Abstract
Background:
Sensorineural hearing loss (SNHL) is a common feature in the postasphyxial syndrome in newborns. Several anesthetic drugs have been proposed to attenuate secondary neuronal injury elicited by hypoxia–ischemia. We hypothesized that propofol anesthesia reduces auditory impairment after perinatal asphyxia in comparison with isoflurane.
Methods:
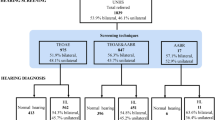
Twenty-three pregnant ewes were randomized to propofol or isoflurane anesthesia and sedation. The lambs underwent in utero umbilical cord occlusion (isoflurane n = 5; propofol n = 7) and were compared with sham-treated animals (isoflurane n = 5; propofol n = 6) at a gestational age of 133 d. For 8 h after delivery by cesarean section, repeated auditory brainstem responses (ABRs) were recorded to obtain hearing thresholds, peak amplitudes, latencies, and interpeak latencies.
Results:
Significantly elevated mean thresholds, diminished amplitudes, and elevated latencies were observed in the asphyxia group relative to the control group through the observation period. Comparison of anesthetic treatment in the asphyxia group revealed a significantly lower elevation in threshold and less impairment in the ABR amplitudes and latencies during propofol anesthesia as compared with isoflurane anesthesia.
Conclusion:
Our results support the hypothesis that anesthesia with propofol has a preventive effect on the functional changes to the auditory pathway in the event of perinatal asphyxia.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Mencher GT . Challenge of epidemiological research in the developing world: overview. Audiology 2000;39:178–83.
Davis A, Wood S, Healy R, Webb H, Rowe S . Risk factors for hearing disorders: epidemiologic evidence of change over time in the UK. J Am Acad Audiol 1995;6:365–70.
Erenberg A, Lemons J, Sia C, Trunkel D, Ziring P . Newborn and infant hearing loss: detection and intervention. American Academy of Pediatrics. Task Force on Newborn and Infant Hearing, 1998–1999. Pediatrics 1999;103:527–30.
Nance WE, Lim BG, Dodson KM . Importance of congenital cytomegalovirus infections as a cause for pre-lingual hearing loss. J Clin Virol 2006;35:221–5.
Borg E . Perinatal asphyxia, hypoxia, ischemia and hearing loss. An overview. Scand Audiol 1997;26:77–91.
Pierrat V, Haouari N, Liska A, Thomas D, Subtil D, Truffert P ; Groupe d’Etudes en Epidémiologie Périnatale. Prevalence, causes, and outcome at 2 years of age of newborn encephalopathy: population based study. Arch Dis Child Fetal Neonatal Ed 2005;90:F257–61.
de Haan M, Wyatt JS, Roth S, Vargha-Khadem F, Gadian D, Mishkin M . Brain and cognitive-behavioural development after asphyxia at term birth. Dev Sci 2006;9:350–8.
Johnston MV, Trescher WH, Ishida A, Nakajima W . Neurobiology of hypoxic-ischemic injury in the developing brain. Pediatr Res 2001;49:735–41.
Jiang ZD, Yin R, Shao XM, Wilkinson AR . Brain-stem auditory impairment during the neonatal period in term infants after asphyxia: dynamic changes in brain-stem auditory evoked response to clicks of different rates. Clin Neurophysiol 2004;115:1605–15.
Jiang ZD, Brosi DM, Wang J, et al. Time course of brainstem pathophysiology during first month in term infants after perinatal asphyxia, revealed by MLS BAER latencies and intervals. Pediatr Res 2003;54:680–7.
Inagaki M, Kaga M, Isumi H, Hirano S, Takashima S, Nanba E . Hypoxia-induced ABR change and heat shock protein expression in the pontine auditory pathway of young rabbits. Brain Res 1997;757:111–8.
Schifilliti D, Grasso G, Conti A, Fodale V . Anaesthetic-related neuroprotection: intravenous or inhalational agents? CNS Drugs 2010;24:893–907.
Koerner IP, Brambrink AM . Brain protection by anesthetic agents. Curr Opin Anaesthesiol 2006;19:481–6.
Kotani Y, Shimazawa M, Yoshimura S, Iwama T, Hara H . The experimental and clinical pharmacology of propofol, an anesthetic agent with neuroprotective properties. CNS Neurosci Ther 2008;14:95–106.
Acquaviva R, Campisi A, Raciti G, et al. Propofol inhibits caspase-3 in astroglial cells: role of heme oxygenase-1. Curr Neurovasc Res 2005;2:141–8.
Chen L, Xue Z, Jiang H . Effect of propofol on pathologic time-course and apoptosis after cerebral ischemia-reperfusion injury. Acta Anaesthesiol Scand 2008;52:413–9.
Hans P, Bonhomme V . Why we still use intravenous drugs as the basic regimen for neurosurgical anaesthesia. Curr Opin Anaesthesiol 2006;19:498–503.
Vasileiou I, Xanthos T, Koudouna E, et al. Propofol: a review of its non-anaesthetic effects. Eur J Pharmacol 2009;605:1–8.
Istaphanous GK, Loepke AW . General anesthetics and the developing brain. Curr Opin Anaesthesiol 2009;22:368–73.
Irifune M, Takarada T, Shimizu Y, et al. Propofol-induced anesthesia in mice is mediated by gamma-aminobutyric acid-A and excitatory amino acid receptors. Anesth Analg 2003;97:424–9, table of contents.
Durrmeyer X, Vutskits L, Anand KJ, Rimensberger PC . Use of analgesic and sedative drugs in the NICU: integrating clinical trials and laboratory data. Pediatr Res 2010;67:117–27.
Back SA, Riddle A, Hohimer AR . Role of instrumented fetal sheep preparations in defining the pathogenesis of human periventricular white-matter injury. J Child Neurol 2006;21:582–9.
Hagberg H, Peebles D, Mallard C . Models of white matter injury: comparison of infectious, hypoxic-ischemic, and excitotoxic insults. Ment Retard Dev Disabil Res Rev 2002;8:30–8.
Wolfs TG, Jellema RK, Turrisi G, Becucci E, Buonocore G, Kramer BW . Inflammation-induced immune suppression of the fetus: a potential link between chorioamnionitis and postnatal early onset sepsis. J Matern Fetal Neonatal Med 2012;25:Suppl 1:8–11.
Mallard EC, Williams CE, Johnston BM, Gluckman PD . Increased vulnerability to neuronal damage after umbilical cord occlusion in fetal sheep with advancing gestation. Am J Obstet Gynecol 1994;170(1 Pt 1):206–14.
Gunn AJ, Cook CJ, Williams CE, Johnston BM, Gluckman PD . Electrophysiological responses of the fetus to hypoxia and asphyxia. J Dev Physiol 1991;16:147–53.
Pasternak JF . Hypoxic-ischemic brain damage in the term infant. Lessons from the laboratory. Pediatr Clin North Am 1993;40:1061–72.
Grasshoff C, Gillessen T . The effect of propofol on increased superoxide concentration in cultured rat cerebrocortical neurons after stimulation of N-methyl-d-aspartate receptors. Anesth Analg 2002;95:920–2, table of contents.
Orser BA, Bertlik M, Wang LY, MacDonald JF . Inhibition by propofol (2,6 di-isopropylphenol) of the N-methyl-D-aspartate subtype of glutamate receptor in cultured hippocampal neurones. Br J Pharmacol 1995;116:1761–8.
Abboud TK, Zhu J, Richardson M, Peres Da Silva E, Donovan M . Intravenous propofol vs thiamylal-isoflurane for caesarean section, comparative maternal and neonatal effects. Acta Anaesthesiol Scand 1995;39:205–9.
Wakasugi M, Hirota K, Roth SH, Ito Y . The effects of general anesthetics on excitatory and inhibitory synaptic transmission in area CA1 of the rat hippocampus in vitro. Anesth Analg 1999;88:676–80.
Buonocore G, Perrone S, Turrisi G, Kramer BW, Balduini W . New pharmacological approaches in infants with hypoxic-ischemic encephalopathy. Curr Pharm Des 2012;18:3086–100.
Bercker S, Bert B, Bittigau P, et al. Neurodegeneration in newborn rats following propofol and sevoflurane anesthesia. Neurotox Res 2009;16:140–7.
Pesic V, Milanovic D, Tanic N, et al. Potential mechanism of cell death in the developing rat brain induced by propofol anesthesia. Int J Dev Neurosci 2009;27:279–87.
Fredriksson A, Pontén E, Gordh T, Eriksson P . Neonatal exposure to a combination of N-methyl-D-aspartate and gamma-aminobutyric acid type A receptor anesthetic agents potentiates apoptotic neurodegeneration and persistent behavioral deficits. Anesthesiology 2007;107:427–36.
Seehase M, Houthuizen P, Jellema RK, et al. Propofol administration to the fetal-maternal unit reduces cardiac injury in late-preterm lambs subjected to severe prenatal asphyxia and cardiac arrest. Pediatr Res 2013;73:427–34.
Vento M, Saugstad OD . Resuscitation of the term and preterm infant. Semin Fetal Neonatal Med 2010;15:216–22.
Pierson LL, Gerhardt KJ, Griffiths SK, Abrams RM . Auditory brainstem response in sheep. Part I: fetal development. Dev Psychobiol 1995;28:293–305.
Author information
Authors and Affiliations
Corresponding author
PowerPoint slides
Rights and permissions
About this article
Cite this article
Smit, A., Seehase, M., Stokroos, R. et al. Functional impairment of the auditory pathway after perinatal asphyxia and the short-term effect of perinatal propofol anesthesia in lambs. Pediatr Res 74, 34–38 (2013). https://doi.org/10.1038/pr.2013.64
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2013.64
This article is cited by
-
Sheep as a large animal model for hearing research: comparison to common laboratory animals and humans
Laboratory Animal Research (2023)
-
The influence of anesthetics on substantia nigra tyrosine hydroxylase expression and tau phosphorylation in the hypoxic–ischemic near-term lamb
Pediatric Research (2018)
-
Propofol administration to the fetal–maternal unit reduces cardiac oxidative stress in preterm lambs subjected to prenatal asphyxia and cardiac arrest
Pediatric Research (2016)
-
Propofol administration to the maternal-fetal unit improved fetal EEG and influenced cerebral apoptotic pathway in preterm lambs suffering from severe asphyxia
Molecular and Cellular Pediatrics (2015)