Abstract
Background:
Postsurgical bleeding causes significant morbidity and mortality in children undergoing surgery for congenital heart defects (CHD). 22q11.2 deletion syndrome (DS) is the second most common genetic risk factor for CHD. The deleted segment of chromosome 22q11.2 encompasses the gene encoding glycoprotein (GP) Ibβ, which is required for expression of the GPIb-V-IX complex on the platelet surface, where it functions as the receptor for von Willebrand factor (VWF). Binding of GPIb-V-IX to VWF is important for platelets to initiate hemostasis. It is not known whether hemizygosity for the gene encoding GPIbβ increases the risk for bleeding following cardiac surgery for patients with 22q11.2 DS.
Methods:
We performed a case–control study of 91 pediatric patients who underwent cardiac surgery with cardiopulmonary bypass from 2004 to 2012 at Children’s Hospital of Wisconsin.
Results:
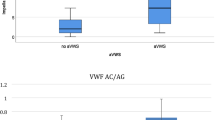
Patients with 22q11.2 DS had larger platelets and lower platelet counts, bled more excessively, and received more transfusion support with packed red blood cells in the early postoperative period relative to control patients.
Conclusion:
Presurgical genetic testing for 22q11.2 DS may help to identify a subset of pediatric cardiac surgery patients who are at increased risk for excessive bleeding and who may require more transfusion support in the postoperative period.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Reller MD, Strickland MJ, Riehle-Colarusso T, Mahle WT, Correa A. Prevalence of congenital heart defects in metropolitan Atlanta, 1998-2005. J Pediatr 2008;153:807–13.
Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol 2002;39:1890–900.
Martin JA, Hamilton BE, Ventura SJ, et al. Births: final data for 2009. Natl Vital Stat Rep 2011;60:1–70.
Moller JH, Taubert KA, Allen HD, Clark EB, Lauer RM. Cardiovascular health and disease in children: current status. A Special Writing Group from the Task Force on Children and Youth, American Heart Association. Circulation 1994;89:923–30.
Ranucci M, Carlucci C, Isgrò G, Baryshnikova E. A prospective pilot study of platelet function and its relationship with postoperative bleeding in pediatric cardiac surgery. Minerva Anestesiol 2012;78:556–63.
Moganasundram S, Hunt BJ, Sykes K, et al. The relationship among thromboelastography, hemostatic variables, and bleeding after cardiopulmonary bypass surgery in children. Anesth Analg 2010;110:995–1002.
Kern FH, Morana NJ, Sears JJ, Hickey PR. Coagulation defects in neonates during cardiopulmonary bypass. Ann Thorac Surg 1992;54:541–6.
Gill R, Herbertson M, Vuylsteke A, et al. Safety and efficacy of recombinant activated factor VII: a randomized placebo-controlled trial in the setting of bleeding after cardiac surgery. Circulation 2009;120:21–7.
Székely A, Cserép Z, Sápi E, et al. Risks and predictors of blood transfusion in pediatric patients undergoing open heart operations. Ann Thorac Surg 2009;87:187–97.
Moulton MJ, Creswell LL, Mackey ME, Cox JL, Rosenbloom M. Reexploration for bleeding is a risk factor for adverse outcomes after cardiac operations. J Thorac Cardiovasc Surg 1996;111:1037–46.
Unsworth-White MJ, Herriot A, Valencia O, et al. Resternotomy for bleeding after cardiac operation: a marker for increased morbidity and mortality. Ann Thorac Surg 1995;59:664–7.
Kobrynski LJ, Sullivan KE. Velocardiofacial syndrome, DiGeorge syndrome: the chromosome 22q11.2 deletion syndromes. Lancet 2007;370:1443–52.
Wilson DI, Burn J, Scambler P, Goodship J. DiGeorge syndrome: part of CATCH 22. J Med Genet 1993;30:852–6.
GeneReviews. 22q11.2 Deletion Syndrome, 2013. (http://www.ncbi.nlm.nih.gov/books/NBK1523/.)
Khositseth A, Tocharoentanaphol C, Khowsathit P, Ruangdaraganon N. Chromosome 22q11 deletions in patients with conotruncal heart defects. Pediatr Cardiol 2005;26:570–3.
McDonald-McGinn DM, Tonnesen MK, Laufer-Cahana A, et al. Phenotype of the 22q11.2 deletion in individuals identified through an affected relative: cast a wide FISHing net! Genet Med 2001;3:23–9.
Michaelovsky E, Frisch A, Carmel M, et al. Genotype-phenotype correlation in 22q11.2 deletion syndrome. BMC Med Genet 2012;13:122.
Rauch A, Zink S, Zweier C, et al. Systematic assessment of atypical deletions reveals genotype-phenotype correlation in 22q11.2. J Med Genet 2005;42:871–6.
Shaikh TH, Kurahashi H, Saitta SC, et al. Chromosome 22-specific low copy repeats and the 22q11.2 deletion syndrome: genomic organization and deletion endpoint analysis. Hum Mol Genet 2000;9:489–501.
Saitta SC, Harris SE, Gaeth AP, et al. Aberrant interchromosomal exchanges are the predominant cause of the 22q11.2 deletion. Hum Mol Genet 2004;13:417–28.
López JA, Leung B, Reynolds CC, Li CQ, Fox JE. Efficient plasma membrane expression of a functional platelet glycoprotein Ib-IX complex requires the presence of its three subunits. J Biol Chem 1992;267:12851–9.
Calverley DC, Yagi M, Stray SM, Roth GJ. Human platelet glycoprotein V: its role in enhancing expression of the glycoprotein Ib receptor. Blood 1995;86:1361–7.
Berndt MC, Andrews RK. Bernard-Soulier syndrome. Haematologica 2011;96:355–9.
Naqvi N, Davidson SJ, Wong D, et al. Predicting 22q11.2 deletion syndrome: a novel method using the routine full blood count. Int J Cardiol 2011;150:50–3.
Kato T, Kosaka K, Kimura M, et al. Thrombocytopenia in patients with 22q11.2 deletion syndrome and its association with glycoprotein Ib-beta. Genet Med 2003;5:113–9.
Lawrence S, McDonald-McGinn DM, Zackai E, Sullivan KE. Thrombocytopenia in patients with chromosome 22q11.2 deletion syndrome. J Pediatr 2003;143:277–8.
Van Geet C, Devriendt K, Eyskens B, Vermylen J, Hoylaerts MF. Velocardiofacial syndrome patients with a heterozygous chromosome 22q11 deletion have giant platelets. Pediatr Res 1998;44:607–11.
Liang HP, Morel-Kopp MC, Curtin J, et al. Heterozygous loss of platelet glycoprotein (GP) Ib-V-IX variably affects platelet function in velocardiofacial syndrome (VCFS) patients. Thromb Haemost 2007;98:1298–308.
Rosa RF, Rosa RC, Dos Santos PP, Zen PR, Paskulin GA. Hematological abnormalities and 22q11.2 deletion syndrome. Rev Bras Hematol Hemoter 2011;33:151–4.
Takahashi K, Kido S, Hoshino K, Ogawa K, Ohashi H, Fukushima Y. Frequency of a 22q11 deletion in patients with conotruncal cardiac malformations: a prospective study. Eur J Pediatr 1995;154:878–81.
Amati F, Mari A, Digilio MC, et al. 22q11 deletions in isolated and syndromic patients with tetralogy of Fallot. Hum Genet 1995;95:479–82.
Peyvandi S, Lupo PJ, Garbarini J, et al. 22q11.2 deletions in patients with conotruncal defects: data from 1,610 consecutive cases. Pediatr Cardiol 2013;34:1687–94.
Williams GD, Bratton SL, Ramamoorthy C. Factors associated with blood loss and blood product transfusions: a multivariate analysis in children after open-heart surgery. Anesth Analg 1999;89:57–64.
Despotis GJ, Avidan MS, Hogue CW Jr . Mechanisms and attenuation of hemostatic activation during extracorporeal circulation. Ann Thorac Surg 2001;72:S1821–31.
Williams GD, Bratton SL, Riley EC, Ramamoorthy C. Association between age and blood loss in children undergoing open heart operations. Ann Thorac Surg 1998;66:870–5; discussion 875–6.
Guay J, Rivard GE. Mediastinal bleeding after cardiopulmonary bypass in pediatric patients. Ann Thorac Surg 1996;62:1955–60.
Agarwal HS, Barrett SS, Barry K, et al. Association of blood products administration during cardiopulmonary bypass and excessive post-operative bleeding in pediatric cardiac surgery. Pediatr Cardiol 2015;36:459–67.
Tomita-Mitchell A, Mahnke DK, Larson JM, et al. Multiplexed quantitative real-time PCR to detect 22q11.2 deletion in patients with congenital heart disease. Physiol Genomics 2010;42A:52–60.
Williams GD, Bratton SL, Riley EC, Ramamoorthy C. Coagulation tests during cardiopulmonary bypass correlate with blood loss in children undergoing cardiac surgery. J Cardiothorac Vasc Anesth 1999;13:398–404.
Greeley WJ, Bushman GA, Kong DL, Oldham HN, Peterson MB. Effects of cardiopulmonary bypass on eicosanoid metabolism during pediatric cardiovascular surgery. J Thorac Cardiovasc Surg 1988;95:842–9.
Acknowledgements
The authors thank Tao Wang for help with statistical analyses and PCTHRC members D. Woodrow Benson, Jim Tweddell, Ron Woods, Jake Scott, Rob Neibler, Bob Montgomery, Alan Mast, Susan Maroney, Julie Slicker, Rowena Punzalan, and Paul Scott for helpful study design and editorial comments. The authors are indebted to Roy Silverstein for helpful editorial comments.
Author information
Authors and Affiliations
Corresponding author
PowerPoint slides
Rights and permissions
About this article
Cite this article
Brenner, M., Clarke, S., Mahnke, D. et al. Effect of 22q11.2 deletion on bleeding and transfusion utilization in children with congenital heart disease undergoing cardiac surgery. Pediatr Res 79, 318–324 (2016). https://doi.org/10.1038/pr.2015.216
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2015.216
This article is cited by
-
In the line-up: deleted genes associated with DiGeorge/22q11.2 deletion syndrome: are they all suspects?
Journal of Neurodevelopmental Disorders (2019)