Abstract
Background:
The aim of this study was to determine whether small-for-gestational-age (SGA) infants born very prematurely had increased respiratory morbidity in the neonatal period and at follow-up.
Methods:
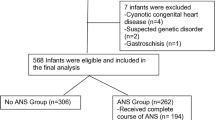
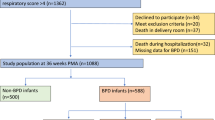
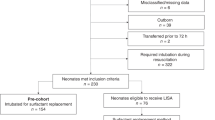
Data were examined from infants recruited into the United Kingdom Oscillation Study (UKOS). Of the 797 infants who were born at <29 wk of gestational age, 174 infants were SGA. Overall, 92% were exposed to antenatal corticosteroids and 97% received surfactant; follow-up data at 22–28 mo were available for 367 infants.
Results:
After adjustment for gestational age and sex, SGA infants had higher rates of supplementary oxygen dependency at 36 wk postmenstrual age (odds ratio (OR): 3.23; 95% confidence interval: 2.03, 5.13), pulmonary hemorrhage (OR: 3.07; 95% CI: 1.82, 5.18), death (OR: 3.32; 95% CI: 2.13, 5.17), and postnatal corticosteroid requirement (OR: 2.09; 95% CI: 1.35, 3.23). After adjustment for infant and respiratory morbidity risk factors, a lower mean birth weight z-score was associated with a higher prevalence of respiratory admissions (OR: 1.40; 95% CI: 1.03, 1.88 for 1 SD change in z-score), cough (OR: 1.28; 95% CI: 1.00, 1.65), and use of chest medicines (OR: 1.32; 95% CI: 1.01, 1.73).
Conclusion:
SGA infants who were born very prematurely, despite routine use of antenatal corticosteroids and postnatal surfactant, had increased respiratory morbidity at follow-up, which was not due to poor neonatal outcome.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Ferdynus C, Quantin C, Abrahamowicz M, et al. Can birth weight standards based on healthy populations improve the identification of small-for-gestational-age newborns at risk of adverse neonatal outcomes? Pediatrics 2009;123:723–30.
Yu HJ, Kim ES, Kim JK, et al. Outcomes of small for gestational age micropremies depending on how young or how small they are. Korean J Pediatr 2011;54:246–52.
Gluck L, Kulovich MV . Lecithin-sphingomyelin ratios in amniotic fluid in normal and abnormal pregnancy. Am J Obstet Gynecol 1973;115:539–46.
Procianoy RS, Garcia-Prats JA, Adams JM, Silvers A, Rudolph AJ . Hyaline membrane disease and intraventricular haemorrhage in small for gestational age infants. Arch Dis Child 1980;55:502–5.
Piper JM, Langer O . Is lung maturation related to fetal growth in diabetic or hypertensive pregnancies? Eur J Obstet Gynecol Reprod Biol 1993;51:15–9.
Ruys-Dudok van Heel I, de Leeuw R . Clinical outcome of small for gestational age preterm infants. J Perinat Med 1989;17:77–83.
Thompson PJ, Greenough A, Gamsu HR, Nicolaides KH . Ventilatory requirements for respiratory distress syndrome in small-for-gestational-age infants. Eur J Pediatr 1992;151:528–31.
Henderson-Smart DJ . Postnatal consequences of chronic intrauterine compromise. Reprod Fertil Dev 1995;7:559–65.
Piper JM, Xenakis EM, McFarland M, Elliott BD, Berkus MD, Langer O . Do growth-retarded premature infants have different rates of perinatal morbidity and mortality than appropriately grown premature infants? Obstet Gynecol 1996;87:169–74.
Fleischer A, Anyaegbunam A, Guidetti D, Randolph G, Merkatz IR . A persistent clinical problem: profile of the term infant with significant respiratory complications. Obstet Gynecol 1992;79:185–90.
Tyson JE, Kennedy K, Broyles S, Rosenfeld CR . The small for gestational age infant: accelerated or delayed pulmonary maturation? Increased or decreased survival? Pediatrics 1995;95:534–8.
Sharma P, McKay K, Rosenkrantz TS, Hussain N . Comparisons of mortality and pre-discharge respiratory outcomes in small-for-gestational-age and appropriate-for-gestational-age premature infants. BMC Pediatr 2004;4:9.
Regev RH, Lusky A, Dolfin T, Litmanovitz I, Arnon S, Reichman B; Israel Neonatal Network. Excess mortality and morbidity among small-for-gestational-age premature infants: a population-based study. J Pediatr 2003;143:186–91.
Bernstein IM, Horbar JD, Badger GJ, Ohlsson A, Golan A . Morbidity and mortality among very-low-birth-weight neonates with intrauterine growth restriction. The Vermont Oxford Network. Am J Obstet Gynecol 2000;182(1 Pt 1):198–206.
Zeitlin J, El Ayoubi M, Jarreau PH, et al.; MOSAIC Research Group. Impact of fetal growth restriction on mortality and morbidity in a very preterm birth cohort. J Pediatr 2010;157:733–9.e1.
Costeloe K, Hennessy E, Gibson AT, Marlow N, Wilkinson AR . The EPICure study: outcomes to discharge from hospital for infants born at the threshold of viability. Pediatrics 2000;106:659–71.
Field DJ, Dorling JS, Manktelow BN, Draper ES . Survival of extremely premature babies in a geographically defined population: prospective cohort study of 1994-9 compared with 2000-5. BMJ 2008;336:1221–3.
Stewart A, Brion LP, Soll R . Diuretics for respiratory distress syndrome in preterm infants. Cochrane Database Syst Rev 2011:CD001454.
Shah SS, Ohlsson A, Halliday H, Shah VS . Inhaled versus systemic corticosteroids for the treatment of chronic lung disease in ventilated very low birth weight preterm infants. Cochrane Database Syst Rev 2007:CD002057.
Walsh MC, Yao Q, Gettner P, et al.; National Institute of Child Health and Human Development Neonatal Research Network. Impact of a physiologic definition on bronchopulmonary dysplasia rates. Pediatrics 2004;114:1305–11.
Kinali M, Greenough A, Dimitriou G, Yüksel B, Hooper R . Chronic respiratory morbidity following premature delivery–prediction by prolonged respiratory support requirement? Eur J Pediatr 1999;158:493–6.
Jobe AH, Bancalari E . Bronchopulmonary dysplasia. Am J Respir Crit Care Med 2001;163:1723–9.
Ehrenkranz RA, Walsh MC, Vohr BR, et al.; National Institutes of Child Health and Human Development Neonatal Research Network. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics 2005;116:1353–60.
Jobe AH . Antenatal factors and the development of bronchopulmonary dysplasia. Semin Neonatol 2003;8:9–17.
Crowley P . Antenatal corticosteroid therapy: a metanalysis of the randomized trials 1972-1994. Am J Obstet Gynecol 1995;173:322–35.
Elimian A, Verma U, Beneck D, et al. Histologic chorioamnionitis, antenatal steroids and perinatal outcomes. Obstet Gynecol 2000;96:333–6.
Harding JE, Pang J, Knight DB, Liggins GC . Do antenatal corticosteroids help in the setting of preterm rupture of membranes? Am J Obstet Gynecol 2001;184:131–9.
Kallapur SG, Kramer BW, Moss TJ, et al. Maternal glucocorticoids increase endotoxin-induced lung inflammation in preterm lambs. Am J Physiol Lung Cell Mol Physiol 2003;284:L633–42.
Cole TJ, Freeman JV, Preece MA . British 1990 growth reference centiles for weight, height, body mass index and head circumference fitted by maximum penalized likelihood. Stat Med 1998;17:407–29.
Olsen IE, Groveman SA, Lawson ML, Clark RH, Zemel BS . New intrauterine growth curves based on United States data. Pediatrics 2010;125:e214–24.
Johnson AH, Peacock JL, Greenough A, et al.; United Kingdom Oscillation Study Group. High frequency oscillatory ventilation for the prevention of chronic lung disease of prematurity. N Engl J Med 2002;347:633–42.
Marlow N, Greenough A, Peacock JL, et al. Randomised trial of high frequency oscillatory ventilation or conventional ventilation in babies of gestational age 28 weeks or less: respiratory and neurological outcomes at 2 years. Arch Dis Child Fetal Neonatal Ed 2006;91:F320–6.
Harding R, Cock ML, Louey S, et al. The compromised intra-uterine environment: implications for future lung health. Clin Exp Pharmacol Physiol 2000;27:965–74.
Maritz GS, Morley CJ, Harding R . Early developmental origins of impaired lung structure and function. Early Hum Dev 2005;81:763–71.
Maritz GS, Cock ML, Louey S, Suzuki K, Harding R . Fetal growth restriction has long-term effects on postnatal lung structure in sheep. Pediatr Res 2004;55:287–95.
Karadag A, Sakurai R, Wang Y, et al. Effect of maternal food restriction on fetal rat lung lipid differentiation program. Pediatr Pulmonol 2009;44:635–44.
Morsing E, Gustafsson P, Brodszki J . Lung function in children born after foetal growth restriction and very preterm birth. Acta Paediatr 2012;101:48–54.
Altman DG, Royston P . The cost of dichotomising continuous variables. BMJ 2006;332:1080.
Peacock JL, Marston L, Marlow N, Calvert SA, Greenough A . Neonatal and infant outcome in boys and girls born very prematurely. Pediatr Res 2012;71:305–10.
Marston L, Peacock JL, Yu K, et al. Comparing methods of analysing datasets with small clusters – case studies using four paediatric datasets. Paediatr Perinatal Epidemiol 2009;23:380–92.
Author information
Authors and Affiliations
Corresponding author
Supplementary information
Supplementary Table S1
(DOC 30 kb)
Supplementary Table S2
(DOC 28 kb)
Rights and permissions
About this article
Cite this article
Peacock, J., Lo, J., D’Costa, W. et al. Respiratory morbidity at follow-up of small-for-gestational-age infants born very prematurely. Pediatr Res 73, 457–463 (2013). https://doi.org/10.1038/pr.2012.201
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2012.201
This article is cited by
-
Childhood outcomes following discharge from a referral bronchopulmonary dysplasia program
Journal of Perinatology (2024)
-
Fetal Growth Restriction in Hypertensive vs. Heavy Smoking Women—Placental Pathology, Ultrasound Findings, and Pregnancy Outcomes
Reproductive Sciences (2021)
-
Prematurity and the burden of influenza and respiratory syncytial virus disease
World Journal of Pediatrics (2016)