Abstract
Background:
Childhood sleep disordered breathing (SDB) presents as isolated respiratory events or episodes of consecutive repetitive events. We hypothesized that the surge in blood pressure (BP) and heart rate (HR) would be greater at the termination of events during episodes of repetitive events than following isolated events.
Methods:
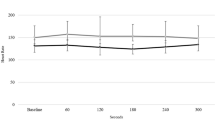
% change in HR and pulse transit time (PTT; inverse surrogate of BP) were calculated from the last half of an event to: (i) between successive repetitive events; (ii) termination of the last repetitive event; (iii) event termination for isolated events.
Results:
69% of the children exhibiting both isolated and repetitive events had more repetitive than isolated events. %HR change between repetitive events (27 ± 1%) was greater than at event termination for isolated events (17 ± 1%; P < 0.001). %PTT change at the termination of the last repetitive event (−8 ± 2%) was greater than at the termination of isolated events (−2 ± 2%; P < 0.05).
Conclusion:
Episodes of repetitive respiratory events evoke a greater acute cardiovascular response, including surges in BP and HR between events, than do isolated events. Given that the majority of respiratory events in preschool children occur as repetitive episodes, this finding should be taken into account when assessing the impact of respiratory events for a given child.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Mindell JA, Owens JA. Pediatric Sleep, Diagnosis and Management of Sleep Problems. 2nd edn. Philadelphia: Lippincott Williams and Wilkins, 2010.
Mindell JA, Owens JA. Sleep-disordered breathing and obstructive sleep apnea syndrome. Pediatric Sleep: Diagnosis and Management of Sleep Problems. 2nd edn. Philadelphia: Lippincott Williams and Wilkins, a Wolters Kluwer Health business, 2010. pp. 100–15.
Horne RS, Yang JS, Walter LM, et al. Elevated blood pressure during sleep and wake in children with sleep-disordered breathing. Pediatrics 2011;128:e85–92.
Li AM, Au CT, Sung RY, et al. Ambulatory blood pressure in children with obstructive sleep apnoea: a community based study. Thorax 2008;63:803–9.
Nisbet LC, Yiallourou SR, Biggs SN, et al. Preschool children with obstructive sleep apnea: the beginnings of elevated blood pressure? Sleep 2013;36:1219–26.
Amin R, Somers VK, McConnell K, et al. Activity-adjusted 24-hour ambulatory blood pressure and cardiac remodeling in children with sleep disordered breathing. Hypertension 2008;51:84–91.
Amin RS, Kimball TR, Bean JA, et al. Left ventricular hypertrophy and abnormal ventricular geometry in children and adolescents with obstructive sleep apnea. Am J Respir Crit Care Med 2002;165:1395–9.
Hamilton GS, Solin P, Naughton MT. Obstructive sleep apnoea and cardiovascular disease. Intern Med J 2004;34:420–6.
Stoohs R, Guilleminault C. Cardiovascular changes associated with obstructive sleep apnea syndrome. J Appl Physiol (1985) 1992;72:583–9.
O’Driscoll DM, Foster AM, Ng ML, et al. Acute cardiovascular changes with obstructive events in children with sleep disordered breathing. Sleep 2009;32:1265–71.
Nisbet LC, Yiallourou SR, Nixon GM, et al. Characterization of the acute pulse transit time response to obstructive apneas and hypopneas in preschool children with sleep-disordered breathing. Sleep Med 2013;14:1123–31.
Traeger N, Schultz B, Pollock AN, Mason T, Marcus CL, Arens R. Polysomnographic values in children 2-9 years old: additional data and review of the literature. Pediatr Pulmonol 2005;40:22–30.
Montgomery-Downs HE, O’Brien LM, Gulliver TE, Gozal D. Polysomnographic characteristics in normal preschool and early school-aged children. Pediatrics 2006;117:741–53.
O’Driscoll DM, Foster AM, Ng ML, et al. Central apnoeas have significant effects on blood pressure and heart rate in children. J Sleep Res 2009;18:415–21.
Okabe S, Hida W, Kikuchi Y, et al. Role of hypoxia on increased blood pressure in patients with obstructive sleep apnoea. Thorax 1995;50:28–34.
Ringler J, Basner RC, Shannon R, et al. Hypoxemia alone does not explain blood pressure elevations after obstructive apneas. J Appl Physiol (1985) 1990;69:2143–8.
Azarbarzin A, Ostrowski M, Hanly P, Younes M. Relationship between arousal intensity and heart rate response to arousal. Sleep 2014;37:645–53.
Bonnet MH, Arand DL. Heart rate variability: sleep stage, time of night, and arousal influences. Electroencephalogr Clin Neurophysiol 1997;102:390–6.
Somers VK, White DP, Amin R, et al.; American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology; American Heart Association Stroke Council; American Heart Association Council on Cardiovascular Nursing; American College of Cardiology Foundation. Sleep apnea and cardiovascular disease: an American Heart Association/american College Of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council On Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). Circulation 2008;118:1080–111.
Dempsey JA, Veasey SC, Morgan BJ, O’Donnell CP. Pathophysiology of sleep apnea. Physiol Rev 2010;90:47–112.
Imadojemu VA, Gleeson K, Gray KS, Sinoway LI, Leuenberger UA. Obstructive apnea during sleep is associated with peripheral vasoconstriction. Am J Respir Crit Care Med 2002;165:61–6.
Lucking EF, O’Halloran KD, Jones JF. Increased cardiac output contributes to the development of chronic intermittent hypoxia-induced hypertension. Exp Physiol 2014;99:1312–24.
Fagan KA. Selected Contribution: Pulmonary hypertension in mice following intermittent hypoxia. J Appl Physiol (1985) 2001;90:2502–7.
Campen MJ, Shimoda LA, O’Donnell CP. Acute and chronic cardiovascular effects of intermittent hypoxia in C57BL/6J mice. J Appl Physiol (1985) 2005;99:2028–35.
Nisbet RE, Graves AS, Kleinhenz DJ, et al. The role of NADPH oxidase in chronic intermittent hypoxia-induced pulmonary hypertension in mice. Am J Respir Cell Mol Biol 2009;40:601–9.
Nishioka S, Yoshioka T, Nomura A, et al. Celiprolol reduces oxidative stress and attenuates left ventricular remodeling induced by hypoxic stress in mice. Hypertens Res 2013;36:934–9.
Gozal D, Hakim F, Kheirandish-Gozal L. Chemoreceptors, baroreceptors, and autonomic deregulation in children with obstructive sleep apnea. Respir Physiol Neurobiol 2013;185:177–85.
Trinder J, Allen N, Kleiman J, et al. On the nature of cardiovascular activation at an arousal from sleep. Sleep 2003;26:543–51.
Eckert DJ, Malhotra A, Jordan AS. Mechanisms of apnea. Prog Cardiovasc Dis 2009;51:313–23.
Dunai J, Wilkinson M, Trinder J. Interaction of chemical and state effects on ventilation during sleep onset. J Appl Physiol (1985) 1996;81:2235–43.
Khoo MC, Gottschalk A, Pack AI. Sleep-induced periodic breathing and apnea: a theoretical study. J Appl Physiol (1985) 1991;70:2014–24.
Kuniyoshi FH, Pusalavidyasagar S, Singh P, Somers VK. Cardiovascular consequences of obstructive sleep apnoea. Indian J Med Res 2010;131:196–205.
Narkiewicz K, Montano N, Cogliati C, van de Borne PJ, Dyken ME, Somers VK. Altered cardiovascular variability in obstructive sleep apnea. Circulation 1998;98:1071–7.
Romero-Corral A, Somers VK, Pellikka PA, et al. Decreased right and left ventricular myocardial performance in obstructive sleep apnea. Chest 2007;132:1863–70.
Ogden CL, Kuczmarski RJ, Flegal KM, et al. Centers for Disease Control and Prevention 2000 growth charts for the United States: improvements to the 1977 National Center for Health Statistics version. Pediatrics 2002;109:45–60.
Iber C, Ancoli-Israel S, Chesson A, Quan SF. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specification. 1st edn. Westchester, IL: American Academy of Sleep Medicine, 2007.
Nixon GM, Hyde M, Biggs SN, Walter LM, Horne RS, Davey MJ. The impact of recent changes to the respiratory scoring rules in pediatrics. J Clin Sleep Med 2014;10:1217–21.
Nisbet LC, Yiallourou SR, Nixon GM, et al. Nocturnal autonomic function in preschool children with sleep-disordered breathing. Sleep Med 2013;14:1310–6.
Vlahandonis A, Biggs SN, Nixon GM, Davey MJ, Walter LM, Horne RS. Pulse transit time as a surrogate measure of changes in systolic arterial pressure in children during sleep. J Sleep Res 2014;23:406–13.
Acknowledgements
The authors would like to thank the children and families who participated in this study and the staff of the Melbourne Children’s Sleep Centre for their support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Walter, L., Biggs, S., Nisbet, L. et al. Augmented cardiovascular responses to episodes of repetitive compared with isolated respiratory events in preschool children with sleep-disordered breathing. Pediatr Res 78, 560–566 (2015). https://doi.org/10.1038/pr.2015.147
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2015.147