Abstract
Background:
Reintroduction of enteral nutrition in neonates with necrotizing enterocolitis (NEC) should take place when the gut is ready for its normal function. Too early a start of oral feeding might lead to disease relapse, whereas prolonged discontinuation of enteral nutrition is associated with impaired gut function and parenteral nutrition–related complications. This study evaluated whether noninvasive urinary measurement of intestinal fatty acid binding protein (I-FABP) at the time of refeeding can predict clinical outcome in neonates with NEC.
Methods:
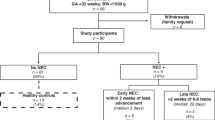
Urinary I-FABP concentrations were measured in 21 infants with NEC just before reintroducing enteral nutrition. Poor outcome was defined as unsuccessful reintroduction of enteral feeding (EF), (re)operation for NEC, or death related to NEC after reintroduction of EF.
Results:
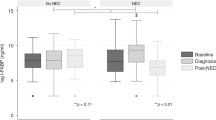
Median urinary I-FABP levels in neonates with poor outcome (n = 5) were significantly higher as compared with I-FABP levels in neonates with good outcome (n = 16) (P < 0.01). A clinically significant cutoff value of 963 pg/ml was found to discriminate between infants with poor outcome and those with good outcome (sensitivity 80%, specificity 94%).
Conclusion:
Noninvasive urinary I-FABP measurement at time of refeeding differentiates neonates with poor outcome from neonates with good outcome in NEC. Urinary I-FABP measurement may therefore be helpful in the timing of EF in neonates with NEC.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Lin PW, Stoll BJ . Necrotising enterocolitis. Lancet 2006;368:1271–83.
Bell MJ, Ternberg JL, Feigin RD, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg 1978;187:1–7.
Neu J . Neonatal necrotizing enterocolitis: an update. Acta Paediatr Suppl 2005;94:100–5.
Lee JS, Polin RA . Treatment and prevention of necrotizing enterocolitis. Semin Neonatol 2003;8:449–59.
Berseth CL . Feeding strategies and necrotizing enterocolitis. Curr Opin Pediatr 2005;17:170–3.
Lin PW, Nasr TR, Stoll BJ . Necrotizing enterocolitis: recent scientific advances in pathophysiology and prevention. Semin Perinatol 2008;32:70–82.
Bohnhorst B, Müller S, Dördelmann M, Peter CS, Petersen C, Poets CF . Early feeding after necrotizing enterocolitis in preterm infants. J Pediatr 2003;143:484–7.
Thuijls G, Derikx JP, van Wijck K, et al. Non-invasive markers for early diagnosis and determination of the severity of necrotizing enterocolitis. Ann Surg 2010;251:1174–80.
Veerkamp JH, Paulussen RJ, Peeters RA, Maatman RG, van Moerkerk HT, van Kuppevelt TH . Detection, tissue distribution and (sub)cellular localization of fatty acid-binding protein types. Mol Cell Biochem 1990;98:11–8.
van de Poll MC, Derikx JP, Buurman WA, et al. Liver manipulation causes hepatocyte injury and precedes systemic inflammation in patients undergoing liver resection. World J Surg 2007;31:2033–8.
Evennett NJ, Hall NJ, Pierro A, Eaton S . Urinary intestinal fatty acid-binding protein concentration predicts extent of disease in necrotizing enterocolitis. J Pediatr Surg 2010;45:735–40.
Morgan J, Young L, McGuire W . Delayed introduction of progressive enteral feeds to prevent necrotising enterocolitis in very low birth weight infants. Cochrane Database Syst Rev 2011:CD001970.
Morgan J, Young L, McGuire W . Slow advancement of enteral feed volumes to prevent necrotising enterocolitis in very low birth weight infants. Cochrane Database Syst Rev 2011:CD001241.
Neu J, Walker WA . Necrotizing enterocolitis. N Engl J Med 2011;364:255–64.
Kliegman RM, Walker WA, Yolken RH . Necrotizing enterocolitis: research agenda for a disease of unknown etiology and pathogenesis. Pediatr Res 1993;34:701–8.
Oste M, Van Haver E, Thymann T, Sangild P, Weyns A, Van Ginneken CJ . Formula induces intestinal apoptosis in preterm pigs within a few hours of feeding. JPEN J Parenter Enteral Nutr 2010;34:271–9.
Derikx JP, Blijlevens NM, Donnelly JP, et al. Loss of enterocyte mass is accompanied by diminished turnover of enterocytes after myeloablative therapy in haematopoietic stem-cell transplant recipients. Ann Oncol 2009;20:337–42.
Bossuyt PM, Reitsma JB, Bruns DE, et al. The STARD statement for reporting studies of diagnostic accuracy: explanation and elaboration. Clin Chem 2003;49:7–18.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Reisinger, K., Derikx, J., Thuijls, G. et al. Noninvasive measurement of intestinal epithelial damage at time of refeeding can predict clinical outcome after necrotizing enterocolitis. Pediatr Res 73, 209–213 (2013). https://doi.org/10.1038/pr.2012.160
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2012.160
This article is cited by
-
Predicting intestinal recovery after necrotizing enterocolitis in preterm infants
Pediatric Research (2020)
-
Intra-amniotic Candida albicans infection induces mucosal injury and inflammation in the ovine fetal intestine
Scientific Reports (2016)
-
Clinical significance of FABP2 expression in newborns with necrotizing enterocolitis
World Journal of Pediatrics (2016)
-
Urine biomarkers for necrotizing enterocolitis
Pediatric Surgery International (2015)
-
Intestinal permeability – a new target for disease prevention and therapy
BMC Gastroenterology (2014)