Abstract
Background:
We examined the relationships between pregnancy disorders leading to very preterm birth (spontaneous preterm labor, prelabor premature rupture of membranes (PPROM), hypertension/preeclampsia, intrauterine growth restriction (IUGR), antenatal hemorrhage, and maternal infection), both in isolation and grouped together as “disorders of placentation” (hypertensive disorders and IUGR) vs. “presumed infection/inflammation” (all the others), and several unfavorable neonatal outcomes.
Methods:
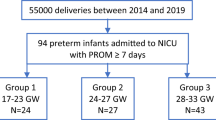
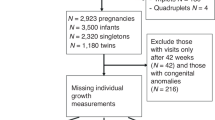
We examined a population-based prospective cohort of 2,085 singleton infants of 23–31 wk gestational age (GA) born in six Italian regions (the Accesso alle Cure e Terapie Intensive Ostetriche e Neonatali (ACTION) study).
Results:
Neonates born following disorders of placentation had a higher GA and better overall outcomes than those born following infection/inflammation. After adjustment for GA, however, they showed higher risk of mortality (odds ratio, OR: 1.4; 95% confidence interval, CI: 1.0–2.0), bronchopulmonary dysplasia (BPD) (OR: 2.5; CI: 1.8–3.6), and retinopathy of prematurity (ROP) (OR: 2.0; CI: 1.1–3.5), especially in growth-restricted infants, and a lower risk of intraventricular hemorrhage (IVH) (OR: 0.5; CI: 0.3–0.8) and periventricular leukomalacia (PVL) (OR: 0.6; CI: 0.4–1.1) as compared with infants born following infection/inflammation disorders.
Conclusion:
Our data confirm the hypothesis that, in very preterm infants, adverse outcomes are both a function of immaturity (low GA) and of complications leading to preterm birth. The profile of risk is different in different pregnancy disorders.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Basso O, Wilcox A . Mortality risk among preterm babies: immaturity versus underlying pathology. Epidemiology 2010;21:521–7.
Baud O, Zupan V, Lacaze-Masmonteil T, et al. The relationships between antenatal management, the cause of delivery and neonatal outcome in a large cohort of very preterm singleton infants. BJOG 2000;107:877–84.
McElrath TF, Hecht JL, Dammann O, et al.; ELGAN Study Investigators. Pregnancy disorders that lead to delivery before the 28th week of gestation: an epidemiologic approach to classification. Am J Epidemiol 2008;168:980–9.
Villar J, Abalos E, Carroli G, et al.; World Health Organization Antenatal Care Trial Research Group. Heterogeneity of perinatal outcomes in the preterm delivery syndrome. Obstet Gynecol 2004;104:78–87.
Chen XK, Wen SW, Smith G, Yang Q, Walker M . Pregnancy-induced hypertension is associated with lower infant mortality in preterm singletons. BJOG 2006;113:544–51.
Foix-L’helias L, Baud O, Lenclen R, Kaminski M, Lacaze-Masmonteil T . Benefit of antenatal glucocorticoids according to the cause of very premature birth. Arch Dis Child Fetal Neonatal Ed 2005;90:F46–8.
Bose C, Van Marter LJ, Laughon M, et al.; Extremely Low Gestational Age Newborn Study Investigators. Fetal growth restriction and chronic lung disease among infants born before the 28th week of gestation. Pediatrics 2009;124:e450–8.
Hansen AR, Barnés CM, Folkman J, McElrath TF . Maternal preeclampsia predicts the development of bronchopulmonary dysplasia. J Pediatr 2010;156:532–6.
O’Shea JE, Davis PG, Doyle LW ; Victorian Infant Collaborative Study Group. Maternal preeclampsia and risk of bronchopulmonary dysplasia in preterm infants. Pediatr Res 2012;71:210–4.
Durrmeyer X, Kayem G, Sinico M, Dassieu G, Danan C, Decobert F . Perinatal risk factors for bronchopulmonary dysplasia in extremely low gestational age infants: a pregnancy disorder-based approach. J Pediatr 2012;160:578–583.e2.
Kramer MS, Papageorghiou A, Culhane J, et al. Challenges in defining and classifying the preterm birth syndrome. Am J Obstet Gynecol 2012;206:108–12.
Klebanoff MA, Shiono PH . Top down, bottom up and inside out: reflections on preterm birth. Paediatr Perinat Epidemiol 1995;9:125–9.
Lal MK, Manktelow BN, Draper ES, Field DJ ; Population-based study. Chronic lung disease of prematurity and intrauterine growth retardation: a population-based study. Pediatrics 2003;111:483–7.
Zeitlin J, El Ayoubi M, Jarreau PH, et al.; MOSAIC Research Group. Impact of fetal growth restriction on mortality and morbidity in a very preterm birth cohort. J Pediatr 2010;157:733–9.e1.
Basso O, Wilcox AJ, Weinberg CR . Birth weight and mortality: causality or confounding? Am J Epidemiol 2006;164:303–11.
Lahra MM, Beeby PJ, Jeffery HE . Maternal versus fetal inflammation and respiratory distress syndrome: a 10-year hospital cohort study. Arch Dis Child Fetal Neonatal Ed 2009;94:F13–6.
Dammann O, Leviton A . Maternal intrauterine infection, cytokines, and brain damage in the preterm newborn. Pediatr Res 1997;42:1–8.
Wu YW, Colford JM Jr . Chorioamnionitis as a risk factor for cerebral palsy: A meta-analysis. JAMA 2000;284:1417–24.
Kusters CD, Chen ML, Follett PL, Dammann O . “Intraventricular” hemorrhage and cystic periventricular leukomalacia in preterm infants: how are they related? J Child Neurol 2009;24:1158–70.
Watterberg KL, Demers LM, Scott SM, Murphy S . Chorioamnionitis and early lung inflammation in infants in whom bronchopulmonary dysplasia develops. Pediatrics 1996;97:210–5.
Been JV, Zimmermann LJ . Histological chorioamnionitis and respiratory outcome in preterm infants. Arch Dis Child Fetal Neonatal Ed 2009;94:F218–25.
Lahra MM, Beeby PJ, Jeffery HE . Intrauterine inflammation, neonatal sepsis, and chronic lung disease: a 13-year hospital cohort study. Pediatrics 2009;123:1314–9.
Hartling L, Liang Y, Lacaze-Masmonteil T . Chorioamnionitis as a risk factor for bronchopulmonary dysplasia: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed 2012;97:F8–F17.
Levine RJ, Maynard SE, Qian C, et al. Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med 2004;350:672–83.
Thébaud B, Lacaze-Masmonteil T . If your placenta doesn’t have it, chances are your lungs don’t have it either: the “vascular hypothesis” of bronchopulmonary dysplasia starts in utero. J Pediatr 2010;156:521–3.
Gagliardi L, Bellù R, Zanini R, Dammann O ; Network Neonatale Lombardo Study Group. Bronchopulmonary dysplasia and brain white matter damage in the preterm infant: a complex relationship. Paediatr Perinat Epidemiol 2009;23:582–90.
Kotecha SJ, Watkins WJ, Heron J, Henderson J, Dunstan FD, Kotecha S . Spirometric lung function in school-age children: effect of intrauterine growth retardation and catch-up growth. Am J Respir Crit Care Med 2010;181:969–74.
Dhaliwal CA, Fleck BW, Wright E, Graham C, McIntosh N . Retinopathy of prematurity in small-for-gestational age infants compared with those of appropriate size for gestational age. Arch Dis Child Fetal Neonatal Ed 2009;94:F193–5.
Darlow BA, Hutchinson JL, Henderson-Smart DJ, Donoghue DA, Simpson JM, Evans NJ ; Australian and New Zealand Neonatal Network. Prenatal risk factors for severe retinopathy of prematurity among very preterm infants of the Australian and New Zealand Neonatal Network. Pediatrics 2005;115:990–6.
Ancel PY, Marret S, Larroque B, et al.; Epipage Study Group. Are maternal hypertension and small-for-gestational age risk factors for severe intraventricular hemorrhage and cystic periventricular leukomalacia? Results of the EPIPAGE cohort study. Am J Obstet Gynecol 2005;193:178–84.
Hernández-Díaz S, Schisterman EF, Hernán MA . The birth weight “paradox” uncovered? Am J Epidemiol 2006;164:1115–20.
Wilcox AJ, Weinberg CR, Basso O . On the pitfalls of adjusting for gestational age at birth. Am J Epidemiol 2011;174:1062–8.
VanderWeele TJ, Hernández-Diaz S . Is there a direct effect of pre-eclampsia on cerebral palsy not through preterm birth? Paediatr Perinat Epidemiol 2011;25:111–5.
Gagliardi L . Prediction and causal inference. Acta Paediatr 2009;98:1890–2.
Cuttini M, Casotto V, Orzalesi M ; Euronic Study Group. Ethical issues in neonatal intensive care and physicians’ practices: a European perspective. Acta Paediatr Suppl 2006;95:42–6.
McElrath TF, Hecht JL . Invited commentary: Intrauterine epidemiology. Am J Epidemiol 2009;170:159–61; discussion 162–3.
Villar J, Papageorghiou AT, Knight HE, et al. The preterm birth syndrome: a prototype phenotypic classification. Am J Obstet Gynecol 2012;206:119–23.
Papile LA, Burstein J, Burstein R, Koffler H . Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr 1978;92:529–34.
de Vries LS, Eken P, Dubowitz LM . The spectrum of leukomalacia using cranial ultrasound. Behav Brain Res 1992;49:1–6.
International Committee for the Classification of Retinopathy of Prematurity. An international classification of retinopathy of prematurity. Pediatrics 1984;74:127–33.
Acknowledgements
Hospitals and participants in the ACTION project have been listed in the Appendix. This article is affectionately dedicated to Eva Buiatti. As chief of the Epidemiological Section of the Regional Health Agency of Tuscany, she was, until her untimely death, a continuing source of inspiration and of generous support to this project.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gagliardi, L., Rusconi, F., Da Frè, M. et al. Pregnancy disorders leading to very preterm birth influence neonatal outcomes: results of the population-based ACTION cohort study. Pediatr Res 73, 794–801 (2013). https://doi.org/10.1038/pr.2013.52
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2013.52
This article is cited by
-
Early Fetal Growth Restriction with or Without Hypertensive Disorders: a Clinical Overview
Reproductive Sciences (2024)
-
Effectiveness of a care bundle for primary prevention of intraventricular hemorrhage in high-risk neonates: a Bayesian analysis
Journal of Perinatology (2023)
-
Complete blood count parameters as biomarkers of retinopathy of prematurity: a Portuguese multicenter study
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
The role of anti-vascular endothelial growth factor in treatment of retinopathy of prematurity—a current review
Eye (2022)
-
Retinopathy of prematurity: contribution of inflammatory and genetic factors
Molecular and Cellular Biochemistry (2022)