imaging 2010;3:727–34.
Coats AJ, Shewan LG . Statement on authorship and publishing ethics in the International Journal of Cardiology. Int J Cardiol 2011;153:239–40.
Kaufman BD, Auerbach S, Reddy S, et al. RAAS gene polymorphisms influence progression of pediatric hypertrophic cardiomyopathy. Hum Genet 2007;122:515–23.
O’Leary PW, Durongpisitkul K, Cordes TM, et al. Diastolic ventricular function in children: a Doppler echocardiographic study establishing normal values and predictors of increased ventricular end-diastolic pressure. Mayo Clin Proc 1998;73:616–28.
Eidem BW, McMahon CJ, Cohen RR, et al. Impact of cardiac growth on Doppler tissue imaging velocities: a study in healthy children. J Am Soc Echocardiogr 2004;17:212–21.
Breunis WB, Biezeveld MH, Geissler J, et al. Vascular endothelial growth factor gene haplotypes in Kawasaki disease. Arthritis Rheum 2006;54:1588–94.
Buraczynska M, Ksiazek P, Baranowicz-Gaszczyk I, Jozwiak L . Association of the VEGF gene polymorphism with diabetic retinopathy in type 2 diabetes patients. Nephrol Dial Transplant 2007;22:827–32.
Hlatky MA, Quertermous T, Boothroyd DB, et al. Polymorphisms in hypoxia inducible factor 1 and the initial clinical presentation of coronary disease. Am Heart J 2007;154:1035–42.
Howell WM, Ali S, Rose-Zerilli MJ, Ye S . VEGF polymorphisms and severity of atherosclerosis. J Med Genet 2005;42:485–90.
Pan D, Li Q, Jiang N, Liu A, Yu K . Robust joint analysis allowing for model uncertainty in two-stage genetic association studies. BMC Bioinformatics 2011;12:9.
Thomas DC, Casey G, Conti DV, Haile RW, Lewinger JP, Stram DO . Methodological Issues in Multistage Genome-wide Association Studies. Stat Sci 2009;24:414–29.
Acknowledgements
We acknowledge the Labatt Family Heart Centre Biobank for access to DNA and tissue samples, and The Centre for Applied Genomics (www.tcag.ca/) for genotyping of candidate SNPs.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alkon, J., Friedberg, M., Manlhiot, C. et al. Genetic variations in hypoxia response genes influence hypertrophic cardiomyopathy phenotype. Pediatr Res 72, 583–592 (2012). https://doi.org/10.1038/pr.2012.126
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2012.126
This article is cited by
-
Association between genetic variants in the HIF1A-VEGF pathway and left ventricular regional myocardial deformation in patients with hypertrophic cardiomyopathy
Pediatric Research (2021)
-
Coronary arterial vasculature in the pathophysiology of hypertrophic cardiomyopathy
Pflügers Archiv - European Journal of Physiology (2019)
-
Serum Biomarkers of Myocardial Remodeling and Coronary Dysfunction in Early Stages of Hypertrophic Cardiomyopathy in the Young
Pediatric Cardiology (2017)
-
Focal myocardial fibrosis assessed by late gadolinium enhancement cardiovascular magnetic resonance in children and adolescents with dilated cardiomyopathy
Journal of Cardiovascular Magnetic Resonance (2015)