Abstract
Background:
Preterm infants are at risk of iron deficiency (ID). Hepcidin has been suggested as a good additional indicator of ID in preterm infants, next to ferritin.
Methods:
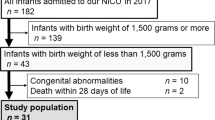
In a prospective observational study, we analyzed serum hepcidin in 111 infants born after 32+0 to 36+6 wk gestational age during the first 4 mo of life.
Results:
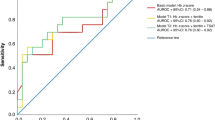
Hepcidin concentrations decreased during the first 4 mo of life, and concentrations were lower in infants with ID compared to those without ID. Infants who developed ID at the age of 4 mo had already significantly lower levels of hepcidin at 1.5 mo of age, while ferritin was already significantly lower at the age of 1 wk.
Conclusion:
Hepcidin concentrations of late preterm infants decrease during the first 4 mo of life. This decrease, which parallels a decrease of ferritin concentration, we interpret as a physiological response, aiming to increase iron availability. Hepcidin concentrations are lower in infants with ID compared with those without ID, with a notable change already observed at 1.5 mo of age. Hepcidin can be used as an early marker of ID, although an additive value of hepcidin over ferritin in the diagnosis of ID is not present.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Lozoff B, Jimenez E, Smith JB. Double burden of iron deficiency in infancy and low socioeconomic status: a longitudinal analysis of cognitive test scores to age 19 years. Arch Pediatr Adolesc Med 2006;160:1108–13.
Beard J. Recent evidence from human and animal studies regarding iron status and infant development. J Nutr 2007;137:524S–530S.
Kroot JJ, Tjalsma H, Fleming RE, Swinkels DW. Hepcidin in human iron disorders: diagnostic implications. Clin Chem 2011;57:1650–69.
Nemeth E, Tuttle MS, Powelson J, et al. Hepcidin regulates cellular iron efflux by binding to ferroportin and inducing its internalization. Science 2004;306:2090–3.
Ganz T, Nemeth E. Hepcidin and iron homeostasis. Biochim Biophys Acta 2012;1823:1434–43.
Ganz T, Nemeth E. Regulation of iron acquisition and iron distribution in mammals. Biochim Biophys Acta 2006;1763:690–9.
Ganz T, Nemeth E. Iron sequestration and anemia of inflammation. Semin Hematol 2009;46:387–93.
Berglund S, Lönnerdal B, Westrup B, Domellöf M. Effects of iron supplementation on serum hepcidin and serum erythropoietin in low-birth-weight infants. Am J Clin Nutr 2011;94:1553–61.
Verweij A, Sanders C, van der Lucht F, and den Hartog FRJ. [Training and education: what is the current situation?] Nationaal Kompas, 2014. (http://www.nationaalkompas.nl/bevolking/sociaaleconomische-status/wat-is-sociaaleconomische-status/.)
Centraal Bureau voor de Statistiek. [Migration; country of origin, homeland and gender] Centraal Bureau voor de statistiek, 2015. (http://statline.cbs.nl/StatWeb/publication/?VW=T&DM=SLNL&PA=60032&LA=NL.)
Schaap CC, Hendriks JC, Kortman GA, et al. Diurnal rhythm rather than dietary iron mediates daily hepcidin variations. Clin Chem 2013;59:527–35.
Galesloot TE, Vermeulen SH, Geurts-Moespot AJ, et al. Serum hepcidin: reference ranges and biochemical correlates in the general population. Blood 2011;117:e218–25.
Kroot JJ, van Herwaarden AE, Tjalsma H, Jansen RT, Hendriks JC, Swinkels DW. Second round robin for plasma hepcidin methods: first steps toward harmonization. Am J Hematol 2012;87:977–83.
Mupfudze TG, Stoltzfus RJ, Rukobo S, Moulton LH, Humphrey JH, Prendergast AJ ; SHINE Project Team. Hepcidin decreases over the first year of life in healthy African infants. Br J Haematol 2014;164:150–3.
Dube K, Schwartz J, Mueller MJ, Kalhoff H, Kersting M. Iron intake and iron status in breastfed infants during the first year of life. Clin Nutr 2010;29:773–8.
Wisaksana R, de Mast Q, Alisjahbana B, et al. Inverse relationship of serum hepcidin levels with CD4 cell counts in HIV-infected patients selected from an Indonesian prospective cohort study. PLoS One 2013;8:e79904.
Jaeggi T, Moretti D, Kvalsvig J, et al. Iron status and systemic inflammation, but not gut inflammation, strongly predict gender-specific concentrations of serum hepcidin in infants in rural Kenya. PLoS One 2013;8:e57513.
Bachman E, Feng R, Travison T, et al. Testosterone suppresses hepcidin in men: a potential mechanism for testosterone-induced erythrocytosis. J Clin Endocrinol Metab 2010;95:4743–7.
Latour C, Kautz L, Besson-Fournier C, et al. Testosterone perturbs systemic iron balance through activation of epidermal growth factor receptor signaling in the liver and repression of hepcidin. Hepatology 2014;59:683–94.
Bachman E, Travison TG, Basaria S, et al. Testosterone induces erythrocytosis via increased erythropoietin and suppressed hepcidin: evidence for a new erythropoietin/hemoglobin set point. J Gerontol A Biol Sci Med Sci 2014;69:725–35.
Alexander GM. Postnatal testosterone concentrations and male social development. Front Endocrinol (Lausanne) 2014;5:15.
Forest MG, de Peretti E, Bertrand J. Testicular and adrenal androgens and their binding to plasma proteins in the perinatal period: developmental patterns of plasma testosterone, 4-androstenedione, dehydroepiandrosterone and its sulfate in premature and small for date infants as compared with that of full-term infants. J Steroid Biochem 1980;12:25–36.
Tapanainen J, Koivisto M, Vihko R, Huhtaniemi I. Enhanced activity of the pituitary-gonadal axis in premature human infants. J Clin Endocrinol Metab 1981;52:235–8.
Kuiri-Hänninen T, Seuri R, Tyrväinen E, et al. Increased activity of the hypothalamic-pituitary-testicular axis in infancy results in increased androgen action in premature boys. J Clin Endocrinol Metab 2011;96:98–105.
Müller KF, Lorenz L, Poets CF, Westerman M, Franz AR. Hepcidin concentrations in serum and urine correlate with iron homeostasis in preterm infants. J Pediatr 2012;160:949–53.e2.
Troutt JS, Rudling M, Persson L, et al. Circulating human hepcidin-25 concentrations display a diurnal rhythm, increase with prolonged fasting, and are reduced by growth hormone administration. Clin Chem 2012;58:1225–32.
Bayele HK, McArdle H, Srai SK. Cis and trans regulation of hepcidin expression by upstream stimulatory factor. Blood 2006;108:4237–45.
Bhatia J, Griffin I, Anderson D, Kler N, Domellöf M. Selected macro/micronutrient needs of the routine preterm infant. J Pediatr 2013;162: Suppl 3:S48–55.
Uijterschout L, Domellöf M, Abbink M, et al. Iron deficiency in the first 6 months of age in infants born between 32 and 37 weeks of gestational age. Eur J Clin Nutr 2015;69:598–602.
Domellöf M, Braegger C, Campoy C, et al.; ESPGHAN Committee on Nutrition. Iron requirements of infants and toddlers. J Pediatr Gastroenterol Nutr 2014;58:119–29.
Schönbeck Y, Talma H, van Dommelen P, et al. The world’s tallest nation has stopped growing taller: the height of Dutch children from 1955 to 2009. Pediatr Res 2013;73:371–7.
McDonald SJ, Middleton P, Dowswell T, Morris PS. Effect of timing of umbilical cord clamping of term infants on maternal and neonatal outcomes. Cochrane Database Syst Rev 2013;7:CD004074.
Schiza V, Giapros V, Pantou K, Theocharis P, Challa A, Andronikou S. Serum transferrin receptor, ferritin, and reticulocyte maturity indices during the first year of life in ‘large’ preterm infants. Eur J Haematol 2007;79:439–46.
Van den Bruel A, Thompson MJ, Haj-Hassan T, et al. Diagnostic value of laboratory tests in identifying serious infections in febrile children: systematic review. BMJ 2011;342:d3082.
Acknowledgements
We thank the children and parents who participated in this study. We thank the staff of the neonatal departments of the Juliana Children’s Hospital, Medical Center Haaglanden, and Medical Center Alkmaar for their assistance including children for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Uijterschout, L., Domellöf, M., Berglund, S. et al. Serum hepcidin in infants born after 32 to 37 wk of gestational age. Pediatr Res 79, 608–613 (2016). https://doi.org/10.1038/pr.2015.258
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2015.258
This article is cited by
-
Growth and micronutrient status parameters of Nigerian preterm infants consuming preterm formula or breastmilk
Pediatric Research (2024)
-
Serum erythroferrone levels during the first month of life in premature infants
Journal of Perinatology (2022)
-
Hepcidin mediates hypoferremia and reduces the growth potential of bacteria in the immediate post-natal period in human neonates
Scientific Reports (2019)
-
Zinc protoporphyrin/heme ratio as parameter of iron status in moderately preterm infants: natural course and associations in the first 4 months
Journal of Perinatology (2017)