Abstract
Background:
Optimization of cerebral oxygenation after pediatric cardiac arrest (CA) may reduce neurological damage associated with the post-CA syndrome. We hypothesized that important alterations in regional partial pressure of brain tissue oxygen (PbO2) occur after resuscitation from CA and that clinically relevant interventions such as hyperoxia and blood pressure augmentation would influence PbO2.
Methods:
Cortical and thalamic PbO2 were monitored in immature rats subjected to asphyxial CA (9 or 12 min asphyxia) and sham-operated rats using oxygen sensors.
Results:
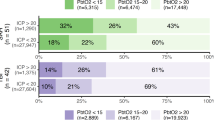
Thalamus and cortex showed similar baseline PbO2. Postresuscitation, there was early and sustained cortical hypoxia in an insult-duration dependent fashion. In contrast, thalamic PbO2 initially increased fourfold and afterwards returned to baseline values. PbO2 level was dependent on the fraction of inspired O2, and the response to oxygen was more pronounced after a 9 vs. 12 min CA. After a 12 min CA, PbO2 was modestly affected by blood pressure augmentation using epinephrine in the thalamus but not in the cortex.
Conclusion:
After asphyxial pediatric CA, there is marked regional variability of cerebral oxygenation. Cortical hypoxia is pronounced and appears early, whereas thalamic hyperoxia is followed by normoxia. Compromised PbO2 in the cortex may represent a relevant and clinically measurable therapeutic target aimed at improving neurological outcome after pediatric CA.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Moler FW, Meert K, Donaldson AE, et al.; Pediatric Emergency Care Applied Research Network. In-hospital versus out-of-hospital pediatric cardiac arrest: a multicenter cohort study. Crit Care Med 2009;37:2259–67.
Nolan JP, Neumar RW, Adrie C, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A Scientific Statement from the International Liaison Committee on Resuscitation; the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; the Council on Stroke. Resuscitation 2008;79:350–79.
Manole MD, Foley LM, Hitchens TK, et al. Magnetic resonance imaging assessment of regional cerebral blood flow after asphyxial cardiac arrest in immature rats. J Cereb Blood Flow Metab 2009;29:197–205.
Stiefel MF, Udoetuk JD, Storm PB, et al. Brain tissue oxygen monitoring in pediatric patients with severe traumatic brain injury. J Neurosurg 2006;105:Suppl:281–6.
Narotam PK, Morrison JF, Nathoo N . Brain tissue oxygen monitoring in traumatic brain injury and major trauma: outcome analysis of a brain tissue oxygen-directed therapy. J Neurosurg 2009;111:672–82.
McCarthy MC, Moncrief H, Sands JM, et al. Neurologic outcomes with cerebral oxygen monitoring in traumatic brain injury. Surgery 2009;146:585–90; discussion 590–1.
Lang EW, Mulvey JM, Mudaliar Y, Dorsch NW . Direct cerebral oxygenation monitoring–a systematic review of recent publications. Neurosurg Rev 2007;30:99–106; discussion 106–7.
Maloney-Wilensky E, Gracias V, Itkin A, et al. Brain tissue oxygen and outcome after severe traumatic brain injury: a systematic review. Crit Care Med 2009;37:2057–63.
Vespa PM . The implications of cerebral ischemia and metabolic dysfunction for treatment strategies in neurointensive care. Curr Opin Crit Care 2006;12:119–23.
Maloney-Wilensky E, Le Roux P . The physiology behind direct brain oxygen monitors and practical aspects of their use. Childs Nerv Syst 2010;26:419–30.
Goodman JC, Valadka AB, Gopinath SP, Uzura M, Robertson CS . Extracellular lactate and glucose alterations in the brain after head injury measured by microdialysis. Crit Care Med 1999;27:1965–73.
Kiening KL, Unterberg AW, Bardt TF, Schneider GH, Lanksch WR . Monitoring of cerebral oxygenation in patients with severe head injuries: brain tissue PO2 versus jugular vein oxygen saturation. J Neurosurg 1996;85:751–7.
Nordmark J, Rubertsson S, Mörtberg E, Nilsson P, Enblad P . Intracerebral monitoring in comatose patients treated with hypothermia after a cardiac arrest. Acta Anaesthesiol Scand 2009;53:289–98.
Bauer R, Gabl M, Obwegeser A, Galiano K, Barbach J, Mohsenipour I . Neurochemical monitoring using intracerebral microdialysis during cardiac resuscitation. Intensive Care Med 2004;30:159–61.
Nemoto EM, Erdmann W, Strong E, Rao GR, Moossy J . Regional brain PO2 after global ischemia in monkeys: evidence for regional differences in critical perfusion pressures. Stroke 1979;10:44–52.
Linner R, Werner O, Perez-de-Sa V, Cunha-Goncalves D . Circulatory recovery is as fast with air ventilation as with 100% oxygen after asphyxia-induced cardiac arrest in piglets. Pediatr Res 2009;66:391–4.
Farber NE, Harkin CP, Niedfeldt J, Hudetz AG, Kampine JP, Schmeling WT . Region-specific and agent-specific dilation of intracerebral microvessels by volatile anesthetics in rat brain slices. Anesthesiology 1997;87:1191–8.
Hansen TD, Warner DS, Todd MM, Vust LJ, Trawick DC . Distribution of cerebral blood flow during halothane versus isoflurane anesthesia in rats. Anesthesiology 1988;69:332–7.
Hendrich KS, Kochanek PM, Melick JA, et al. Cerebral perfusion during anesthesia with fentanyl, isoflurane, or pentobarbital in normal rats studied by arterial spin-labeled MRI. Magn Reson Med 2001;46:202–6.
Loeb AL, Raj NR, Longnecker DE . Cerebellar nitric oxide is increased during isoflurane anesthesia compared to halothane anesthesia: a microdialysis study in rats. Anesthesiology 1998;89:723–30.
Lowry JP, Boutelle MG, Fillenz M . Measurement of brain tissue oxygen at a carbon past electrode can serve as an index of increases in regional cerebral blood flow. J Neurosci Methods 1997;71:177–82.
Rossi S, Balestreri M, Spagnoli D, et al. Oxygen delivery and oxygen tension in cerebral tissue during global cerebral ischaemia: a swine model. Acta Neurochir Suppl 2000;76:199–202.
Longhi L, Valeriani V, Rossi S, De Marchi M, Egidi M, Stocchetti N . Effects of hyperoxia on brain tissue oxygen tension in cerebral focal lesions. Acta Neurochir Suppl 2002;81:315–7.
Hlatky R, Valadka AB, Gopinath SP, Robertson CS . Brain tissue oxygen tension response to induced hyperoxia reduced in hypoperfused brain. J Neurosurg 2008;108:53–8.
Meixensberger J, Dings J, Kuhnigk H, Roosen K . Studies of tissue PO2 in normal and pathological human brain cortex. Acta Neurochir Suppl (Wien) 1993;59:58–63.
Rossi S, Longhi L, Balestreri M, Spagnoli D, deLeo A, Stocchetti N . Brain oxygen tension during hyperoxia in a swine model of cerebral ischaemia. Acta Neurochir Suppl 2000;76:243–5.
Armstead WM . Age dependent endothelin contribution to NOC/oFQ induced impairment of NMDA cerebrovasodilation after brain injury. Peptides 2001;22:39–46.
Jung KH, Chu K, Ko SY, et al. Early intravenous infusion of sodium nitrite protects brain against in vivo ischemia-reperfusion injury. Stroke 2006;37:2744–50.
Poloyac SM, Zhang Y, Bies RR, Kochanek PM, Graham SH . Protective effect of the 20-HETE inhibitor HET0016 on brain damage after temporary focal ischemia. J Cereb Blood Flow Metab 2006;26:1551–61.
Ristagno G, Tang W, Huang L, et al. Epinephrine reduces cerebral perfusion during cardiopulmonary resuscitation. Crit Care Med 2009;37:1408–15.
Masamoto K, Takizawa N, Kobayashi H, Oka K, Tanishita K . Dual responses of tissue partial pressure of oxygen after functional stimulation in rat somatosensory cortex. Brain Res 2003;979:104–13.
Andreasen A, Danscher G, Juhl S, et al. Distinct differences in partial oxygen pressure at micrometer ranges in the rat hippocampal region. J Neurosci Methods 1997;72:15–21.
Manole MD, Kochanek PM, Foley LM, et al. Polynitroxyl albumin and albumin therapy after pediatric asphyxial cardiac arrest: effects on cerebral blood flow and neurologic outcome. J Cereb Blood Flow Metab 2012;32:560–9.
Fink EL, Alexander H, Marco CD, et al. Experimental model of pediatric asphyxial cardiopulmonary arrest in rats. Pediatr Crit Care Med 2004;5:139–44.
Shoykhet M, Simons DJ, Kochanek PM, Clark RSB Anatomic evidence of injury to thalamocortical structures in a rodent model of pediatric asphyxia cardiac arrest. Critical Care Med 2011;38:Suppl:A152.
Dewachter P, Raëth-Fries I, Jouan-Hureaux V, et al. A comparison of epinephrine only, arginine vasopressin only, and epinephrine followed by arginine vasopressin on the survival rate in a rat model of anaphylactic shock. Anesthesiology 2007;106:977–83.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Manole, M., Kochanek, P., Bayır, H. et al. Brain tissue oxygen monitoring identifies cortical hypoxia and thalamic hyperoxia after experimental cardiac arrest in rats. Pediatr Res 75, 295–301 (2014). https://doi.org/10.1038/pr.2013.220
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2013.220
This article is cited by
-
Early Thalamocortical Reperfusion Leads to Neurologic Recovery in a Rodent Cardiac Arrest Model
Neurocritical Care (2022)
-
Combination of cardiac and thoracic pump theories in rodent cardiopulmonary resuscitation: a new method of three-side chest compression
Intensive Care Medicine Experimental (2019)
-
Effect of Electrical Vagus Nerve Stimulation on Cerebral Blood Flow and Neurological Outcome in Asphyxial Cardiac Arrest Model of Rats
Neurocritical Care (2019)
-
Enduring disturbances in regional cerebral blood flow and brain oxygenation at 24 h after asphyxial cardiac arrest in developing rats
Pediatric Research (2017)
-
A pilot cohort study of cerebral autoregulation and 2-year neurodevelopmental outcomes in neonates with hypoxic-ischemic encephalopathy who received therapeutic hypothermia
BMC Neurology (2015)